CASE REPORT
A case of classic Kaposi’s sarcoma masquerading as a vascular malformation
Howroyd LR,1 Milroy C,2 Ray S,3 Morgan R,1 Ratnam LA1
Abstract
A 45-year-old man presented with painful lumps on his right foot. Imaging suggested a vascular malformation and the patient was referred first to a vascular surgeon, then to a specialist vascular malformation centre. MRA and catheter angiography confirmed a high flow lesion. However, there was clinical and radiological suspicion that an alternative diagnosis was possible. Biopsy confirmed the lesions to be Kaposi’s sarcoma. Arteriovenous malformations and Kaposi’s sarcoma can appear almost identical clinically and radiologically, so histological analysis is important if there are any doubts about the diagnosis.
Case report
A 45-year-old man presented with a painful lump on his right foot, which had been slowly increasing in size over approximately 9 months and was interfering with his daily activities. He was a marathon runner and had stopped running due to the pain. There was no past medical or family history of note and he had never smoked. He was born in Tunisia and emigrated to the UK.
An ultrasound requested by the primary care doctor described an arteriovenous malformation (AVM) and he was referred to a vascular surgeon at a district general hospital, who found a lobulated subcutaneous mass including soft and fibrotic areas and attributed the pain to repeated thrombosis (Figure 1). He was recommended daily aspirin, an MRA of his foot was requested and he was referred to a specialised unit dealing in vascular malformations for consideration of sclerotherapy.

The MRA (Figure 2) showed distinct but communicating lesions with arterial supply and early venous drainage, suggestive of an arteriovenous lesion. A specialist multidisciplinary team (MDT), consisting of dermatology, vascular, diagnostic and interventional radiology experts, considered the lesions too high flow (ie, arterial) for sclerotherapy and recommended a diagnostic angiogram with a view to possible endovascular embolisation.
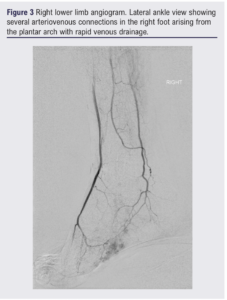
The diagnostic angiogram (Figure 3) showed abnormal feeding arteries and early venous pooling. Embolisation was not felt to be appropriate due to the high risk of resultant tissue loss and the case was rediscussed in the specialist MDT. Concerns were raised regarding the diagnosis as the lesions had multiplied and were felt to be disproportionally painful since the initial presentation. The decision was made to perform a biopsy prior to any further treatment. Microscopy showed spindle cells with mild atypia, scattered lymphocytes and extravasation of red blood cells. Staining with human herpes virus 8 (HHV8) was strongly positive. The biopsy was diagnostic of Kaposi’s sarcoma.

The patient was seen in an oncology clinic, now with multiple lumps on his foot and one on his shin. A viral panel showed he was HHV8 positive and HIV negative. A CT scan of his thorax, abdomen and pelvis showed no concerning lymph nodes or visceral lesions. Radiotherapy was not considered to be appropriate due to the number of lesions and the patient was commenced on a course of chemotherapy (pegylated liposomal doxorubicin). The patient completed eight cycles of chemotherapy but, unfortunately, he presented again 6 months later with new lesions in his foot for which he is currently being restaged.
Discussion
Vascular malformations encompass a wide spectrum of lesions. A fundamental radiological classification is whether the lesion is high or low flow,1 which can be further expanded based on flow dynamics and cellular features.2
AVMs are vascular malformations resulting from developmental defects of the arterial and venous vasculature. They affect any organ, most commonly the head and neck (specifically the most frequent are intracranial AVMs) followed by the extremities. The exact aetiology is unclear. To our knowledge, there are no published data regarding the incidence of peripheral AVMs. The incidence of intracranial AVMs is around 1–10/100,000.3-5
Although AVMs are thought to be present at birth, if they are deep or slow growing the patient may not present until adulthood. AVMs can be solitary or multifocal, and usually are slow growing but can grow rapidly. They often present with pain and swelling and can be red/blue/purple in colour.
Kaposi’s sarcoma is a low-grade vasoformative/ angioproliferative neoplasm (sarcoma is a misnomer) associated with HHV8, also known as Kaposi’s sarcoma-associated herpes virus (KSHV).6-8 There are four main subtypes of Kaposi’s sarcoma: classic, endemic (observed in sub-Saharan Africa), epidemic (AIDS related), and iatrogenic (transplant related).
Classic Kaposi’s sarcoma is what was originally described by Kaposi in 1872,9 a cutaneous tumour affecting primarily the skin over the lower legs and feet in a multifocal and classically symmetrical distribution. Kaposi’s sarcoma often occurs in older males of Mediterranean (such as Tunisian) or Central/Eastern European ancestry. It is likely multifactorial with one factor being that HHV8 infection rates are substantially higher in these parts of the world.10-12 Additionally, it is thought that people with classic Kaposi’s sarcoma are born with a genetic/immunological vulnerability to the HHV8 virus.6,7,13,14 Transmission routes of HHV8 are not fully understood, but both vertical and horizontal transmission are established and it is thought to be via bodily fluids including saliva.8,15
The incidence rate of classic Kaposi’s sarcoma in the UK is thought to be around 0.014/100,000 person-years.16 However, in Sardinia the incidence rate was estimated at 1.58/100000 person-years.17
Classic Kaposi’s sarcoma is characterised by the appearance of purplish, reddish blue or dark brown/black macules, plaques and nodules on the skin. The lesions vary from very small to several centimetres in diameter. They can remain unchanged for months to years or may grow rapidly and can be accompanied by contemporaneous mucous membrane and visceral lesions.
It is well established that the cutaneous manifestation of Kaposi’s sarcoma and an AVM can be similar.18-22 Most cases reported in the literature are of ‘pseudo-Kaposi’s sarcoma’, also eponymously called Stewart–Bluefarb syndrome, where the patient is initially thought to have classic Kaposi’s sarcoma and it is discovered to be an AVM. Indeed, to our knowledge there is only one case report describing a case of Kaposi’s sarcoma which was initially thought to represent an AVM.21 It is unusual for these cases to be presented in vascular journals and therefore vascular clinicians may not be aware of this diagnostic pitfall.
This case report serves to highlight to those involved in the patient’s journey that these two conditions can be almost indistinguishable both clinically and radiologically. If there is any uncertainty in the history, examination or imaging, then a biopsy and histopathological analysis should be obtained prior to any definitive treatment. The treatment of the two conditions is very different and diagnostic delay can have detrimental consequences for the patient.

Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;Online ahead of publication
Publication date:
May 1, 2024
Author Affiliations:
1. Department of Radiology, St George’s University Hospital NHS Foundation Trust, London, UK
2. Department of Plastic Surgery, St George’s University Hospital NHS Foundation Trust, London, UK
3. Department of Vascular Surgery, Kingston Hospital NHS Foundation Trust, Galsworthy Road, Kingston upon Thames, UK
Corresponding author:
Lucy-Rose Howroyd
Department of Radiology, St George’s University Hospital NHS Foundation Trust, London SW17 0QT, UK
Email: rose.howroyd@ stgeorges.nhs.uk











