CASE REPORT
Ectopic thyroid tissue presenting as a carotid body paraganglioma
Fabre I,1 Christian A,2 Rees A,3 Bosanquet DC1,2
Abstract
Ectopic thyroid tissue is a rare developmental abnormality, typically presenting with midline ectopia due to incomplete embryological migration via the thyroglossal duct. The presence of ectopic thyroid tissue lateral to the midline is very rare, accounting for 1–3% of all ectopic thyroid tissue. Clinically, these lesions are often mistaken for other diagnoses including enlarged lymph nodes or metastatic tumours. We present a case of lateral ectopic thyroid tissue presenting as a presumed carotid body paraganglioma in a middle-aged woman. The patient presented with a slow-growing lateral neck mass which was clinically and radiologically consistent with a carotid body paraganglioma. She subsequently underwent tumour excision after which histological analysis identified ectopic thyroid tissue with no evidence of malignancy.
Background
Embryologically, the thyroid gland begins development at the third week of gestation.1 It is derived from the fusion of a large median anlage and two lateral anlages. The median anlage, which produces the follicular cells (making up the majority of the thyroid parenchyma), arises first as an endodermal growth from the second pharyngeal arch.2 This growth is known as the thyroid diverticulum. The thyroid diverticulum then descends caudally down the midline until the eighth gestational week when it reaches its final destination, sitting anterior to the trachea and larynx.3 This line of migration is known as the thyroglossal duct. The two lateral anlages, which produce the parafollicular C cells, are derived from the fourth pharyngeal pouch. They migrate to fuse with the posterior surface of the median anlage during its descent in the fifth week of gestation.2,4
In contrast, the carotid body, which sits within the adventitial layer of the carotid bifurcation, is derived from the mesoderm of the third pharyngeal arch and the neural crest ectoderm. Tumours of the carotid body arise from the paraganglioma cells. There is no known relationship between the carotid body and the thyroid gland.5
Ectopic thyroid tissue (ETT), defined as thyroid tissue not located anterolaterally to the second to fourth tracheal cartilages,6 was first described by Hickman in 1869 when a newborn suffocated as a result of a lingual thyroid causing upper airway obstruction.7 Since then, multiple cases of ETT have been reported. Typically, as with Hickman’s case, the ETT is found in the midline due to incomplete descent of the median anlage. The presence of ETT lateral to the midline is rare, likely due to dysembryogenesis in the migration of the lateral anlage.4 Due to their rarity, these are often clinically misdiagnosed as enlarged lymph nodes, metastatic tumours8 or, as in our case, carotid body paragangliomas. Even with modern imaging it can be difficult to differentiate ETT from other pathology such as carotid body paraganglioma and therefore many are only diagnosed after surgical excision and histological analysis.9
Case presentation
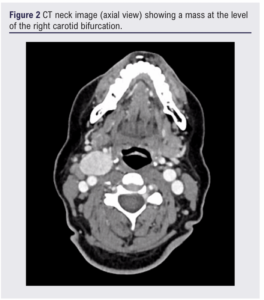
A woman in her 50s presented with a right-sided lateral neck mass which had been present for a few months and was associated with mild discomfort, but no disturbance to speech or swallowing and no symptoms of thyrotoxicosis. Examination revealed a solitary firm mass in the right anterior triangle with no overlying skin changes and no lymphadenopathy, consistent with a provisional clinical diagnosis of carotid body paraganglioma. An ultrasound scan (Figure 1) of the neck identified a well-defined hyperechoic mass at the right carotid bifurcation, and a subsequent CT scan (Figures 2 and 3) revealed a 51 mm hyper-enhancing mass straddling the carotid bifurcation, sitting 17 mm inferior to the skull base, described as consistent with a carotid body tumour. There was no evidence of any pathological lymphadenopathy and the upper aerodigestive tract appeared normal. The presence of a thyroid gland in the normal orthotopic position was also noted. Based on these findings, the mass was initially diagnosed as a carotid body paraganglioma and the patient was scheduled for endovascular embolisation followed by surgical resection. All pre-procedure haematological and biochemical investigations were normal. Previous thyroid function tests were within normal ranges.


During the endovascular embolisation the angiogram showed modest hypervascularity relating to the mass. The three largest feeder vessels were embolised and this resulted in a 70–80% reduction in the lesion’s ‘blush’.
Intraoperatively, the tumour was encountered at the level of the carotid bifurcation and complete excision was performed. The tumour encased the carotid arteries but was easily resectable, with no invasion of the adventitia. An enlarged jugulodigastric lymph node lying superficial to the tumour was also excised.
Histological analysis showed lobulated thyroid with marked necrosis and haemorrhage, in keeping with embolisation. There were no features to suggest malignancy from the primary lesion or lymph node. The final diagnosis of ETT was made.
During the initial postoperative period the patient developed left arm weakness. This was initially investigated and treated as a potential cerebrovascular accident; however, a CT and MRI showed no evidence of any infarct. There were no further concerns from the vascular team prior to discharge. The total length of stay was 10 days.
Follow-up at four weeks confirmed the patient was recovering well, with no further neurological symptoms and recovery of most of her arm function. The wound had healed well and there were no symptoms of hypothyroidism and thyroid function tests were normal.
Discussion
ETT is a rare embryological abnormality with a prevalence of 1/100,000–300,000.1 Typically, it occurs along the median path of migration as a lingual thyroid (80–90% of cases) or thyroglossal cyst (5–15% of cases) secondary to incomplete descent or obliteration of the thyroglossal duct.4 Ectopic tissue lateral to the midline is rare, accounting for only 1–3% of all ETT. The most accepted hypothesis for its development is failure of the lateral anlage to fuse with the medial anlage and non-migration of the gland.4,5,10 Mutations in a number of transcription factors (NKX2-1, PAX8, FOXE1 and TSHR) associated with definition and migration of the developing thyroid are recognised causes of thyroid dysgenesis.11 These are often tested for in patients with congenital hypothyroidism, which is associated with thyroid dysgenesis and ectopy. However, previous biochemistry showed our patient to be euthyroid and therefore this was not examined.
Where reported, 70% of lateral ETT are located in the submandibular region or, less commonly, near the carotid sheath.4 There have been only six previously reported cases of ETT at the carotid bifurcation.5,9,12-15 Other unusual locations of ETT include the mediastinum, chest and abdomen.12
The clinical presentation of our patient was similar to those in previously reported cases – namely, a slow-growing asymptomatic mass. However, on retrospective review it was noted that our patient’s preoperative CT scan identified a thyroid gland located in the normal orthotopic position. In cases of lateral ETT, only 41% have also had a thyroid gland in the normal orthotopic position. However, it is noteworthy that a further 24% had another site of thyroid tissue located elsewhere such as a lingual thyroid. In comparison, a second site of thyroid tissue was seen in only 25% of those with ectopic lingual thyroids.4
Given this, it is important to consider the functional effects when excising ETT. It has been reported that, in 70–80% of cases, ETT may be the only functional tissue5 and therefore excision can lead to irreversible hypothyroidism. This was not the case in this instance. The simultaneous finding of lateral ETT and a normally located functional thyroid gland is extremely rare.5,16
Even with modern imaging techniques it can be difficult to discriminate lateral ETT from other diagnoses including carotid body tumours, and therefore management is often via first-line excision biopsy. Consequently, ETT is often only diagnosed after histological analysis.4,9 When ETT is suspected, technetium-99 or iodine-131 scintigraphy are not only important diagnostic investigations but may also demonstrate the presence or absence of normally located or other functional thyroid tissue.4,16 Somatostatin receptor scintigraphy such as octreotide scans or 68Ga-DOTATATE PET scans are often used to diagnose neuroendocrine tumours, including paragangliomas. However, uptake of octreotide and 68Ga-DOTATATE within thyroid goitres, and in a case of ETT, has also been reported.12,17
Albeit rare, ETT is an important differential to consider given the risk of irreversible hypothyroidism. Others have highlighted the importance of combined investigations such as CT, MRI, scintigraphy (somatostatin receptor, technetium-99 or iodine-131) and fine needle aspiration cytology to give a higher sensitivity and specificity when investigating a lateral anterior triangle neck mass.4,12,16

Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;Online ahead of publication
Publication date:
May 1, 2024
Author Affiliations:
1. Aneurin Bevan University Health Board, UK
2. Cardiff and Vale University Health Board, UK
3. Neuroscience and Mental Health Innovation Institute, Cardiff University, UK
Corresponding author:
Ismay Fabre
The Vascular Institute, Royal Gwent Hospital, Cardiff Road, Newport NP20 2UB, UK
Email: Ismay.Fabre3@ wales.nhs.uk











