ORIGINAL RESEARCH
A quality improvement project on operative records
Soh V,1 Mowlood C,1 Yuen Eow S,1 Donnelly C,1 Dow E,1 Reid J,1 Elbaroni W,2 Healy D1
Plain English Summary
Why we undertook the work: Clear and accurate notes taken during surgery are vital for providing patients’ postoperative care and for legal purposes. The Royal College of Surgeons of England (RCSEng) stresses the importance of good documentation in medical practice to provide the highest level of patient care. To improve the quality of our surgical notes, we conducted an assessment and introduced an electronic system to replace handwritten notes. This change was prompted by issues like missing records, hard-to-read handwriting and incomplete instructions, which caused challenges for our nursing staff and doctors.
What we did: We conducted a review of our surgery records to improve their quality.
In the first review we checked records over specific periods and used a standard guideline for what should be included. To make things better, we talked to colleagues, put up posters and sent reminder emails. We then assessed our operative records after our interventions. In the second review we worked on an electronic template to replace handwritten notes. We made some changes based on feedback from surgeons and eventually implemented the electronic system for all.
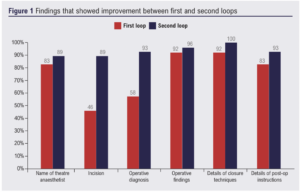
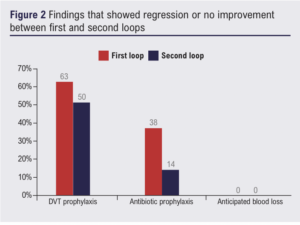
What we found: In the first review we looked at 24 surgical notes before the intervention and 28 surgical notes after the intervention. We discovered that some important information was missing, such as the name of the anaesthetist, surgical findings and postoperative instructions. After making changes, there were improvements in the quality of the surgical notes. The description of the incision increased by 43%, specifying the diagnosis improved by 35%, and closure technique description improved by 8%. Postoperative instructions also got better by 10%. However, there are areas where we still need to work on documenting, such as postoperative venous thromboembolism instructions. In the second review we were able to create an electronic note template through multiple loops of feedback from other vascular surgeons in our unit. However, some surgeons found it challenging to use due to computer access and printing issues. We are currently working on improving access and encouraging everyone to embrace the benefits of electronic records.
What this means: We observed positive changes within our vascular unit through the implementation of a system for electronic operative records. More quality improvement projects should be done in the future to ensure compliance and improvement in the quality of the operative records and the barriers faced in this study have been solved.
Abstract
Introduction: In 2013 the Royal College of Surgeons of England (RCSEng) published a Standard of Good Practice for surgeons to adhere to in the UK. The guideline included the importance of legible documentation and what should be included in the operative notes. We conducted an audit and quality improvement project in our regional vascular unit in Northern Ireland which showed multiple elements of our operative records that could be improved, such as the documentation of deep vein thrombosis prophylaxis, antibiotic prophylaxis and the use of electronic operative records.
Methods: We organised an audit between 3rd and 16th October 2022 where operative notes were collected consecutively and analysed. Multifaceted interventions such as discussion with colleagues, reminder emails and the placement of guidelines around the vascular theatres were done. The second loop of audit was completed between 7th and 20th November 2022. After the audit, we underwent four cycles of Plan-Do-Study-Act (PDSA) where we designed and developed an electronic operative note template and linked it to our electronic records system within the Trust.
Results: A total of 24 and 28 operative records were collected, respectively, in the first and second loop of the audit. The majority of the domain showed improvement after the multifaceted interventions: for instance, the documentation of incision (from 46% to 89%), operative diagnosis (from 58% to 93%) and details of closure technique (from 92% to 100%). Through our PDSA cycles, an electronic operative note template was created and improved via feedback from the vascular surgeons. Logistic and IT issues were addressed and we are currently in the process of increasing the number of computers and printers around the vascular theatres. The Vascular Surgical Unit is currently slowly adapting to the use of electronic operative records.
Conclusion: Our work has improved the compliance of operative records with the RCSEng guideline and increased the use of electronic operative notes, which are more accessible and legible for our multidisciplinary team.
Background
Accurate and legible operative notes are critical for providing high-quality postoperative care and they also serve a crucial role for medicolegal disputes.1,2 The General Medical Council (GMC) has emphasised the importance of good documentation as part of good medical practice.3 Additionally, the Royal College of Surgeons of England (RCSEng) has developed a guideline that contains recommendations on the content of operative notes and also encourages the use of electronic operative notes.4 Various quality improvement studies have been done to evaluate the compliance and quality of operative notes with the RCSEng guideline, and there have been positive changes in their respective units.1,5,6 The Vascular Surgical Unit in Northern Ireland is a tertiary centre with 10 vascular surgeons. In the unit, hand-written operative notes have traditionally been used. However, issues such as missing records, illegible handwriting and incomplete postoperative instructions have been reported, posing significant challenges to the nursing staff and doctors in our unit.
We aimed to evaluate and improve the quality of our operative notes by doing a closed loop audit. We also aimed to establish an electronic system for operative notes through the process of quality improvement via Plan-Do-Study-Act (PDSA) cycles.
Methods
Audit
In the closed loop audit study, the baseline measurements included the adherence to RCSEng guidelines on operative notes,4 listed below:
• Date and time Elective/emergency procedure
• Names of the operating surgeon and assistant
• Name of the theatre anaesthetist
• Operative procedure carried out
• Incision
• Operative diagnosis
• Operative findings
• Any problems/complications
• Any extra procedure performed and the reason why it was performed
• Details of tissue removed, added or altered
• Identification of any prosthesis used, including the serial numbers of prostheses and other implanted materials
• Details of closure technique
• Anticipated blood loss
• Antibiotic prophylaxis (where applicable)
• Deep vein thrombosis prophylaxis (where applicable)
• Detailed postoperative care instructions
• Signature
A closed loop audit on the quality of our operative records was initially done from 3rd to 16th October 2022 and from 7th to 20th November 2022. We based the standard on the RCSEng guideline, which specified 18 elements that should be included in each operation note. For the first audit cycle we collected data over two weeks before implementing our intervention. The interventions included formal discussions with colleagues to highlight the RCSEng standard, placing posters in each of the operating theatres and sending a reminder to all of our department members via email. A further two-week period of data collection closed the audit loop.
Quality Improvement Project
We also conducted a quality improvement project that began on 21st November 2022 using the PDSA system. Each PDSA cycle was trialled for a month.
PDSA Cycle 1
Two of the 10 vascular surgeons used an electronic operative note template that was accessible via our local “Patient Centre” software system. After a month, the surgeons gave feedback regarding the ergonomics and accessibility of the electronic note template. Software problems and ergonomic issues with the template were highlighted and it was decided to change software and modify the template.
PDSA Cycle 2
A new template was designed with the help of the Urology Department which provided us with their electronic operative notes for reference. The new template could be saved as a PDF file and directly uploaded to our more modern intranet-based Northern Ireland Electronic Care Record (NIECR) system. Two surgeons evaluated this system for a month and felt that it was effective. We proceeded to roll it out to the whole unit.
PDSA Cycle 3
The remaining eight vascular surgeons in the unit gave feedback on the content of the template and amendments were made to it. The revised electronic template was made available to all surgeons in our unit and it became the recommended method of creating operative notes; however, compliance with the new system remained a challenge. The barriers to compliance were mainly the prolonged time needed to type and a lack of computers and printers within the operating theatres.
PDSA Cycle 4
This cycle is currently underway and involves enhancing access to computers and printers by liaising with the IT department and continually emphasising the benefits of electronic records to our colleagues in order to enhance compliance.
Results
A total of 24 and 28 operative records were collected, respectively, in the first and second loops of the audit. The first loop audit study showed all operative notes contained date and time, names of surgeons, details of operative procedure, descriptions of tissue removed, identification of prosthetics, and surgeon’s signature. After the intervention, several areas showed improvement. There was a 6% increase in the documentation of the name of the anaesthetist (from 83% to 89%), a 43% increase in the description of the incision (from 46% to 89%), a 35% increase in specifying the operative diagnosis (58% to 93%), a 4% increase in operative findings, an 8% increase in closure technique description (from 92% to 100%) and a 10% increase in the documentation of postoperative instructions (from 83% to 93%) (Figure 1). There was a decrease in deep vein thrombosis and antibiotic prophylaxis documentation of 13% (from 63% to 50%) and 24% (from 38% to 14%), respectively (Figure 2). There was no documentation of anticipated blood loss in either cycle. No operative notes were fully compliant with the RCSEng guideline in either loops. We measured the proportion of completed domains out of the 18 elements included in the RCSEng guideline, gave each operative note a score and calculated the average score for each loop. There was an improvement in the mean operative note score after the intervention from 61% (11/18) to 66% (12/18) (Table 1).

In our quality improvement project we have been able to establish an electronic operative note system effectively and responsibly by using the PDSA system. The vascular surgeons in our unit have provided positive feedback during our monthly clinical governance meeting regarding the latest version of the electronic operative notes.
Discussion
The aim of this study is to improve the quality of operative notes according to the RCSEng guideline. Our initial audit showed there was poor documentation and compliance with various elements of the RCSEng guideline, such as incision type and operative diagnosis. The multi-faceted intervention between the first and second loops improved compliance with the RCSEng guideline, where documentation of operative diagnosis and closure techniques was 58% and 92%, respectively, pre-intervention and 93% and 100%, respectively, post-intervention. Furthermore, we designed and continuously update the new electronic operative notes through feedback from other vascular surgeons. Integrating the template to the local NIECR system allowed better access to operative notes for other healthcare colleagues such as general practitioners and nursing staff. The limitation of this study is the short time period of data collection and PDSA cycle, and a further quality improvement project should be repeated to assess compliance of the new electronic operative notes with the RCSEng guideline. There are still barriers to using our electronic operation note system including inadequate access to computers and printers in theatres. The latest version of the electronic template is in use and we are liaising with our IT department to provide more computers near the vascular theatres.
Conclusion
Our work has improved accessibility and legibility of operation notes for nursing and medical staff. We have met the aim of this study to improve compliance and record keeping of operative notes. More quality improvement projects should be done in the future to ensure compliance and quality of the operative records improves and the barriers faced in this study have been solved.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023; 3(1): 32-35
Publication date:
November 16, 2023
Author Affiliations:
1. Department of Vascular Surgery, Belfast Health and Social Care Trust, Belfast, UK
2. Department of Urology, Belfast Health and Social Care Trust, Belfast, UK
Corresponding author:
Vernie Soh
Royal Victoria Hospital,
274 Grosvenor Road, Belfast BT12 6BA, UK
Email: VernieWenYee.Soh@ southerntrust.hscni.net











