CASE REPORT
A rare congenital abnormality mimicking the appearance of a type A aortic dissection
Ahmed-Issap A,1 Adem A,1 Magee D,2 Nanjaiah P,1 Wells D3
Abstract
Type A aortic dissection is a tear in the wall of the ascending aorta and/or arch between the tunica intima and tunica media layers. This is a surgical emergency and requires immediate surgical repair. Aortic CT angiography is essential for classification, assessing extent of the disease and planning the management. An intimal flap on CT is characteristic of the pathology. We present a case where a fibrous cord, presumed to be a congenital remnant, mimicked the appearance of an intimal flap but was not an aortic dissection.
Introduction
Aortic dissections are caused by a tear in the tunica intima of the aortic wall allowing blood to enter a new ‘false lumen’ created between the tunica intima and tunica media. Stanford type A aortic dissections involve the ascending aorta and/or arch. Type A aortic dissections are classified as a surgical emergency and require immediate repair by a cardiothoracic surgeon.
Type A aortic dissections classically present as a sudden ‘excruciating tearing chest pain radiating to the back’. There may be a significant difference in blood pressure and pulses in both arms. Modifiable risk factors that may increase the event of a type A aortic dissection including smoking, hypertension, recreational drug use and dyslipidaemia. Genetic abnormalities that may put an individual at an increased risk of developing the disease include a congenital defect to the aortic valve such as a bicuspid aortic valve causing a dissection of the ascending aorta or connective tissue disorders such as Marfan’s, Ehlers-Danlos or Loeys-Dietz syndromes.
Imaging of a suspected aortic dissection is essential for diagnosis, classification and planning management. The gold standard imaging modality for aortic dissection is aortic CT angiography (CTA). Typical CTA findings include an intimal flap, double lumen, dilatation of the aorta and intramural haematoma. An intimal flap is pathognomonic of the condition. However, one must be cautious when considering this sign as it may not always indicate an aortic dissection.1 We present a rare case of a fibrous cord in the ascending aorta mimicking an intimal flap.
Case presentation
A 66-year-old man presented to the Emergency Department of a tertiary hospital with two episodes of losing his balance after standing or walking for a prolonged period. He also reported chest pain with no radiation, worse with deep inspiration, and pallor. He denied dyspnoea, sweating, cough or palpitations. His past medical history included frequent light-headed episodes on standing, falls, vacant episodes, schizophrenia, depression, angina, diabetes mellitus, hyperthyroidism, asthma and hypertension. His social history included current smoker (rolling tobacco cigarettes, 11 pack/year history), infrequent alcohol drinker and communication through British Sign Language as he was born deaf. He lived at a residential home.
On examination he was severely hypotensive (61/39 mmHg) with the paramedics with a heart rate of 65 beats per minute (bpm). On attendance at the Emergency Department his blood pressure returned to normal (107/58 mmHg) but his heart rate was 48 bpm and irregular. Lungs were clear on auscultation but a new ejection-systolic murmur was noted. Twelve-lead ECG demonstrated bradyarrhythmia with no prolonged PR interval or heart block. Blood tests showed mild renal impairment (eGFR 68 mL/min/1.73 m2) and C-reactive protein 19.4 mg/L.
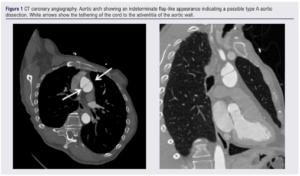
During his admission, further investigations to find a cause of his dizziness included a head CT scan which was negative, a 24-hour cardiac tape which showed sinus rhythm with episodes of bradycardia, and a transthoracic cardiac echo which showed an ejection fraction of >50% but was unable to assess the aortic valve for aortic stenosis. A respiratory infection was diagnosed clinically and antibiotics were started. Due to the inability to assess the aortic valve on cardiac echo, a CT coronary angiogram (CTCA) was requested. The CTCA showed an aortic valve calcium score of 514 (non-severe aortic stenosis2), normal coronary arteries with right dominance and an indeterminate flap-like appearance of the aortic arch was noted with no associated haematoma (Figure 1).
Subsequent CTA did not show a double lumen but did highlight a cord-like structure that was 27 mm in length and 1.8 mm in diameter. This structure was tethered to the adventitia of the aortic wall and traversed to the opposite wall in a characteristic position (Figure 1).
Discussion
Type A aortic dissections are classified as a surgical emergency and, once identified, patients should be transferred immediately to theatre. Without repair, mortality increases by 10% per hour. CTA is the gold standard for assessing the presence of aortic dissection as it has a sensitivity and specificity approaching 100%, so should be undertaken in all patients with a strong clinical suspicion. Classic features of aortic dissection on CTA include intimal flap, double lumen, dilatation of the aorta and intramural haematoma.3 In this case, an ‘intimal flap’ was seen on one CTA slice but no double lumen, intramural haematoma or aortic dilatation.
Only one previous case of a cord-like structure on imaging like this has been reported.1 These authors presented an asymptomatic patient with an intraluminal line in the distal ascending aorta on CTA and MRI which remained unchanged on imaging over the next five years. They theorised that this was a congenital remnant forming a fibrous cord in the aorta.
The aorta develops in the first few weeks of fetal life from the truncus arteriosus arising from the primitive heart and divides into six paired pharyngeal aortic arches.4 The fourth arch forms the right brachiocephalic and both subclavian arteries. The aortic arch proper then joins with the descending aorta. The first, second and fifth arches regress whilst the third arch forms the carotid arteries. Abnormal persistence or obliteration of the various arches may lead to anatomical variations which can cause longstanding consequences that may require surgical repair or form congenital abnormalities. Guo et al proposed that the congenital intraluminal structure was an incomplete formation then rapid regression of a persistent fifth aortic arch (PFAA).1
We also found a cord-like structure like Guo et al but in the aortic arch rather than the ascending aorta. Like Guo et al, we also consider that this cord may be a remnant of the fifth aortic arch as the formation of the cord-like structure.
Conclusion
Type A aortic dissection is a surgical emergency diagnosed with a combination of clinical and radiological findings. Rare benign pathologies identified on imaging such as a fibrous cord may mimic a dissection and this is important to recognise, especially when the clinical situation does not correlate with the imaging. An opinion from a vascular radiologist in these circumstances can reduce the follow-up surveillance scans, radiation burden and anxiety for the patient.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(3):160-162
Publication date:
May 17, 2024
Author Affiliations:
1. Department of Cardiothoracic Surgery, Royal Stoke Hospital, University Hospitals of North Midlands NHS Trust, Stoke-on-Trent, UK
2. Keele University School of Medicine, Keele University, Staffordshire, UK
3. Department of Interventional Radiology, Royal Stoke Hospital, University Hospitals of North Midlands NHS Trust, Stoke-on-Trent, UK
Corresponding author:
Amber Ahmed-Issap
Department of Cardiothoracic Surgery, Royal Stoke Hospital, University Hospitals of North Midlands NHS Trust, Newcastle Road, Stoke-on-Trent ST4 6QG, UK
Email: amber.ahmed-issap@ uhnm.nhs.uk











