ORIGINAL RESEARCH
Ambulatory vascular clinics provide a safe and effective pathway for management of chronic limb threatening ischaemia
Sivaharan A,1 Williams T,1 Ng C,1 Nixon R,1 Green M,1 Benton L,1 O’Shea S,1 Prouse S,1 Bell R,1 Patel A,1 Patel S,1 Thulasidasan N,1 Partridge J,1 Sandford B1
Plain English Summary
Why we undertook the work: The management of patients with diseased blood vessels in the lower limbs severely reducing blood supply resulting in pain at rest and ulcers is challenging.
What we did: We looked back at the outcomes of patients who attended the Guy’s and St Thomas’ (GSTT) Emergency Vascular Clinic (EVC). We used electronic hospital records to gather information about each patient who attended the EVC from 31 July 2017 to 19 April 2021 and documented their outcome after treatment.
What we found: We found that the GSTT’s EVC service provides a safe and effective model of care for the management of this frequently complex and frail group of patients.
What this means: Further national research is needed to see whether this ambulatory EVC model can be used in other vascular units across the country.
Abstract
Introduction: The management of chronic limb threatening ischaemia (CLTI) has changed rapidly over recent years. The outcomes of lower limb revascularisation, despite improvements since centralisation, remain poor. Ambulatory emergency care has emerged in several surgical subspecialties as the optimal pathway to ensure timely access to specialist services whilst avoiding unnecessary urgent hospital admission and lengthy inpatient stays. This study aims to describe the outcomes of such a service for those with CLTI.
Methods: This study includes all patients with suspected CLTI presenting to the Guy’s and St Thomas’ (GSTT) Emergency Vascular Clinic (EVC) between 31 July 2017 and 19 April 2021. Demographic, clinical and admission data were gathered from a prospectively maintained database. Operative details, in hospital and mid-term outcomes were gathered retrospectively from electronic hospital records. Frailty data were calculated using the Edmonton Frailty Scoring (EFS) System.
Results: There were 799 encounters at the EVC for suspected CLTI. 375 (46.9%) of these encounters resulted in a confirmed diagnosis of CLTI and admission, either the same day as an emergency (187 (23.4%)) or as a planned urgent admission (188 (23.5%)). Time from referral to EVC review was a median of 1 day (interquartile range (IQR) 1–3 days) and median time from EVC review to revascularisation or amputation (in cases where this was the primary treatment strategy) was 8 days (IQR 4–16 days). Median time to admission was 1 day (IQR 0–13 days and length of stay was a median of 7 days (IQR 2–15 days). Amputation-free survival (AFS) from the first patient encounter (with presentations for each leg taken separately) was 95% at one month and 78% at one year. Overall survival was 98% at one month and 84% at one year. Frailty was significantly associated with mortality (p=0.03), but not AFS (p=0.085).
Conclusion: These data suggest that an EVC pathway provides a safe method of treating CLTI with minimal delays to urgent planned admission, revascularisation and AFS, in keeping with nationally reported data.
Introduction
The management of chronic limb threatening ischaemia (CLTI) has changed rapidly over recent years, both due to the newer technologies in the realm of endovascular surgery1 and the current model of centralising vascular services.2 The outcomes of lower limb revascularisation, however, remain fairly poor, with a recent randomised controlled trial showing a 33–37% mortality in those CLTI patients undergoing surgery.3 The Global Vascular Guidelines4 recommend specialist vascular limb salvage services in order to reduce adverse outcomes in this group.5
The Peripheral Arterial Disease Quality Improvement Framework by the Vascular Society of Great Britain and Ireland (VSGBI) supports this approach, recommending timely access to intervention for CLTI (5 days for inpatients and 14 days for outpatients).6 However, only a minority of vascular centres currently provide outpatient facilities within 7 days of referral and less than a third of vascular surgeons think that a 14-day referral to treatment pathway is feasible for patients who are not admitted to hospital.7
Ambulatory emergency care has emerged in several surgical subspecialties over recent years as the optimal pathway to ensure timely access to specialist services whilst avoiding unnecessary urgent hospital admission and lengthy inpatient stays. Evidence from general surgery demonstrates that ambulatory emergency care is associated with decreased length of inpatient stay, expedited clinical decision making and improved financial efficiency when managing emergency surgical patients.8 Urgent one stop outpatient clinics for emergencies have also been demonstrated to reduce acute admission.9,10 However, adverse outcomes have been reported with ambulatory general surgery associated with frail patients, with frailty rather than age being associated with an increased risk of complications after surgery.11
Vascular surgery has always presented a unique challenge, with a multi-morbid and frail patient group.12 Ambulatory emergency ‘hot clinics’ are now established in several UK arterial hub centres and reported benefits for vascular patients include decreased length of stay with no difference in time to procedure, return to theatre or 30-day readmission.13 Similarly to general surgery services, financial efficiencies related to decreased hospital stay have also been reported. It is well recognised that elderly frail patients become deconditioned rapidly during in-hospital stays, and there is some evidence that an ambulatory patient pathway may benefit outcomes, both in terms of reduction in frailty14 and also in reduced rate of major limb amputation.15
The Guy’s and St Thomas’ (GSTT) NHS Trust Emergency Vascular Clinic (EVC) was established in 2018 after a pilot project in 2017 proved to be a safe and effective service. This study describes the outcomes of this clinic service for those with CLTI.
Methods
This observational cohort study includes all patients with suspected CLTI (defined as ischaemic rest pain or tissue loss persisting for more than 2 weeks)4 presenting to the GSTT EVC between 31 July 2017 and 19 April 2021. All patients were referred urgently via the on-call vascular registrar or a consultant vascular surgeon and deemed appropriate for an EVC pathway after further triage by the EVC team. Referrals were accepted from networked hospitals, podiatrists and clinical nurse specialists.
The EVC is a daily clinic, active from Monday to Friday. All patients were assessed by a clinical nurse specialist with additional qualifications in patient assessment and prescribing. Following history and examination, laboratory tests, ankle brachial pressure index and imaging (duplex ultrasound scans and/or CT angiography) were arranged and reviewed the same day. Photographs were taken and uploaded onto the electronic patient record if appropriate. Patients were then reviewed along with their investigations by a consultant vascular surgeon and a management plan made. In some cases, a referral for Comprehensive Geriatric Assessment (CGA) by the Perioperative medicine for Older People Undergoing Surgery (POPS) team was arranged prior to hospital admission, and where possible on the same day as the EVC appointment. This service is thus far limited to those undergoing major revascularisation procedures or with significant multimorbidity/functional limitations.
Demographic, clinical and admission data were gathered from a prospectively maintained database. This database covers the time until definitive treatment or decision for conservative management, therefore operative details, in-hospital and mid-term outcomes (including complications) were gathered retrospectively from electronic hospital records. Frailty data were calculated using the Edmonton Frailty Scoring (EFS) System, with a score of <3, 4–5, 6–7, 8–9 and >10 indicating no frailty, vulnerable, mild, moderate, or severe frailty, respectively.16 This was documented as part of the CGA.
Data were stored in a password-protected anonymised database. The study was registered as an audit within the Trust and all data were pseudo-anonymised under institutional governance obviating the need for ethical approval.
Statistical analysis was performed using R v4.2.2 (R Foundation for Statistical Computing, Vienna, Austria). The first part of the analysis was performed on all encounters leading to an emergency or planned admission. The second part of the analysis, pertaining to frailty, survival, and amputation-free survival (AFS), was performed from the first encounter for each patient, per leg (thereby removing patients who represented unless they did so for the opposite leg).
Descriptive analysis was done using the mean for parametric data and the median for non-parametric data, reporting interquartile ranges (IQR) where appropriate. Testing for normality was undertaken using the Shapiro–Wilk test. Proportional testing for complication rates based on primary management was undertaken using the χ2 test. Kaplan–Meier curves were generated to demonstrate overall survival and AFS and, where this was done to compare by frailty severity, Cox regression was performed with the log-rank test reported. We used a two-sided α level of 0.05.
Results
There were 799 consecutive encounters at the EVC for suspected CLTI between 31 July 2017 and 19 April 2021. Figure 1 summarises the inclusion flowchart for the subsequent data analyses.
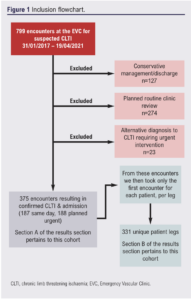
Results by encounters
During this time frame, 375 (46.9%) of these encounters resulted in a confirmed diagnosis of CLTI and admission, either the same day as an emergency (187 (23.4%)) or as a planned urgent admission (188 (23.5%)). Other outcomes after EVC included conservative management and discharge (127 (15.9%)), planned clinical review in routine OPD (274 (34.3%)), or an alternative diagnosis to CLTI (23 (2.9%)).
With respect to the 375 encounters that resulted in admission, 130 were for ischaemic rest pain (Rutherford 4 (34.7%)), 203 for ischaemic ulceration (Rutherford 5 (54.1%)) and 42 for tissue necrosis (Rutherford 6 (11.2%)).
Median time from referral to EVC review was 1 day (IQR 1–3 days) and median time from EVC review to revascularisation or amputation (in cases where this was the primary treatment strategy) was 8 days (IQR 4–16 days). Median time to admission was 1 day (IQR 0–13 days, and length of stay was a median of 7 days (IQR 2–15 days). Median follow-up was up to 9.9 months (IQR 3.4–18.8). When taking only those who were admitted the same day, median time from EVC review to intervention was 5 days (IQR 2–8 days).
Of the 375 encounters resulting in an admission, 63 (16.8%) underwent conservative management, 180 (48.0%) undrwent endovascular revascularisation as the primary procedure, 48 (12.8%) underwent hybrid revascularisation, 54 (14.4%) underwent open surgery, 9 (2.4%) underwent primary major lower limb amputation (MLLA) and 20 (5.3%) underwent minor procedures. The 30-day readmission rate was 69 (18.6%) and 90-day readmission rate was 85 (22.9%).
Complications were experienced in 68 admissions (18.1%), including 15 (4.0%) respiratory complications, 17 (4.5%) wound complications, 8 (2.1%) cardiac complications (including acute coronary syndromes and tachyarrhythmias) and five (1.3%) patients with acute kidney injury. When comparing the complication rate of different primary treatment modalities, there were no significant differences in cardiac (p=0.50), respiratory (p=0.64), renal (p=0.51) or wound complications (p=0.97).
Results by unique patients/legs
This group included 331 unique patient legs (mean (SD) age 70.8 (11.9) years), 217 (65.6%) male, 114 (34.4%) female). AFS was 95% at one month and 78% at one year (Figure 2A) and survival was 98% at one month and 84% at one year (Figure 2B) per unique patient leg.

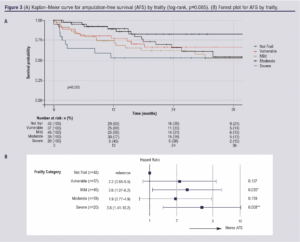
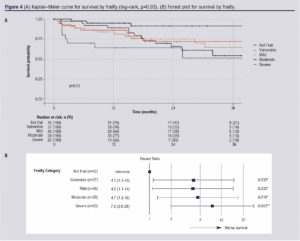
Frailty data for those who were admitted following EVC review were available for 183 patients; 148 patients had missing data points. Frailty scoring suggested that 42 patients (23.0%) were not frail, 37 (20.2%) were vulnerable, 45 (24.6%) were mildly frail, 39 (21.3%) were moderately frail and 20 (10.9%) were severely frail. We found no statistically significant relationship in this cohort between frailty and AFS (log-rank p=0.085; Figure 3A). However, an overall trend is apparent upon inspection of the forest plot and some individual hazard ratios reached significance (Figure 3B). Frailty was shown to be associated with survival (p=0.03, Figure 4A), with hazard ratios all reaching significance (Figure 4B).
Discussion
This study adds to the existing evidence13,15 examining ambulatory care pathways for CLTI in demonstrating safety and efficiency for a group noted to be living with frailty.
The National Vascular Registry reported that, in 2020, the median (IQR) length of stay for non-elective endovascular, open and hybrid procedures was 11 (6–22), 13 (8–22) and 12 (7–22) days in the UK. Our results using the EVC model show a reduced length of stay compared with this, even in the context of the COVID-19 pandemic which was known to cause delays due to staffing levels and issues with theatre and intensive care capacity.17 This is most likely a result of the EVC pathway avoiding a lengthy preoperative hospital admission (resulting from delays to preoperative imaging and urgent unplanned theatre slots) when limited theatre slots were unavailable and there was no immediate urgency for admission due to sepsis or other emergent factors.
Our data show that there is a significant burden of frailty in the population with peripheral vascular disease, even in those deemed suitable for ambulatory treatment. It is known that frailty and its related syndrome of sarcopenia results in poorer outcomes after treatment for CLTI, and this has been shown in multiple populations globally.18-22 Our data support this finding.
Perioperative CGA and optimisation in older frail surgical patients has demonstrated clinical and cost effectiveness.23 The POPS service has spearheaded the implementation of CGA in our unit for multiple specialities including vascular surgery and has shown improvement in postoperative complications, delirium and a reduced length of hospital stay.24,25 The implementation of this service alongside the EVC has facilitated safe ambulatory treatment for this high-risk multi-morbid and frail population group.
An advantage of the ambulatory care model is that it avoids unnecessary out-of-hours inter-hospital transfer, thereby saving costs on patient transport and also relieving pressure on off-peak healthcare staff, both in specialist vascular centres and in emergency departments. Cognisant of the data showing increased mortality and need for ICU following night-time transfer,26 an EVC service provides an alternative pathway for timely senior vascular surgeon review that can remove pressure on out-of-hours resources with improved safety, without introducing delays to decision making. In addition, it can be argued that a more streamlined patient journey will result in an improved patient experience by reducing time waiting in emergency departments for a bed to become available and reduced time kept inappropriately nil-by-mouth. It is important to carefully triage those who still require emergency admission and distinguish those who can wait until the next day for a specialist review.
It is worth noting that, while we did treat a frail cohort via EVC, many patients who were at the worse end of the frailty spectrum (particularly if non-ambulatory) were not deemed appropriate for this pathway. For these patients we offer an outreach service that provides inpatient consultant reviews or virtual support to community teams with video/telephone consultations if appropriate. In addition, the times to admission and intervention were occasionally lengthy; this can be explained by theatre capacity still being a limiting factor and complicated revascularisations still requiring careful planning and CGA by the POPS service.
Our study is in agreement with previously published data on similar services in the UK, including the Leicester Vascular Limb Salvage (VaLS) clinic which showed reduced rates of MLLA in those managed via an ambulatory pathway after adjustment for multiple variables including disease severity.15 Our EVC shows similar rates of AFS at one year to the Leicester VaLS service (75% vs 72.8%). This has similarly been trialled in Manchester, where appropriately timely revascularisation time frames using a hot clinic model were demonstrated with comparable short- and long-term outcomes to emergency admission (81% AFS, albeit with a shorter follow-up time compared with our study).13
An advantage of our service is that we have managed to capture the whole cohort of CLTI patients who underwent intervention via the EVC pathway due to the prospective nature of the database used to monitor each encounter. We also have high quality follow-up data in this study due to the electronic nature of our hospital records which are linked to the centralised NHS Spine database, allowing us to reliably access data on re-intervention rates, follow-up encounters and death. We also include data prior to and during the COVID-19 pandemic, which allows us to demonstrate efficacy of this ambulatory model in both contexts.
A major limitation of this study is the retrospective nature of most of the clinical data collected. In particular, it would have been useful to gain information on rates of wound healing in those who presented with tissue loss; however, this was not possible from the electronic record notation system. We also have a lack of comparative data in this study, meaning we can draw conclusions about safety and efficacy but not superiority or non-inferiority. In addition, our service covers a large network with local follow-up protocols in place with incomplete data held at the hub site. Quantitative frailty information was also difficult to extract; while it was occasionally encoded as part of the CGA, it was not possible to retrospectively calculate this from the notes.
In addition, our single-centre experience may not apply to units across the country due to variation in geography, catchment area and patient demographics and co-morbidities. Despite these limitations, the study supports ambulatory emergency care for patients with CLTI and demonstrates the safety and efficiency of this approach.
Conclusion
This study shows that the GSTT NHS Trust’s EVC service provides a safe and effective model of care for the complexity and frailty of the CLTI patient cohort. Prospective multicentre research is needed to assess whether an ambulatory care pathway can be used as a model for vascular units and, in addition, further health economic analysis may help guide services in funding and staff allocation.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(3):167-173
Publication date:
May 5, 2023
Author Affiliations:
1. Guy’s and St Thomas’ NHS Foundation Trust, St Thomas’ Hospital, London, UK
Corresponding author:
Becky Sandford
Guy’s and St Thomas’ NHS Foundation Trust, St Thomas’ Hospital, Westminster Bridge Road, London SE1 7EH, UK
Email: [email protected]











