CASE REPORT
Blue toe syndrome secondary to multiple spontaneous aortic thrombi following pneumonia
Casey C
Abstract
A 65-year-old man presented with bilateral ischaemic toes 11 days following hospital discharge for pneumonia. His initial admission was complicated by atrial fibrillation requiring rivaroxaban on discharge. A thromboembolic cause of his toe ischaemia was suspected. An echocardiogram demonstrated only moderate atherosclerosis. However, repeat echocardiogram revealed five thrombi within the descending aorta. Medical management included therapeutic enoxaparin, aspirin, atorvastatin and a five-day course of iloprost. Subsequent right 5th toe amputation was required for osteomyelitis, but otherwise the patient made a full recovery and was asymptomatic at 12 months.
Introduction
Blue toe syndrome is a disease of the small arteries in the foot/toes characterised by painful blue discolouration in one or more toes. The most common aetiology is distal embolic disease. If foot pulses are palpable, medical management is frequently all that is required.
Case report
A 65-year-old man was readmitted to hospital complaining of pain, paraesthesia and blue discolouration in his left 3rd and right 4th and 5th toes. Eleven days previously he had been discharged from hospital following treatment of a lower lobe pneumonia. During his initial presentation he was Ig-G negative for Mycoplasma pneumoniae but strongly Ig-G positive when readmitted 11 days later, suggesting reactivation. An antinuclear antibody (ANA) screen was weakly positive. His initial hospital admission was complicated by the onset of rapid atrial fibrillation with resultant transfer to the cardiac care unit, where he spontaneously reverted. A transthoracic echocardiogram was functionally normal with moderate aortic atherosclerosis. He was initially discharged on rivaroxaban, doxycycline and amoxicillin (for one week).
Following discharge, the patient experienced paraesthesia and pain with purple mottling in his left 3rd and right 4th and 5th toes, which was most marked on leg elevation. On examination, peripheral pulses were palpable but both feet were cool. There was no previous history of peripheral arterial disease. He was an ex social smoker, with no personal or family history of coagulopathies. His past medical history included hypertension, paroxysmal atrial fibrillation, depression/anxiety, right total knee replacement, bilateral total hip replacements and cervical and lumbar fusions.
Despite recently being placed on rivaroxaban, a thromboembolic source was suspected. Thrombophilia screening was negative. The patient was reviewed by the vascular team who diagnosed blue toe syndrome, considered that there was no immediate threat to the limbs and suggested iloprost infusion for 5 days in addition to rivaroxaban.
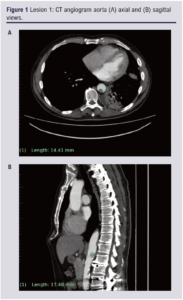
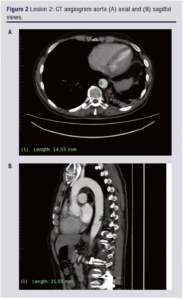
Following a transthoracic echocardiogram which excluded a cardiac embolic source, a CT angiogram demonstrated multiple foci of protuberant soft plaque within the thoracic and abdominal aorta which were considered to be the likely source of distal emboli (Figure 1 & 2).
Conservative medical management was considered the most appropriate initial treatment given viable feet, palpable foot pulses, disease burden and difficulty in accessing the lesions. Haematology recommended replacing rivaroxaban with therapeutic enoxaparin, and starting aspirin and atorvastatin with a view to plaque stabilisation. An outpatient PET/CT scan, given the weak ANA positivity, excluded vasculitis whilst a follow-up CT angiogram at 3 months demonstrated complete thrombus resolution. Due to established atrial fibrillation, enoxaparin was converted to rivaroxaban for ongoing therapeutic anticoagulation. The right 5th toe developed dry gangrene and osteomyelitis and was surgically amputated through the proximal phalanx at six weeks post representation. At one year follow-up the patient was asymptomatic and remained on rivaroxaban, aspirin and statin.
Discussion
Blue toe syndrome is the acute onset of painful, ischaemic, cyanotic toes in an otherwise well perfused foot, in the absence of trauma, cold injury or generalised cyanosis. Decreased arterial flow due to digital arterial embolism is the most common aetiology. Embolic sources include cardiac (atrial fibrillation, endocarditis, myxoma, post-myocardial infarction mural thrombus) and arterial (aortic and peripheral atherosclerotic thrombus and aneurysms). Rarer causes include in situ thrombosis (antiphospholipid syndrome, paraneoplastic syndrome), vasoconstrictive (Raynaud’s syndrome) and hyperviscosity disorders (cryoglobulinaemia).
Isolated aortic thrombus as a cause as in this case is relatively rare. It is plausible that a pro-coagulable state secondary to pneumonia was a contributing factor. Arterial thrombosis post pneumonia has been attributed to activation of the coagulation cascade, in particular platelet aggregation.1 Mycoplasma pneumoniae specifically is associated with thrombus formation in a number of case reports.2 The underlying mechanism has yet to be fully elucidated, with some authors suggesting that cytokine release directly affects vascular tissue.3-5 In several case reports, Mycoplasma pneumoniae has been detected in atherosclerotic plaque.6,7
Symptomatic treatment (analgesia), risk factor management (smoking cessation, hypertension control, management of hypercholesterolaemia) and medical management (antiplatelets, anticoagulation and vasodilatation) are frequently all that are required for blue toe syndrome. Surgical or endovascular management may be required to deal with the embolic source or remove ischaemic tissue.8,9
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2032;2(4):225-227
Publication date:
June 26, 2023
Author Affiliations:
Department of General Surgery, Sir Charles Gairdener Hospital, Perth, Western Australia
Corresponding author:
Cian Casey
Department of General Surgery, Sir Charles Gairdener Hospital, Perth, WA 6009, Western Australia
Email: cian.casey@ health.wa.gov.au











