CASE REPORT
Congenital absence of splenic artery: a rare cause of upper gastrointestinal bleed
Kiyawat V,1 Day C,1 Wells D1
Abstract
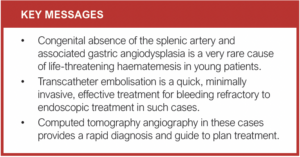
A 21-year-old woman presented as an emergency with upper abdominal discomfort and one episode of haematemesis. Physical examination, blood results and oesophagogastroduodenoscopy (OGD) were unremarkable. The patient collapsed following a large haematemesis 24 hours later and was intubated, ventilated and resuscitated. Repeat OGD demonstrated multiple areas of gastric angiodysplasia with active bleeding. Attempted haemostasis was unsuccessful. computed tomography angiography (CTA) demonstrated an absent splenic artery and multiple abnormal collaterals supplying the stomach, pancreas and spleen originating from a hypertrophied left gastric artery and gastro-epiploic arteries. Angiography demonstrated active bleeding from these abnormal collaterals, which were successfully embolised and haemostasis attained. On follow-up CTA, no evidence of further bleeding or infarction was noted. Congenital absence of the splenic artery is rare, with only four reported cases, and is an extremely rare cause of upper gastrointestinal bleeding.
Case details
A 21-year-old woman presented to the emergency department with upper abdominal discomfort and one episode of haematemesis. The patient had a previous history of haematemesis 10 years previously which was managed with medication and blood transfusion. There was no history of smoking, non-steroidal anti-inflammatory drugs or alcohol intake.
At presentation the physical examination was unremarkable. Initial blood results were pH 7.36, haemoglobin 118 g/l, haematocrit 0.36, platelets 326 109/l, INR 1.2, albumin 31 g/l, bilirubin 9 μmol/l, alkaline phosphatase 72 units/l, alanine aminotransferase 12 IU/l, albumin 31 g/L, amylase 74 units/l, sodium 140 mmol/l, potassium 5.1 mmol/l, urea 12.1 mmol/l, creatinine 52 μmol/l and glomerular filtration rate >90 ml/min/1.73 m2. On oesophagogastroduo-denoscopy (OGD), no active bleeding was seen.
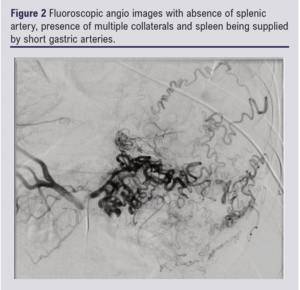
The patient collapsed with large haematemesis 24 hours later and underwent intubation, ventilation and resuscitation with packed red cells, fresh frozen plasma and platelets. She also received a proton pump inhibitor infusion, vitamin K and tranexamic acid. Repeat OGD demonstrated multiple small areas of actively bleeding gastric angiodysplasia in abnormal vascular territories. Attempted haemostasis at OGD was unsuccessful and the patient underwent computed tomography angiography (CTA) to delineate the vascular anatomy and plan treatment. CTA demonstrated an absent splenic artery, collaterals supplying the stomach, pancreas and spleen originating from a hypertrophied left gastric artery and gastro-epiploic arteries and a large volume of blood in the stomach (Figure 1).

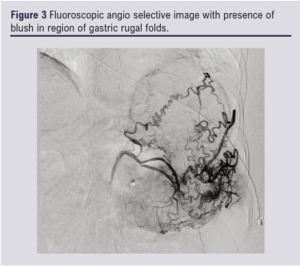
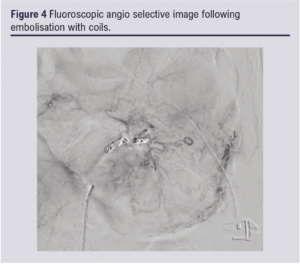
Following transfer to the interventional radiology theatre with anaesthetic support, the right common femoral artery was accessed using an ultrasound-guided modified Seldinger technique and secured with a 35 cm 5F sheath (Cordis). The coeliac artery was accessed with a 4F Sim 1 catheter (Cordis) and 180 cm Zip wire (Boston Scientific) followed by selective catheterisation of the left gastric and gastro-epiploic arteries. Angiography with pump injection at 10 mL iodinated contrast at 5 mL/s showed active bleeding from collaterals arising from the left gastric artery and gastro-epiploic arteries. Super-selective catheterisation of the tortuous branches was performed with a 130 cm 2.7F Progreat microcatheter (Terumo) (Figure 2 & 3). The bleeding vessels were successfully coil embolised with micronester coils through the Sim 1 catheter to haemostasis (Figure 4). The patient clinically improved over her course of stay in hospital with no further bleeding. On follow-up CT, no evidence of further bleeding or infarction was noted.
Discussion
Acute upper gastrointestinal bleeding is one of the most common medical emergencies in the UK with an estimated incidence of 134 per 100,000.1 Peptic ulcer disease remains the commonest cause for non-variceal upper gastrointestinal bleeding.2 Endoscopy is the investigation of choice for diagnosis and targeted endoscopic treatment3 after failure of conservative treatment.
Multidetector CT is a non-invasive tool for assessment of bleeding with a sensitivity of 86% and specificity of 95%.4 It not only determines the site and possible cause for the bleeding, but also displays the vascular anatomy which assists in planning subsequent endovascular intervention.5
In our case, failure to secure haemostasis at endoscopy led to CTA, which demonstrated active gastric bleeding from collateral vessels derived from hypertrophic left gastric and gastro-epiploic vessels with absent splenic artery. It was thus realised that haematemesis in our patient was due to bleeding from abnormal collateral vessels.6
Non-visualisation of the splenic artery and filling of the intrasplenic vessels through collaterals was in keeping with the absence of the splenic artery. Possible causes for splenic artery absence include atherosclerosis,7 thrombosis,8 surgery9 and congenital absence.
Atherosclerosis is usually seen in elderly patients and rarely results in complete occlusion.7 However, ischaemic changes in the spleen would be expected with splenic artery thrombosis.8
In our case there was congenital absence of the splenic artery. Only four cases of congenital absence of the splenic artery appear to have been reported, the details of which are shown in Table 1.6,10-12 Congenital absence of an artery frequently results in development of collateral channels with serpentine appearance, rhythmic convolutions and uniform size.13
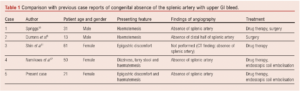
Transcatheter embolisation is a frequently effective treatment for acute non-variceal upper gastrointestinal bleeding refractory to endoscopy.14 It is fast, effective and a minimally invasive alternative to surgery. Most commonly, the splenic artery originates from the coeliac trunk; however, it is important to appreciate anatomical variability.15
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(4)222-224
Publication date:
June 26, 2023
Author Affiliations:
1. Radiology Department, Royal Stoke University Hospital, Newcastle Road, Stoke-on-Trent, UK
Corresponding author:
Vivek Kiyawat
Radiology Department,
Royal Stoke University Hospital, Newcastle Road, Stoke-on-Trent ST4 6QG, UK
Email: vivek.kiyawat@ uhnm.nhs.uk











