ORIGINAL RESEARCH
Frailty Assessment in UK Vascular Centres (FAVE): a survey to investigate data collection methods and impact on clinical practice
Hitchman L,1,2 Palmer J,2,3 Lathan R,1,4 Totty J,1,4 Smith GE,1,4 Carradice D,1,4 Chetter IC1,4
Plain English Summary
Why we undertook the work: Frailty is an important clinical syndrome. Frailty describes people who are more likely to have problems after a major health event, for example, an operation. The chance of being frail increases with age. Over 75% of people with circulation problems are over 65 years old. This means they have a higher chance of being frail and having problems after an operation. A patient’s level of frailty can guide vascular surgeons in planning care before, during and after an operation to reduce the risk of problems. Frailty can also be used to help discussions with patients about the risks of having certain operations. In 2019 the National Vascular Registry (NVR), an anonymous database of vascular operations, started to include the patient’s level of frailty on all operations entered onto their database. However, assessing frailty is only just becoming part of routine care in vascular surgery. To find out whether frailty is being measured in people with circulation problems, we conducted a survey of UK vascular surgeons.
What we did: We distributed an online questionnaire to vascular surgeons in the UK. The survey was advertised to vascular surgeons through Twitter and Vascular and Endovascular Research Network (VERN) and the Vascular Society of Great Britain and Ireland (VSGBI) email mailing lists and newsletters. The questionnaire was split into three parts. The first part asked where the surgeon was based. This was to ensure we gathered results from all over the UK. The second part asked questions about how frailty was assessed, which patients were assessed for frailty and how the surgeon used these assessments to guide patient care. The third part asked surgeons about their opinion about frailty. The survey ran from March 2022 to May 2022.
What we found: 48 surgeons who were based in 31 UK vascular centres completed the survey. Over half of the centres who responded assessed patients for frailty (61%, 19/31). Most centres use a scoring system to decide if someone is frail (68%; 13/19). The other centres use clinical judgement. The Clinical Frailty Scale was the most frequently used scoring system (77%; 10/13). Vascular surgeons perform frailty assessments in 47% (9/19) of centres and most assessments take place on the ward (68%;13/19). People are re-assessed for frailty following optimisation or an operation in 21% (4/19) of centres. The patient’s level of frailty was used to guide their care in 63% (12/19) of vascular centres. In the vascular centres that did not assess frailty more than half plan to start in the future (58%; 7/12). Vascular surgeons do not assess frailty because they are unfamiliar with the best way to do it and because they did not think the current ways of assessing frailty are applicable to some people with circulation problems.
What this means: There is a lot of variation in how patients with circulation problems are assessed for frailty in the UK. The top reasons vascular surgeons did not assess frailty are uncertainty in the best way to measure frailty and applicability of current frailty scoring systems for patients with circulation problems. Future research should address these reasons.
Abstract
Background: Frailty is an important clinical syndrome that is associated with adverse postoperative outcomes. The assessment of frailty provides an opportunity to enhance patient care. The National Vascular Registry (NVR) introduced frailty categories on all vascular procedure proformas in 2019. The aim of this survey was to capture the current practice of frailty assessment in vascular centres in the UK.
Methods: A nationwide survey was carried out of all UK vascular centres who enter procedural data onto the NVR database. The Qualtrics online survey tool was used to distribute the survey through mailing lists and social media. The survey captured data on location of centres who responded, how frailty data are collected and vascular surgeons’ opinions of frailty assessments. The survey was live from 29 March 2022 to 29 May 2022.
Results: The survey received responses from 48 UK vascular surgeons based in 31 UK vascular centres. Frailty assessment was undertaken in 61% (19/31) of centres that responded, of which 68% (13/19) used a frailty assessment tool. The Clinical Frailty Scale was the most frequently used tool (77%; 10/13). Vascular consultants personally perform frailty assessments in 47% (9/19) of centres and most assessments take place in the ward setting (68%; 13/19). Frailty was re-evaluated in 21% (4/19) of centres. Frailty status influenced clinical practice in 63% (12/19) of vascular centres. 58% (7/12) of responders plan to assess frailty in the future. Clinician-perceived barriers to assessing frailty was unfamiliarly with the tools and concerns over validity.
Conclusion: There is variation in how frailty is measured in UK vascular centres. Uncertainty and concerns over validation of tools are perceived barriers to assessing frailty. Further research should target validation of frailty tools and their role in guiding patient care in vascular surgery.
Introduction
The importance of frailty as a clinical syndrome is gaining momentum in surgical specialties. Frailty is defined as ‘a state of vulnerability to a stressor event, triggering disproportionate changes in health status’.1 Increasing age may lead to the clinical condition of frailty.1 In the UK, three quarters of patients presenting with vascular disease are over 65 years old, putting them at an increasing risk of being frail.2 Frailty has already been identified as a risk factor for morbidity and mortality at 30 days and one year post surgery in patients undergoing vascular procedures.3 Identifying preoperative frailty provides an opportunity for surgeons to work in multidisciplinary teams to optimise a patient’s preoperative state, plan admission to higher dependency units and organise appropriate rehabilitation.
There is no consensus on the gold standard tool for capturing frailty status in vascular patients. The National Vascular Registry (NVR) included frailty on all vascular surgical proformas from 2019 to help explore the influence of frailty on clinical outcomes.4,5 In order to accommodate centres using different tools, the NVR created frailty categories to enable centres to map their frailty score to the NVR categories if they were using either the Clinical Frailty Scale (CFS), Edmonton Frail Scale or the Electronic Frailty Index.4 Currently, other validated tools used for screening for frailty are not easily – or not at all – transferable to the NVR categories.
This survey aims to evaluate whether frailty assessments are being undertaken, how the frailty data are collected, and how frailty assessments inform clinical care in vascular centres in the UK.
Methods
This survey is reported with reference to the Checklist for Reporting of Survey Studies (CROSS).6
Design
A nationwide cross-sectional survey of frailty assessments was conducted in vascular centres in the UK. The survey was designed by a vascular speciality trainee and a research fellow with a PhD in frailty in vascular surgery. The survey was internally piloted in four vascular consultant surgeons, in line with the target population, until no further changes were necessary. The survey was then revised based on consensus opinion before being re-piloted. Major changes included removing details about the centre activity (as this is available through the annual NVR reports). Minor changes included removing questions on mechanisms of undertaking frailty assess-ments, such as length of time taken to perform an assessment and where the outcome was reported, as this was felt to be irrelevant. The survey was then shared with the Vascular and Endovascular Research Network (VERN) Executive Committee, which includes six consultant vascular surgeons, who externally piloted the survey. The survey was then amended based on consensus opinion until no further changes were necessary before distribution.
Eligibility
The survey was aimed at vascular consultant surgeons based in UK vascular centres. A UK vascular centre was defined as an NHS Trust who provides arterial services and submits data to the NVR. This includes the 101 NHS Trusts.7
Outcomes
The primary outcome of this survey was to establish how clinicians in UK vascular centres assess frailty in patients presenting to vascular services. The outcome measures were: name of the frailty assessment tool, type of patient screened for frailty, timing of frailty assessment and healthcare professional assessing for frailty. Secondary outcomes were: coverage of UK and Irish vascular centres in the survey, judged by response rate and geographical location of responders, impact of frailty assessment and clinician opinions of frailty assessment in vascular patients.
Data collection
The Qualtrics online survey tool (London, UK) was used to collect data. The survey was split into three sections. The first part captured the geographical spread of respondents to ensure the sample was representative of UK vascular centres. The second part explored frailty assessment. The third part investigated clinicians’ perceptions around frailty assessment. The survey items are included in Appendix 1 (online at www.jvsgbi.com). Multiple choices responses were permitted for questions Q7, Q8, Q10, Q12, Q17, Q22, Q29 and Q34. Results of these questions are presented as the total number of responders who selected each option in the question. The remaining questions were single response answers.
The survey was distributed in collaboration with the VERN and Vascular Society of Great Britain and Ireland via social media platforms and mailing lists. Convenience sampling was used to identify respondents. Responses from clinicians outside the UK were excluded from the analysis. The survey was re-distributed every month via Twitter and newsletters and collected responses between 29 March 2022 and 29 May 2022. Only responses during this window were included in the analysis, and after a lockout was enabled, preventing further responses. The QualtricsXM ‘prevent multiple responders’ function was used to prevent multiple participation of participants.
Analysis of data
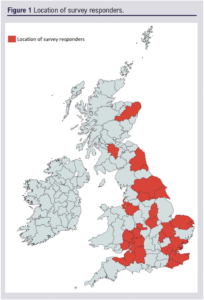
Only responders who had completed the survey were included in the analysis. Data submitted by responders from the same centre were checked for similarity before being entered into Microsoft Excel (Excel for Microsoft 365, Microsoft Corporation, Washington, USA). Descriptive statistics, including counts and frequencies, are reported where appropriate. Free-text responses of clinicians’ opinions were collated and described. Figure 1 was created using MapChart (https://www.mapchart.net/).8
Ethics and governance
The study did not require ethical approval as it was a survey of healthcare professionals and did not involve patients. Consent was indicated by completion of the survey. Responders could decide whether to provide their name and the centre at which they worked. Any identifiable responder information collected was kept confidential and destroyed at the end of the survey.
Results
Reach
The survey received responses from 31 (31%) vascular centres in the UK (Figure 1). Forty-eight consultant vascular surgeons completed the survey fully. There were responses from 28 centres in England, two centres in Wales and one centre in Scotland.
Frailty assessment
Frailty was assessed in 61% (19/31) of centres that responded. Nine units use a frailty assessment tool alone (47%; 9/19), four units rely on clinical judgement (21%; 4/19) and a further four use a combination of both (21%; 4/19). Two centres did not give details on how frailty was assessed. Responders from the same centre agreed on how frailty assessments were undertaken.
In the centres using a frailty assessment tool, the CFS was the most frequently used (77%; 10/13). Other tools included the Electronic Frailty Index and the Comprehensive Geriatric Assessment Toolkit. Clinical judgement of frailty, not using a frailty assessment tool, was undertaken by either a vascular medical physician, vascular perioperative physician, anaesthetist or care of the elderly physician.
Common reasons cited for selecting a frailty assessment tool were ease and speed of use (32%; 6/19), validated tool (37%; 7/19), fit to the local population (21%; 4/19), fulfilling NVR criteria (21%; 4/19) and prior experience using the tool (21%; 4/19). Other reasons included current use of the tool for research purposes at the NHS Trust, local NHS Trust policy, integration in electronic record systems, ‘national guidance’ and inclusion in other specialty clerking booklets.
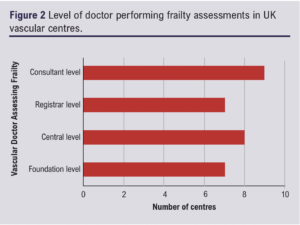
Healthcare professionals completing the frailty assessment tool were mostly consultant vascular surgeons (47%; 9/19), followed by vascular junior doctors (42%; 8/19), consultant vascular physicians (21%; 4/19), vascular specialist nurses (11%; 2/19) and physician associates (16%; 3/19). Other healthcare professionals were research nurses, advanced nurse practitioners, physiotherapists and occupational therapists. The seniority of the vascular junior doctor assessing frailty is shown in Figure 2. One-fifth of centres provide training for frailty assessment (21%; 4/19).
The location of frailty assessments included vascular outpatient clinics including pre-assessment clinics (74%; 14/19), hospital wards (68%; 13/19) and the emergency department (32%; 6/19).
One-fifth of responders reported frailty status was re-evaluated (21%; 4/19). This was undertaken prior to any operative intervention (25%; 1/4), after the patient’s clinical status was deemed to have changed (50%; 2/4) and after optimisation interventions (25%; 1/4).
Frailty status influenced clinical practice in most vascular units that assessed patient frailty state (63%; 12/19). Patient care was adapted according to frailty status in multiple ways. The most common ways were through prehabilitation planning (67%; 8/12), involving other specialists (67%; 8/12), earlier initiation of physiotherapy (58%; 7/12), rehabilitation (58%; 7/12), admission planning (25%; 3/12) and follow-up planning (42%; 5/12). Five centres used the degree of frailty to guide decisions to offer invasive interventions (42%; 5/12).
Patients screened for frailty
Thirty percent of responders screen all patients admitted to a vascular ward for frailty (32%; 6/19), 21% screen patients over 65 years old under the care of vascular services (4/19) and 21% screen all patients under the care of the vascular service (inpatients and outpatient) (4/19). Three (15%) centres screen all patients prior to aortic interventions. Other responders reported an ad hoc approach where patients are assessed depending on clinician judgement, depending on (poor) results from cardiopulmonary exercise testing and all patients presenting with chronic limb-threatening ischaemia.
Centres that do not assess frailty
Reasons responders cited for not assessing frailty at their vascular unit (38%; 12/31) included frailty assessments not being part of routine clinical practice (83%; 10/12), unfamiliarity with assessing for frailty (42%; 5/12), frailty status not impacting clinical management (8%; 1/12) and lack of evidence on the impact of frailty status on clinical management and outcomes (8%; 1/12).
In centres that did not assess frailty, two-thirds (67%; 8/12) reported that they planned to assess frailty in the future. The CFS (38%; 3/8) and the NVR categories (38%; 3/8) were the commonest choices. The Fried Frailty Phenotype Criteria (12%; 1/8) was proposed to be used by one centre and the other centre was undecided (12%; 1/8).
Reasons for the choice of tool were ease and speed of use (50%; 4/8), tool validation (50%; 4/8), fulfilling NVR criteria (50%; 4/8) and prior experience using the frailty tool (38%; 3/8).
Clinician opinions of frailty assessments
Clinician-reported barriers to carrying out frailty assessments in routine practice were uncertainty in how to assess frailty (53%; 8/15), concerns over validity of frailty tools in vascular patients (27%; 4/15), need for research into the benefit of assessing for frailty (13%; 2/15), requirement for input from care of the elderly specialists (7%; 1/15) and no perceived benefit of frailty assessment over end-of-the-bed review (7%; 1/15).
Themes arising in the free-text responses included the view that frailty assessment had a positive impact on patient care. Clinicians reported frailty assessments result in additional support by both the care of the elderly ward and the perioperative care for older people undergoing surgery (POPS) teams, who specifically tailor the care of older patients (but not necessarily frailer) to support any additional needs.
However, other responders felt assessing frailty is a ‘tick-box’ exercise and has little clinical value over end-of-the-bed assessment. Others felt the application of current tools are not appropriate in certain patient groups – for example, those with chronic limb-threatening ischaemia. Some clinicians felt frailty assessments should be undertaken by care of the elderly specialists as surgeons are ‘incentivised’ to operate, whereas care of the elderly clinicians are able to optimise patients based on findings from frailty assessments. “Knowing the degree of frailty alone is of no benefit”, noted another respondent.
Some responders felt assessment of frailty in vascular patients could have an important role in patient care, but that further research was required to guide the use of frailty status in decisions around offering high-risk surgical interventions.
Discussion
This survey found frailty is assessed in over half of the centres that responded, with a further quarter planning to introduce frailty assessments, signifying a growing role of frailty assessment in vascular practice. However, uncertainty in undertaking frailty assessment, along with queries about validation of existing tools in vascular patients and variable input from care of the elderly specialists, has resulted in some vascular surgeons questioning the value of frailty assessments until future research is available.
There are currently a plethora of tools that measure frailty, which can be considered in two main types – the cumulative deficit9 and the phenotype frailty models.10 A cumulative model quantifies frailty through an increasing number of co-morbidities, whereas a phenotype model describes frailty as a group of characteristics. There is some overlap between these models11 – for example, functional decline as measured in the deficit-driven model will encompass cumulative factors identified in the phenotype model such as physical activity, muscle strength and walking speed.
A range of frailty assessment tools has been used to predict the risk of adverse outcomes in patients undergoing vascular procedures.12 Studies of patients undergoing vascular procedures report the Hospital Frailty Risk Score, FRAIL (Fatigue, Resistance, Aerobic capacity, Illness and Loss of weight) screening tool, Groningen Frail Indicator, Addenbrookes Vascular Frailty Score, modified Frailty Index and Risk Analysis Index can all predict 30-day mortality, postoperative complications and requirement for a higher level of care on discharge.13-20 Critics of these tools argue that they describe cumulating co-morbidities rather than detecting the phenotypical characteristics of frailty, and therefore contest their validity as tools to identify frailty. In addition, these studies often exclude patients who did not undergo an intervention which introduces selection bias and limits generalisability. The responders of this survey felt a major role of frailty assessment tools is to predict the risk of surgical morbidity and mortality. While frailty may be associated with increased surgical risk, the relationship is complex and the ultimate aim of frailty assessment tools is to reliably diagnose frailty and improve care. The NVR has stated that the CFS, Edmonton Frail Scale and Electronic Frailty Index can all map onto the four categories of frailty recorded in the NVR4 but, again, validation of these scales to diagnose frailty in vascular patients is still awaited.9,21-23
In this survey, some surgeons reported that the assessment of frailty results in reduced postoperative complications in their vascular centre. This finding is likely confounded by those who have a positive experience also having resources to optimise individuals identified as frail. Nonetheless, similar findings are reported in the literature; collaboration between the vascular team and specialist perioperative care of the elderly team results in fewer complications, shorter length of stay and fewer 30-day readmissions.24 This likely drives the reported cost effectiveness of assessing frailty.25,26 These findings should be considered by vascular centres when allocating resources.
Another application of frailty assessment is to inform decision making around ‘high-risk’ interventions. This area is more contentious, as risk is subjective and comprised of many components, of which patient related risk is only one aspect.27 Frailty screening must not increase harm to older frail persons by denying a patient a surgical intervention based on the score alone. The British Geriatrics Society (BSG) and Centre for Perioperative Care (CPOC) provide extensive guidance on how frailty assessment can complement care throughout the surgical pathway to complement shared decision making, rather than dictate it.28,29
Time, ease of use and prior experience were all listed reasons why units chose to adopt certain frailty tools. A combination of patient-reported outcomes and surgeon-performed frailty assessment using the CFS could provide a reliable and efficient method of assessing frailty in the outpatient clinic setting.30,31 Some vascular surgeons in this survey felt they performed just as well as frailty assessment tools; while the end-of-the-bed assessments could be a useful screening tool to trigger a more in-depth frailty assessment, further validation work is needed.32
The CFS was the preferred frailty assessment tool in this survey. It is a user-friendly tool that describes the sequential degrees of frailty in text and pictorial form. The BSG/CPOC guidelines recommend using the CFS to assess frailty in all those over 65 years old and those under 65 years old at risk of frailty prior to surgery.29 While the CFS is a validated, easy to use and recommended tool to use in patients prior to surgery, there are concerns about its applicability in certain vascular patient groups. For example, those with claudication and progressive limb ischaemia due to peripheral arterial disease report similar symptoms to those described in the CFS of limited walking ability and being ‘slowed up’. The differentiation between declining function due to frailty versus symptoms of lower limb ischaemia is difficult to untangle and may affect the validity of the CFS in these patients. Curiously, few centres reported using the Electronic Frailty Index, despite it being a validated tool recommended by NHS England to GPs to assess those over 65 years old for frailty that is often included on the patient’s GP record,33 that can also be mapped on the NVR’s frailty categories.
The major limitation of this survey was engagement. The survey gained responses from vascular centres spread throughout the England; however, engagement from the devolved nations was limited, with only two responses from Wales, one response from Scotland and no responses from Northern Ireland. While the survey does give an indication of the current state of frailty assessments in England, it cannot reliably report on practice in Scotland, Wales or Northern Ireland. The survey is also subject to selection bias, where those in support of frailty assessments are more likely to have completed the survey compared with those who do not assess frailty and those more sceptical of frailty assessments. This could have skewed the results and potentially mean most vascular units in the UK actually do not routinely assess for frailty. Other implications of the low response rate include those surgeons who did respond could not represent the practice of that unit and skew the reported methods on how frailty is assessed and the impact it has on patient care. Other limitations include the views surgeons have on frailty in vascular surgery may not be represented by the 48 surgeons who provided responses. Nonetheless, the results of this survey support the NVR Annual Report 2021, which reported that an insufficient amount of frailty data is submitted, potentially due to frailty assessment not being undertaken, which prevents exploration of the relationship between frailty and mortality.5
Conclusion
This survey has demonstrated the variation in frailty assessment in vascular centres in England and Wales, although generalisability of the results are limited by lack of engagement. The preferred method to assess frailty is with a tool such as the CFS. Vascular surgeons believe frailty assessment could play an important role in shared decision making, especially in high-risk cases. However, barriers to implementation of frailty assessment include concerns of validity of frailty assessment methods in vascular patients, uncertainty in how to perform frailty assessments by vascular surgeons and insufficient resources to optimise the care of those identified as frail. Ongoing studies should target validation of the frailty tools recommended by the NVR to guide the role of frailty assessments in vascular surgery.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(2):69-75
Publication date:
January 9, 2023
Author Affiliations:
1. Hull York Medical School, Hull, UK
2. University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK
3. University of Birmingham, Birmingham, UK
4. Hull University Teaching Hospitals NHS Trust, Hull, UK
Corresponding author:
Louise Hitchman
NIHR Doctoral Research Fellow, Academic Vascular Surgery Unit, 2nd Floor, Allam Building, Hull Royal Infirmary, Anlaby Road, Hull, HU3 2JZ, UK
Email: [email protected]











