EDITORIALS
Management of iatrogenic acute limb ischaemia in the paediatric intensive care unit population
Kwan JY,1 Stocco F,1 Ali RK,1 Bourke G,2 Natalwala I,2 Richards M,3 Puppala S,4 Finn D,5 Scott J,1 Stansfield T,1 Forsyth J1
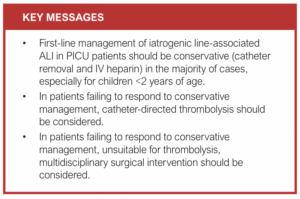
In the Paediatric Intensive Care Unit (PICU) an arterial line is often inserted in critically unwell children to allow for reliable blood pressure monitoring and access to arterial blood for point-of-care blood gas analysis and laboratory testing. However, arterial catheterisation is a procedure that carries the risk of serious complications including impaired tissue perfusion, thrombotic events and limb ischaemia.1 The typical clinical features of iatrogenic acute limb ischaemia (ALI) in PICU patients include: (1) pallor (pale discolouration, mottling, cyanosis), (2) perishingly cold (cold to touch, use of temperature probe), (3) pulseless (absent distal pulses in affected limb), and (4) 3As (increasing analgesia requirements, anxiety and agitation). Importantly, other classical features of ALI such as pain, paralysis and paraesthesia are less useful in a PICU setting where patients are often sedated and ventilated.
Most cases of iatrogenic ALI in PICU patients are successfully managed with non-operative management alone, with a low risk of limb loss. King et al2 quoted a limb loss risk of 0.6% in 10,394 patients >1 month of age with femoral artery catheterisation, whilst Totapally et al3 quoted a limb loss risk of 3.1% in 961 children with extremity arterial thrombosis.
Most commonly, patients are anticoagulated with an intravenous heparin infusion and, if the limb remains viable, this is generally converted to therapeutic low molecular weight heparin for a further 5–7 days.4-6 The evidence base for anti-coagulation duration is limited, and it may be effectively extended for up to 3 months if needed, guided by arterial duplex and clinical assessment.7 It is important to be aware that the evidence for heparin in children and neonates is minimal, but it is generally considered a UK medicolegal standard. If a negative outcome such as amputation arose in a paediatric ALI patient not receiving appropriate anticoagulation (except in neonates deemed to be at high haemorrhagic risk), it would likely be deemed to have fallen below the expected standard of care. Other conservative measures include the use of glyceryl trinitrate patches, milrinone and peripheral nerve blockade.8-11
Rarely, in cases of severe ischaemia when conservative medical management fails, surgical or endovascular intervention may be considered when expertise in microsurgery, micro-sheaths, wires and catheters may be required, especially in neonates.12 However, such interventions, despite being with the best of intentions, can still cause further severe iatrogenic injury. A multidisciplinary approach is generally required with the involvement of vascular, paediatric and plastic surgery; vascular interventional radiology; and paediatric haematology if thrombolysis is being considered. Both systemic and catheter-directed (CD) thrombolysis may be considered. However, systemic thrombolysis is associated with a significant bleeding risk. Woods et al13 highlighted that although almost 80% of paediatric patients receiving systemic thrombolysis achieve complete or partial thromboembolism resolution, up to 15% have major bleeding complications. Whilst there are no randomised controlled trials comparing systemic and CD thrombolysis in children, low-level evidence suggests that CD thrombolysis is safer and more efficacious. Rizzi and Albisetti14 describe a thrombus resolution rate of 70% with systemic thrombolysis versus 85% for CD thrombolysis, and a major bleeding rate of 9–40% for systemic thrombolysis versus 7% for CD thrombolysis.
Open surgical intervention in very small children should be avoided if possible. Lin et al15 found that adverse events and postoperative mortality all occurred in those aged <2 years (p<0.05), whilst those aged >2 years all regained palpable pedal pulses in the follow-up period. This suggests a need for increased caution regarding surgical intervention in children aged <2 years. This is reflected in the European Society of Vascular Surgery (ESVS) 2020 Management Guideline for ALI, which recommends initial conservative management with heparin for infants and children younger than 2 years of age.12
In the surgical repair of iatrogenic common femoral artery injuries in children (average age 5.8 years), Aspalter et al16 recommended primary vein patch angioplasty using heparin, topical papaverine, a microsurgical technique with optical magnification and a longitudinal arteriotomy to facilitate access to profunda femoris and superficial femoral arteries. Lin et al15 reported outcomes of femoral artery catheter-related ALI in 14 paediatric patients (average age 4 years) managed using size #2 or #3 Fogarty embolectomy catheters in all patients and saphenous vein patch angioplasty in the majority. Fogarty embolectomy catheters may cause vasospasm and intimal injury, therefore the smallest sized catheter possible should be used with caution.
Iatrogenic aortic injury and/or thrombosis is a recognised complication of umbilical artery catheterisation (UAC), which is considered the standard of care for arterial access in neonates.17 Aortic thrombosis secondary to UAC classically presents with a triad of congestive cardiac failure, severe hypertension and bilateral ALI.18 In infants with mild and transient ischaemia that resolves with catheter removal, conservative management may be all that is required and includes heparinisation, protective wrapping of the limb/s, reflex warming and careful observation.19
For patients with bilateral severe ALI secondary to aortic thrombosis from UAC, open surgical management (eg, transabdominal aortotomy with thrombectomy) has been advocated.18,20,21 However, open surgical intervention for aortic thrombosis/iatrogenic injury within the context of UAC and bilateral ALI should be tempered with rationalisation and discretion. Aggressive conservative management is appropriate in the majority of cases of ALI secondary to UAC, and thrombolysis may also be considered within the appropriate clinical context. Current evidence does not mandate open surgical intervention, but as a consideration.
It is crucial to consider what constitutes a ‘realistic’ outcome following iatrogenic ALI in the PICU population. Chaikof et al22 described their experience of operating on seven infants under the age of 6 months on PICU with iatrogenic ALI. Although there were no instances of limb loss, palpable pulses were restored in only 56% of limbs. Additionally, long-term outcome is often poorly recorded, highlighting the need for appropriate follow-up. The authors concluded that “… although thrombectomy is a safe and simple procedure in even the very youngest of patients with arterial insufficiency, surgical optimism should be tempered by frequent inability to achieve full and durable success …”. It is important for clinicians to remember that these patients are likely to be frail and sick neonates, and despite the notion that surgical intervention may well be possible, it needs to be categorised and considered within the overall holistic context.
Finally, in the devastating situation of a PICU patient with non-salvageable ALI, amputation should be delayed for as long as possible as the eventual line of demarcation may be some way distal to the original line of ischaemia.23 Amputation should be undertaken with full consideration of future prosthetic limb application and joint contracture prevention. Amputation should be performed by a multidisciplinary team of surgeons experienced in paediatric major amputation, paediatricians, occupational therapists, physiotherapists and prosthetists to ensure the best outcome for the child.
Conclusion
Iatrogenic ALI in the PICU population is a rare but potentially catastrophic event associated with the possibility of limb loss, long-term disability and mortality. Conservative management with anticoagulation and ongoing specialist input from a multidisciplinary team should be considered the standard of care. The multidisciplinary team should include clinicians from PICU, vascular surgery, vascular interventional radiology, plastic surgery, paediatric surgery and paediatric haematology. This multidisciplinary team approach is likely to yield the best long-term result in most of these patients.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(2):62-64
Publication date:
February 8, 2024
Author Affiliations:
1. Leeds Vascular Institute, Leeds General Infirmary, UK
2. Department of Plastic Surgery, Leeds General Infirmary, UK
3. Department of Paediatric Haematology, Leeds General Infirmary, UK
4. Department of Interventional Radiology, Leeds General Infirmary, UK
5. Department of Paediatric Intensive Care Unit, Leeds General Infirmary, UK
Corresponding author:
Jing Yi Kwan
Leeds Vascular Institute, Leeds Teaching Hospitals NHS Trust, Great George Street, Leeds LS1 3EX, UK
Email: [email protected]











