ORIGINAL RESEARCH
Outcomes of vascular interventions for chronic limb-threatening ischaemia in nonagenarians
Atkins E,1 Stather P,1 Burrows M,1 Singh A,2 Medagoda A,1 Ezzarghani A,1 Al-Jundi W,1 Mughal NA2
Plain English Summary
Why we undertook the work: People in the UK are living longer with lots of medical conditions. This means people aged over 90 are more likely to need vascular surgery for lack of blood supply to the legs. We wanted to know what the results of surgery or keyhole procedures to improve blood supply are in these people.
What we did: We looked at people aged 90 and older who were admitted to one hospital with a severe lack of blood supply to the leg, and had a surgical or keyhole procedure to improve it to try to save the leg. People admitted between January 2010 and December 2017 had their medical records reviewed, and we looked at how many of them were alive 30 days, 90 days and 1 year after their first procedure.
What we found: We looked back at the medical records of 99 patients. Their average age was 92. The 99 patients had 117 procedures between them, with 15 legs needing more than one procedure; 5.1% of people died in the first 30 days after their procedure, 18.2% died in the 90 days after and 44.4% died in the year after. If people came to hospital as an emergency, they were less likely to be alive at 1 year than someone coming in as a planned admission
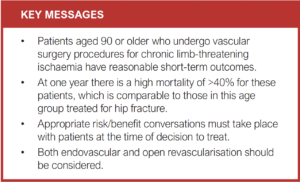
What this means: There is a high chance of someone aged 90 or older dying in the first year after a procedure for a severe lack of blood supply to the leg, about the same as for patients who have an operation for a broken hip. Our operations provide pain relief and an ability to retain independence, so we should continue to consider them in people of this age.
Abstract
Background: With increasing age of the population, more patients over 90 years old are being referred to vascular surgery with increasingly complex comorbidity. There are minimal data on undertaking revascularisation at this extreme of age. This study therefore aims to evaluate the outcomes of nonagenarians who underwent vascular surgical procedures for chronic limb-threatening ischaemia.
Methods: A retrospective clinical record review was carried out of all patients aged 90 and older with chronic limb-threatening ischaemia who presented to a tertiary centre between January 2010 and December 2017 and underwent vascular surgical intervention. Primary outcomes were mortality at 30 days, 90 days and 1 year.
Results: Ninety-nine patients were included. The median age was 92 years (IQR 90–94) and median follow-up was 15 months (IQR 4–32). A total of 117 limbs were treated, with 15 limbs requiring multiple procedures. Of the patients’ first procedures, 76 (76.8%) were endovascular, 14 (14.1%) open and 9 (9.1%) were major limb amputations. The 30-day, 90-day and 1-year procedural mortality rates were 5.1%, 18.2% and 44.4%, respectively, with higher mortality for emergency cases at 1 year (p=0.045).
Conclusions: Mortality for these procedures in patients aged over 90 is high, similar to patients who undergo surgery for hip fracture. Given similar benefits for treatment in terms of pain relief and ability to retain independence, patients in this age group should be considered for limb salvage procedures.
Introduction
The ageing population is growing. In 2020 there were 609,503 UK residents aged 90 and over, an increase of more than 2.5 times in the past 30 years.1 Cardiovascular disease is a large contributor to morbidity and mortality in this age group,2 and consequently older patients are being referred for vascular surgery evaluation.3
Given increasing comorbidities,3 decision making in this population becomes difficult. Risk stratifying scores such as V-POSSUM (Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity) and V-POSSUM Cambridge scores have not been validated in elderly patients.4 This population carries an increased perioperative and postoperative mortality for vascular procedures, with a study by Saarinen et al evaluating outcomes in patients with either chronic limb-threatening ischaemia or acute limb ischaemia highlighting a 1-year survival rate of 50%.5 It is important that an accurate picture of risk is discussed with patients and their advocates prior to any procedures carried out, as well as their potential benefits.
Current guidance from the Vascular Society of Great Britain and Ireland recommends early revascularisation for presentations of chronic limb-threatening ischaemia in order to prevent limb loss.6 The Global Vascular Guidelines recommend offering revascularisation to patients after taking into account their surgical risk, level of ischaemia and how threatened their limb is.7 Surgical risk is difficult to assess. Average-risk and high-risk patients are defined by estimated procedural and 2-year all-cause mortality, with the list of predictors including age, chronic kidney disease, coronary artery disease, congestive heart failure, diabetes mellitus, smoking, cerebrovascular disease, tissue loss, body mass index, dementia and functional status. However, the Global Vascular Guidelines recommend no particular model to assess surgical risk.
The aim of this study was to evaluate outcomes of vascular surgery for chronic limb-threatening ischaemia in nonagenarians, to compare elective and emergency surgery, and open and endovascular procedures. As the ageing population grows, this information will help guide decision making, consent discussions and risk stratification.
Methods
A retrospective notes review of patients aged 90 and older who underwent revascularisation or major amputation following a presentation with chronic limb-threatening ischaemia at one tertiary vascular unit in the UK was carried out, with reporting according to STROBE guidelines.8 The study was registered with the local Norfolk and Norwich University Hospital institutional audit department to ensure all data collection was in line with local committee ethical standards and, after review by the local R&D department, the study was deemed exempt from ethical approval owing to the minimal risk and non-identifiable nature of the study. Patients were de-identified and analysed anonymously.
Patients admitted between January 2010 and December 2017 were included and the demographics and comorbidities of the cohort were captured. These included age, sex, diabetes, hypertension, chronic kidney disease, chronic obstructive pulmonary disease, ischaemic heart disease, having had vascular surgery in the past, stroke, heart failure and smoking history. Chronic limb-threatening ischaemia was defined as rest pain or tissue loss. The frailty score and Rutherford classification were also calculated. Patients were identified through both surgical and interventional radiology procedural databases and cross-referenced with departmental governance data. Case notes, discharge summaries and clinic notes were used for data collection. Deaths were identified from patient records. Follow-up was completed in April 2021.
The type of procedure was recorded and grouped as to whether it was elective or emergency (defined as an outpatient or inpatient pathway), and open or endovascular. Data were also collected on their discharge destination and whether they returned to the address from which they were admitted to hospital within 3 months. This was retrieved from the Trust’s Patient Administration System. A ‘nursing home’ was defined as a care destination which always has a qualified nurse on site whereas a ‘care home’ has trained care assistants. Patients who require a nursing home have increased care needs compared with those who require a care home.
The decision to treat a patient in their 90s who presented with chronic limb-threatening ischaemia was made by the admitting vascular surgeon. An opinion from a consultant vascular anaesthetist was sought prior to any open vascular surgical procedure. Patients on an elective pathway were discussed at weekly vascular multidisciplinary team (MDT) meetings; however, MDT discussion for emergency admissions were variable depending on day of admission. Patients who were deemed too high risk for any procedure were managed conservatively. Input from geriatricians was not routinely sought.
The primary outcome measured was mortality at 1 year. Secondary outcomes included discharge destination, re-interventions, amputation, and mortality at 30 and 90 days.
Data analysis
Statistical analysis was carried out using Kaplan–Meier curves to calculate mortality, statistical significance being calculated using Mantel–Cox log rank test and Fisher’s exact test or χ2 test depending on raw numbers. Descriptive statistics were documented as percentages. For patients who had more than one procedure in the follow-up period, the first procedure only was used in mortality calculations. Statistical significance was defined as p<0.05.
Study size was based on the number of cases undergoing the procedure during the study duration and was not a calculated sample size. Missing data were reported as such and statistical analyses based on the number with data obtained. No matching of cases or sensitivity analyses were possible due to the nature of the study and sample size.
Results
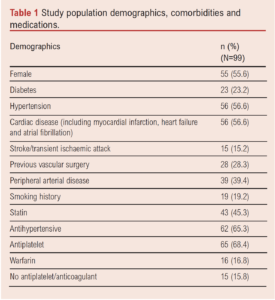
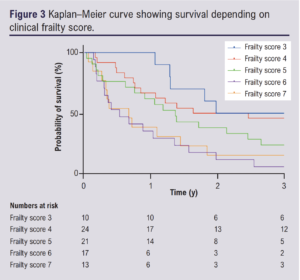
Ninety-nine patients (44.4% male) who underwent 117 procedures were identified. The median age was 92.4 years (IQR 90.9–94.6) with a median follow-up of 1.24 years (IQR 0.37–3.17). A total of 101 limbs were treated, 67.5% of which were treated following emergency admission. Patient comorbidities and medications are shown in Table 1 and were commensurate with standard vascular risk factors. Twenty-eight patients (28.3%) had previously undergone vascular intervention. The Rutherford classification was known for 94 patients: 43.6% had Rutherford stage 6, 41.5% had stage 5, 10.6% stage 4 and 4.3% stage 3. Clinical frailty scores were also calculated for 85 patients, with 15.3% scoring 7, 20.0% scoring 6, 23.5% scoring 5, 28.2% scoring 4, 11.8% scoring 3 and 1.2% scoring 2.
 Eighty-four limbs underwent a single intervention and 15 limbs underwent a secondary procedure with one limb undergoing three procedures. Primary procedures included 78 angioplasties, nine femoral endarterectomies±angioplasty, five lower limb bypasses and nine major limb amputations (above or below knee). Secondary procedures included nine major limb amputations following angioplasty, five repeat angioplasties, one femoral endarterectomy post-angioplasty and one redo femoral endarterectomy.
Eighty-four limbs underwent a single intervention and 15 limbs underwent a secondary procedure with one limb undergoing three procedures. Primary procedures included 78 angioplasties, nine femoral endarterectomies±angioplasty, five lower limb bypasses and nine major limb amputations (above or below knee). Secondary procedures included nine major limb amputations following angioplasty, five repeat angioplasties, one femoral endarterectomy post-angioplasty and one redo femoral endarterectomy.
The 30-day, 90-day and 1-year procedural mortality rates for all patients were 5.1%, 18.2% and 44.4%, respectively (Table 2). Median survival time was 1.23 (IQR 0.37–3.17) years. One-year mortality rates for patients undergoing open surgical revascularisation and angioplasty (excluding amputation) were 64.2% and 42.1%, respectively (p=0.13). These differences were also non-significant at 30 and 90 days post-procedure (Table 2). Median survival was higher following endovascular procedures than open surgery (1.29 years (IQR 0.37–3.17) vs 0.93 years (IQR 0.38–2.98)), but no significant difference between Kaplan–Meier curves (Figure 1) was demonstrated on the Mantel–Cox log rank test (p=0.9).
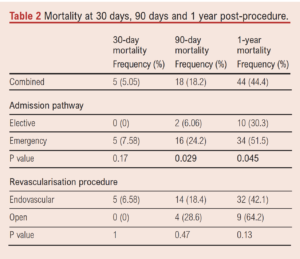

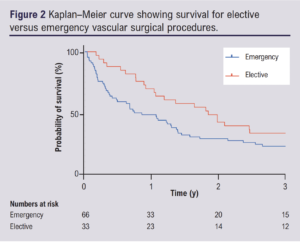
Mortality at 1 year following emergency cases was 51.5% whilst that following elective cases was 30.3% (p=0.045). Table 2 shows that the differences in mortality were not significant at 30 days post-procedure but were significant at 90 days post-procedure (p=0.029) and at 1 year. Median survival was higher following elective procedures than following emergency surgery (2.04 years (IQR 0.90–3.43) vs 0.86 years (IQR 0.29–3.08)), but no significant difference between Kaplan–Meier curves (Figure 2) was demonstrated on the Mantel–Cox log rank test (p=0.16).
Prior to the first admission, 13.1% of patients lived in a care home, 77.8% in their own home, 2.0% in a nursing home and 7.1% in sheltered housing. Three months following discharge 87 patients were alive, of which 17.2% were in a care home, 71.3% in their own home, 4.0% in a nursing home, 5.1% in sheltered housing and 1.0% in a hospice. This resulted in 94.3% of surviving patients maintaining their preoperative level of independence at 3 months.
Of the 77 patients who were admitted to hospital from their own home, all survived to discharge. Discharge destination was their own home for 68 patients (88.3%), a care home for four patients (5.19%), a rehabilitation placement for three patients (3.90%) and a nursing home for two patients (2.60%). Seventy patients (90.9%) were alive at 12 weeks, 66 (94.3%) of whom had returned to their own home, three (4.29%) were living in a care home and one patient (1.43%) was in a hospice.
Clinical frailty was analysed to determine whether increasing frailty was associated with long-term survival. Kaplan–Meier analysis and log-rank test showed a significant association between increasing frailty scores and poorer survival (p=0.0005, Figure 3).
Discussion
These data highlight the fact that patients at the extremes of age are able to undergo vascular intervention, with the majority of patients able to maintain their pre-existing level of independence. With careful patient selection, patients over the age of 90 can return to independent living with revascularisation and should not be turned down for intervention based on age, but the risks and benefits of intervention should be appropriately discussed.
As the number of nonagenarian patients referred to vascular surgeons increases, it is important to identify those who would benefit most from invasive vascular surgical procedures, which often have significant risk attached. This assessment and identification is challenging and requires close working with the surgeon, anaesthetist and care of the elderly physician to optimise patients perioperatively. Patient frailty is an independent risk factor for poor outcomes in vascular surgery,9 which is in accordance with the findings of this study. Many tools to assess frailty exist, and not all are validated in the surgical population. In addition, not all patients with increased surgical risk will be frail and there is no evidence to decline surgery based on a frailty score alone.9
The overall 30-day mortality rate for vascular surgery procedures in nonagenarians, combining elective and emergency operations over the study period, was 5.1%. This is comparable to the literature on general surgery for patients aged 90 years or older, with a 30-day mortality rate of 8.4% reported by Hosking et al10 and 6.2% reported by Sudlow et al.11 In the literature on vascular surgery, the 30-day mortality rate for patients aged over 90 following combined elective and emergency procedures ranges from 6.2% to 12.7%.12
Mortality in our study cohort was not significantly increased at 30 days for emergency procedures compared with elective procedures, but was at 90 days and one year. The lack of an early significant difference is likely due to all of these cases having chronic limb-threatening ischaemia and therefore undergoing intervention within a short period of time from referral regardless of mode of presentation. At 1 year, mortality reached 51.5% in emergency cases and 30.3% in elective cases. These outcomes are worse than in a younger cohort,13 and as such underline the importance of frank and honest conversations about expected outcomes with patients and their advocates when making the decision to perform a surgical intervention.
When comparing open procedures to endovascular procedures, there was a higher mortality at 1 year for those undergoing open surgery, which was not significant. It is also important to note that all cases of open surgery had no endovascular option, and as such it is not a like-for-like comparison. These data suggest that an ‘endovascular first’ strategy may be beneficial in the over-90s, especially with recent and ongoing advances in what can be achieved via endovascular methods, although clearly this is not possible in all cases. The mortality of 44.4% in all those undergoing interventions for chronic limb-threatening ischaemia at 1 year is comparable to patients undergoing surgery for hip fracture, which has an associated 1-year mortality rate of 25–50% in this age group.14,15 Given the similarities in these patient cohorts, including poor functional status, pain and reduced quality of life, a similar approach to treatment could be considered as the benefits of limb salvage, mobility and pain relief in both scenarios are considerable, so open surgery should remain an option in selected patients.
It is exceedingly difficult to determine how much benefit one individual will derive from a vascular surgical procedure, especially in the context of high risk of harm. A woman aged 90 in England is expected to live a further 4.61 years and a man 4.09 years,16 and by the age of 92 (the median age of our study cohort), the life expectancy is 3.94 further years for women and 3.5 for men. Our results show a median life expectancy of 1.19 years for nonagenarians fit enough to undergo vascular intervention, and the decision-making process should thus take into account the limited life expectancy for patients of this age.
It is evident from this study that the majority of patients over the age of 90 were treated as an emergency. This may be due to a reluctance of healthcare professionals to make a referral to tertiary providers for patients in this age group, but it may also be due to the perspective that vascular surgeons may adopt a more conservative approach to patients in this age group when seen in clinic compared with younger patients. In the context of emergency presentation, particularly if the patient has intolerable pain or significant tissue loss, the patient and their advocates may be willing to accept a higher level of risk. There may also be corresponding pressure on the surgeon to ‘do something’ when faced by a patient in extremis.
Fewer than half of the study cohort were taking a statin and over a quarter were not taking any antiplatelet or anticoagulant medication. Previous research on best medical therapy in vascular surgery patients has shown similarly limited cardiovascular risk factor modification.17 This leads to an increased perioperative cardiovascular risk, especially in the population with peripheral vascular disease,18 and may have contributed to the high mortality we have described. The harms of overprescribing have been a recent focus of the UK Department of Health and Social Care, with a review of the topic being commissioned in 2018.19 Whilst there is no standardised definition of polypharmacy, its prevalence is increasing in older adults, along with its negative associations.20 A meta-analysis of de-prescribing in older adults has shown that mortality is not affected,21 but a specific subgroup analysis of patients with peripheral vascular disease has not been carried out. Clinician education on the benefits of secondary prevention in peripheral vascular disease could be a potential solution to ensure patients with cardiovascular risk factors are on appropriate secondary prevention medications.
This study has several limitations. Data on those patients who did not undergo intervention has not been obtained to provide a comparative analysis, and this will likely include those with the lowest preoperative functional status and worse outcomes. Information on pre- or post-morbid functional status or quality of life was also not available, although discharge destination was used as the next best outcome measure. The study period is long and encompasses many advances in endovascular technology. These may lead to better outcomes for endovascular procedures in the current environment than we have described.
Conclusions
Mortality following vascular surgical interventions for chronic limb-threatening ischaemia in patients aged 90 or over is high, with a mortality rate of 44.4% at 1 year and a median life expectancy of 1.19 years in those deemed fit enough to undergo intervention. These data are similar to those for patients over the age of 90 undergoing surgical interventions for hip fractures. Considering the benefits of vascular surgery – including pain relief, retention of functional status and ability to maintain independence – these patients should be considered for limb salvage with both endovascular and open revascularisation in appropriate patients.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(3):65-70
Publication date:
May 3, 2022
Author Affiliations:
1 Department of Vascular and Endovascular Surgery, Norfolk and Norwich University Hospital, UK
2 Department of Vascular Surgery, Cambridge University Hospitals NHS Trust, UK
Corresponding author:
Dr Eleanor Atkins
Vascular Surgery Registrar, Department of Vascular and Endovascular Surgery, Norfolk and Norwich University Hospitals NHS Trust, NR4 7UY, UK
Email: [email protected]











