ORIGINAL RESEARCH
Popliteal sciatic nerve block in the endovascular management of critical limb ischaemia: a UK single-centre experience
Davies J,1 Sammut J,2 Greenway M,3 Day C4
Plain English Summary
Why we undertook the work: Patients with poor blood supply to the leg may find it difficult to tolerate procedures to open up the vessels (angioplasty) due to severe pain such that the procedure may need to be abandoned or performed under sedation or general anaesthetic. Another option is to inject local anaesthetic around the main nerve supplying the lower leg as it passes behind the knee joint in order to “block” this nerve and relieve the pain. This study assesses how effective this is compared with similar patients who didn’t have a nerve block.
What we did: Nerve blocks were carried out in 63 patients with severe leg pain undergoing angioplasty. Pain severity was measured before and after the nerve block using a score from 0 (no pain) to 10 (worst pain). We recorded whether any sedation was given and whether any procedures were abandoned. These results were compared with 62 similar patients who underwent the same type of procedure before the nerve block procedure was introduced.
What we found: Patients receiving the nerve block had significantly less pain during the procedure, and no procedures were abandoned, unlike in the group with no nerve block where three procedures were abandoned due to pain. With the nerve block, fewer patients needed sedation and, when it was required, the dose was smaller.
What this means: Patients with severe leg pain due to poor blood supply appear to benefit from a nerve block behind the knee to reduce their pain severity, reduce the need for sedation and reduce abandoned procedures due to pain.
Abstract
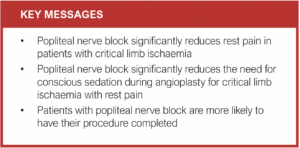
Objective: This study aims to assess the safety and efficacy of the use of popliteal nerve block (PNB) in the endovascular management of patients with critical limb threatening ischaemia.
Design: Single-centre retrospective observational study.
Methods: All patients with rest pain who received PNB from March 2018 to August 2021 were included. Pain scores were recorded before and after block using a visual analogue scale (VAS). Requirements for analgesia or sedation, complications related to nerve block, and level of intervention were recorded. Results were compared with a historical cohort of patients prior to implementation of nerve blocks.
Results: 68 nerve blocks were performed in 63 patients (M:F 46:17) of mean age 71.7 years (range 43–91). All patients were Fontaine classification III–IV. Sonographically, all nerve blocks were technically successful. The mean VAS pain score was 8.2 pre-block, reducing to 0.3 (p<0.0001) post-block. There were no complications related to the block. Four patients required supplementary analgesia for breakthrough ischaemic pain. Compared with the historical comparison group of patients (n=62), there was a statistically significant reduction in the requirement for conscious sedation (p=0.004) and no procedures were abandoned due to pain compared with three in the historical comparison group (p=0.034).
Conclusion: Popliteal sciatic nerve block is safe and effective in patients with critical limb threatening ischaemia undergoing lower limb endovascular intervention, significantly reducing the need for conscious sedation and risk of procedural abandonment.
Introduction
When performing endovascular treatments in patients with critical limb threatening ischaemia (CLTI), providing safe and effective pain management can be challenging, particularly with the increasing length and complexity of such procedures. The patient often needs to lie flat for a prolonged period and needs to be still through critical parts of the procedure. In addition, the patient will often require bed rest following the procedure to reduce access site complications. Patients with CLTI may hang their leg in a dependent position in order to bring their pain to a more tolerable level. This is not possible during the procedure and pain is often exacerbated.
Conscious sedation (CS) using a combination of opioid and benzodiazapine has been used, but can be ineffective within safe dose limits and the patient may become agitated or confused such that the procedure has to be abandoned.1 Airway, respiratory and cognitive risks associated with CS require additional staff to safely administer and monitor the effects of these medications.2 More invasive alternatives to control CLTI-associated pain include spinal, epidural and general anaesthesia, but there is variability in anaesthetic availability within interventional radiology (IR) units across the UK, and patients often have multiple co-morbidities increasing the risk of anaesthetic.3 This is of particular importance with current targets for treatment of CLTI.4
Regional nerve block techniques have been performed by anaesthetists for many years. This is an attractive option for treating patients with CLTI-associated pain, and several studies have reported the use of nerve blocks to facilitate endovascular intervention in such circumstances.5-8 This study describes the development of a popliteal nerve block (PNB) service within IR with support from anaesthetic colleagues, and aims to assess the safety and efficacy of PNB in endovascular treatment for CLTI in comparison with a historical cohort of patients treated before the introduction of the service.
Methods
Study design and data collection
This is a single-centre retrospective observational study of patients with CLTI undergoing PNB to facilitate endovascular intervention in a tertiary referral regional vascular unit from March 2018 to August 2021. No formal ethics board approval was required because this is a well-established anaesthetic technique routinely carried out in other clinical settings and was instituted as a quality improvement practice. Inclusion criteria were patients with CLTI-associated pain undergoing lower limb revascularisation. The only strict contraindication was any documented reaction to local anaesthetic agents, of which none were recorded. Given the nature of the work and logistics within the department and gradual implementation of PNB, not all patients with CLTI over the study period were captured.
Technical success was defined as sonographic visualisation of adequate tumescence around the nerves in the popliteal fossa. Clinical success was determined by a reduction in objective pain score taken pre and post PNB using a visual analogue scale (VAS) on a scale from 0 (no pain) to 10 (worst pain). VAS was chosen because it is a standard valid and reliable method commonly used to evaluate pain. Clinical failure was defined as a requirement for supplementary CS. A two-tailed t-test was used to compare pre and post block. Data including the use of any supplementary analgesia and sedation, complications and success of the intervention were recorded.
A historical comparison group of 62 patients was created using a key word search of the radiology information system (CRIS) for consecutive patients undergoing lower limb angioplasty for rest pain from 2017 to 2018. Given that this was a retrospective study, there was no formal randomisation process. Data collection in both groups was performed by the study authors, who also followed up patients to the point of discharge for any complications that may have arisen as a result of block. Day case patients were discharged when they had fully recovered sensation and mobilised successfully. Inpatients were discharged when assessed to be ready by the vascular surgeons. Data were collected and analysed on Microsoft Excel (Microsoft Corporation, 2010). Means and standard deviations were calculated and, where appropriate, numerical data were compared with a two-tailed t-test. A χ2 test and Z test was used where suitable for categorical data.
Implementation of the nerve block service
Following approval within the radiology department, proctoring was provided to a single radiologist (CD) by an anaesthetist (MG) for the first 10 cases of PNB. Once all involved were confident that the procedure could be done safely, it was performed by the same consultant radiologist who then taught the technique to eight other IR consultants and IR trainees within the department. This continued in the form of mentoring until all involved were comfortable performing the procedure. The consultants continue to support each other when necessary. No formal competence assessment was undertaken for consultants, but IR trainees are assessed using the Royal College of Radiologists (RCR) Radiology Direct Observation of Procedural Skills (Rad-DOPS) framework. PNB is now used regularly by all nine IR consultants and a standard operating procedure (SOP) has been written. This includes the consent process, complications, a recommended standard report and guidelines for the management of local anaesthetic toxicity.
Performing the block
Following informed consent, the PNB is performed within the IR suite with the patient on their bed in the lateral decubitus position with the index limb uppermost. The area is prepared and draped using sterile precautions and ultrasound used to identify the sciatic bundle within the popliteal fossa and its division into tibial and common peroneal nerves. Initially, a Siemens Helx Evolution ultra-sound machine (Siemens Healthcare GmbH) was used, using a high frequency probe (9–4 MHz) on ‘nerve-tint’ setting, to allow optimal visualisation of the nerve. Specific ‘nerve’ settings were subsequently installed on other ultrasound machines within the department.
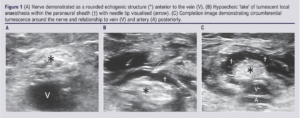
The sciatic bundle presents itself in the transverse view as a round echogenic structure lying superficial to the popliteal vein and artery (Figure 1A). Imaging should identify the bifurcation of this bundle into the tibial and common peroneal nerves with the block performed just proximal to it. This is important to identify because it may be at or above the popliteal skin crease rather than the usual place below it. A 22G Stimuplex Ultra 360 needle (B Braun Medical Ltd, UK) is inserted under ultrasound guidance, using a lateral approach, to the edge of the nerve. This can be performed with the needle either in-plane or out-of-plane to the ultrasound probe. The in-plane technique is preferred to allow constant needle visualisation with the nerve visualised transversely (Figure 1B). Once the needle is in place, local anaesthetic is injected by a second operator to allow better control and accuracy of needle placement. The local anaesthetic used was 1% prilocaine (Citanest, AstraZeneca, 10 mg/mL), aiming for a volume of 20 mL which is below the maximum safe dose of 6 mg/kg. The aim is to achieve tumescence within the paraneural sheath surrounding the nerve (Figure 1C). Following this, the needle is removed and the patient transferred to the fluoroscopy table. The PNB results in anaesthesia of the entire lower two-thirds of the leg, with the exception of the medial aspect of the leg which receives sensory supply from the saphenous nerve. The PNB is performed in patients with CLTI pain mostly affecting the foot and is therefore usually adequate.
Discharge
Day case patients on the Radiology Day Case Unit (RDCU) are normally discharged within 6 hours of the procedure. This is nurse-led following a written protocol. In addition to the standard discharge protocol, patients undergoing PNB will only be discharged once sensation has returned and the patient has mobilised safely. The discharge protocol includes provision for admitting patients for an overnight stay should they not be fit for discharge by the time the RDCU closes for the day. All patients have access to the surgical assessment unit should any problems occur following discharge.
Results
Sixty-eight PNBs were performed in 63 patients (M:F 46:17) with an average age of 71.7 years (range 43–91) from March 2018 to January 2022. Patients between PNB and comparison groups were well matched for age and sex (Table 1). Fifty-two procedures (76%) were performed on inpatients, with the other 16 (24%) performed as day case procedures. All day case patients had fully recovered sensation and movement before discharge with no delayed discharge or overnight admission. Inpatient stay following PNB ranged from 1 to 90 days with a median stay of 8 days following the procedure. All patients met criteria for a Fontaine classification of III–IV.9 All patients had CLTI-associated pain despite receiving regular analgesia including a combination of paracetamol, ibuprofen, codeine, tramadol and opiates, together with gabapentin or pregabalin if there was thought to be a neuropathic element to the pain. Forty-seven patients had additional necrosis/gangrene or ulceration. The level of intervention is shown in Figure 2.
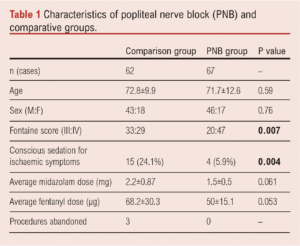
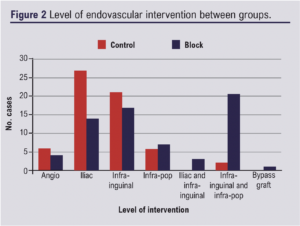
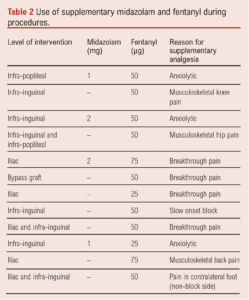
Four patients had angiography only without intervention. The block was performed on the left in 38 cases and on the right in 28. One case had bilateral PNB during the same procedure. All cases were performed prior to intervention. PNB can be performed with the patient supine and therefore could be potentially used as rescue analgesia, but this is not our standard practice. In general a 20 mL standardised dose of 1% prilocaine was given, although this ranged from 13 mL to 40 mL with an average dose of 19.98 mL. Sonographically, all blocks appeared technically successful. Four (5.9%) cases required supplementary midazolam or fentanyl (or a combination) for CLTI-associated pain (Table 2). Further cases required analgesia (Table 2) due to slow onset of block (n=1), musculoskeletal pain (n=3), as an anxiolytic to manage hypertension prior to puncture (n=3), and for CLTI-associated pain in the contralateral foot (n=1). Levels of intervention between the historical comparison and PNB groups showed a similar distribution of intervention, but with a higher proportion of multilevel disease treated in the PNB group (Figure 2). No data on length of procedure or lesion specifics were collected. When given, an average of 1.5 mg midazolam was used (range 1–2 mg), and an average of 50 μg of fentanyl (range 25–75 μg) in the PNB group.
Before PNB the mean VAS pain score was 8.2, significantly reducing to 0.3 after PNB (p<0.0001). Time of onset varied from 5 to 40 minutes and, although no strict objective measurements were taken to assess the progression of the block, the vast majority experienced effective relief within 10 minutes. The recording of the post-block VAS was not strictly timed, but was performed as near as possible to the start of the procedure. When compared with the historical group, there was a significant reduction of sedation required (p=0.004) and no procedures were abandoned (Table 1). When analgesia was required there was a trend to a decreased dose of midazolam and fentanyl, but this did not reach statistical significance. All patients were Fontaine score III or IV but, of note, there was a significantly higher proportion of patients with tissue loss in the PNB group (Table 1).
Discussion
The results of this study demonstrate a significant reduction in CS (p=0.004) and the number of procedural abandonments (p=0.034) following the implementation of PNB. PNB is a well-established technique in other settings such as foot and ankle surgery,10 although there is limited evidence of its use in the endovascular treatment of CLI. Marcus et al first described a combination of femoral nerve block and PNB in 11 patients undergoing lower limb angioplasty.5 In this study, more proximal sciatic block with or without femoral nerve blocks were used. Average VAS pain scores reduced from 10 to 3.7 and the procedure was deemed to be as safe and effective when compared with a control group of epidural anaesthesia patients. Unlike the current study, use of supplementary CS was not documented. Subsequent work by Tureli et al6 and Getikoglu and Eker7 in 30 and 10 patients, respectively, demonstrated similar safety and efficacy. In the former study, only two patients (6.6%) required midazolam as an anxiolytic. Two patients reported suboptimal pain reduction and an extra 20 mL of 1% prilocaine prior to the procedure such that no supplementary analgesia was required. In the latter paper, further nerve blocks were performed after the procedure in three patients for breakthrough pain due to distal emboli. Our results compare favourably, with four patients (5.9%) experiencing breakthrough pain treated with CS rather than further PNB.
The most recent work on nerve block in critical limb ischaemia by Danisan and Taydas randomised 60 patients to receive ultrasound-guided subgluteal sciatic nerve block or fentanyl sedation.8 Strengths of this study include formal randomisation and two measures of pain including a VAS score and FLACC (Face, Legs, Activity, Cry, Consolability). The latter score is particularly useful when patients are unable to express pain (for example, with dementia). A few patients still reported pain in the medial lower leg due to saphenous nerve supply.
Subgluteal sciatic nerve block was chosen for the randomised study8 based on data suggesting a lower volume of anaesthetic is required compared with peripheral nerve block,11 although this case series only had five patients. Despite this, the volume of local anaesthetic was 25–30 mL of 1% lidocaine/0.25% ropivacaine/epinephrine 1:400,000, which is greater than the average volume used in this study (19.98 mL). Higher volumes12 and mixing both short- and long-acting local anaesthetics13 will extend the duration of the nerve block. This may increase time to sensation and motor function recovery which is of importance for the patients admitted through the RDCU with the potential to delay discharge. Total time to recovery and mobilisation following PNB was not formally assessed in the current study, but there were no delayed discharges or unexpected admissions from the RDCU following PNB. In addition, all PNB patients were discharged before closure of the RDCU (20:00 hours), demonstrating its safe use in this setting.
In contrast to previous work, the current study includes multiple operators (both IR consultants and trainees). Only four patients (5.9%) required supplementary analgesia for ischaemic breakthrough pain, suggesting that the technique has been effectively adopted although formal assessment of the learning curve was not undertaken. Only one case had slow onset PNB most likely due to inadequately positioned tumescence, but the block was ultimately effective.
A significantly higher number of patients with a Fontaine score of IV were present in the PNB group (p=0.007). It is difficult to ascertain whether this has a bearing on the overall results, although it is encouraging to see a reduction in analgesia in a patient group with greater disease severity. Given the retrospective collection of data in the comparison group with variable documentation of CS administered, the overall benefit incurred using PNB may be higher than reported, particularly given the more complex disease in this group. The majority of PNB patients received CS for symptoms unrelated to rest pain, but it was not possible to determine if this was the case for most of the historical patients. It is reasonable to assume that, in the absence of other means of analgesia, the majority would have received sedation primarily for rest pain.
Given the benefits of PNB, it is likely that it will have a cost benefit. Patients with rest pain will be more likely to have a successful procedure first time, reducing the impact on IR service capacity given that it is less likely the patient will need a second procedure. Anaesthetic support is costly to the Trust and may impact other services, preventing them being deployed elsewhere. With PNB it is likely that more patients with CLI and rest pain can be treated as day cases without needing an overnight stay. Formal evaluation of cost effectiveness will be useful in future studies.
Despite the additional benefits PNB can bring, some potential pitfalls should be highlighted. Absence of sensation could increase the risk of adverse procedural events going unnoticed, but this is considered to be low because completion angiography will identify any potential vessel injury or embolic disease and reperfusion injury or compartment syndrome is uncommon following revascularisation for chronic limb ischaemia. An antisympathetic effect is possible with PNB that could obscure angiographic findings. This was not assessed as part of this study but, given the nature of atherosclerotic disease, this would seem unlikely.
There are several limitations to this study. The lack of formal randomisation and use of a historical control group is a limiting factor when compared with the most recent work by Danisan et al.8 Some aspects of data collection were not rigorous due to the nature of the study, such as time to onset of effective PNB and length of procedure and exact time to return of normal sensation and mobility. Historical comparison group data relies on the detail of information recorded at the time of their procedure. Recording data from multiple operators including during their learning curve may produce more varied results than if a single operator was evaluated, particularly with the relatively small number of patients. In addition, with more operators there is likely to be potential for variation in practice – for example, the small variation in the volume of local anaesthetic used in this study.
Conclusion
This study demonstrates that PNB provides effective and safe anaesthesia for CLTI patients undergoing lower limb endovascular intervention with a significant reduction in the requirement for CS and procedural abandonments. It can be performed by IRs, reducing the need for anaesthetic support. The results of this study are similar to the limited amount of previous work in this area providing additional evidence to support its introduction in other IR departments.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(3):174-179
Publication date:
May 10, 2023
Author Affiliations:
1. Consultant Interventional Radiologist, Department of Radiology, Dorset County Hospital NHS Foundation Trust, Dorchester, Dorset, UK (formerly at Royal Stoke University Hospital, Stoke-on-Trent)
2. Consultant Interventional Radiologist, Department of Interventional Radiology, Royal Preston Hospital, UK (formerly at Royal Stoke University Hospital, Stoke-on-Trent)
3. Consultant Anaesthetist, Department of Anaesthetics, Royal Stoke University Hospital, Stoke-on-Trent, UK
4. Consultant Interventional Radiologist, Department of Interventional Radiology, Royal Stoke University Hospital, Stoke-on-Trent, UK
Corresponding author:
Christopher Day
Consultant Interventional Radiologist, Department of Interventional Radiology, Royal Stoke University Hospital, Stoke-on-Trent ST4 6QG, UK
Email: Christopher.DAY@ uhnm.nhs.uk











