ORIGINAL RESEARCH
Research Priorities for Carotid Conditions: results of the UK Vascular James Lind Alliance Priority Setting Process
Luo X,1 Nortley M,1,2 Long J,3 Gronlund T,4 Bulbulia R,5 Halliday A,2 Howard DPJ,1,6 on behalf of the VSGBI Carotid Special Interest Group/James Lind Alliance Priority Setting Partnership
Plain English Summary
Why we undertook the work: More research is needed to help improve treatment and delivery of care for people with vascular conditions, but funding is limited. The Vascular Society of Great Britain and Ireland (VSGBI) undertook a Priority Setting Process (PSP) to find the most important research priorities. This will help researchers to better focus their work and funders to direct support to projects that aim to answer questions important to people with lived experience as well as vascular health professionals. This paper presents the results of this process on carotid condition-related research priorities.
What we did: Vascular patients and healthcare professionals participated in surveys and were asked to suggest priorities for vascular research. Responses were summarised and organised into nine overall vascular condition areas. Summary questions were then sent out in a second survey for scoring according to order of importance. The lists of patient and professional priorities were then combined into a shared list for discussion at a final workshop meeting where a mix of patients and healthcare professionals agreed the ‘top 10’ research priorities for carotid condition research in the UK.
What we found: A total of 481 healthcare professionals and 373 patients or carers submitted research priorities about vascular conditions, which were combined into a list of 14 priorities specifically about carotid conditions. At a final workshop involving patients, carers and clinicians, these priorities were put into a ‘top 10’ list ranked according to perceived importance. Research priorities relate to risk prediction and personalised treatment, prevention, screening and surveillance.
What this means: Carotid research priorities that are most important for people with lived experience and vascular health professionals have been identified. It is hoped that researchers and funders will focus on addressing these priorities and supporting studies in these areas.
Abstract
Introduction: Recent estimates of the prevalence of carotid plaque disease and carotid stenosis in people aged 39–79 years are 21.2% and 1.5% of the global population, respectively. Carotid artery disease and its management has one of the largest evidence-based areas of surgical practice, but several important questions remain unanswered. The Vascular Society of Great Britain and Ireland (VSGBI) in association with the James Lind Alliance (JLA) undertook a national Priority Setting Process (PSP) to identify carotid disease research priorities. This paper presents the results of this process.
Methods: A modified JLA Priority Setting Partnership was developed to gather clinician, patient and carer research priorities for vascular conditions. Consensus workshops were held to discuss clinician and patient priorities and agree a list of joint research priorities. Consensus was achieved using a nominal group technique and a ranked ‘top 10’ list of research priorities for carotid conditions was established.
Results: In the first phase (survey), 481 clinicians submitted 1,231 research priorities related to general vascular conditions. There were overlapping themes within the 1,231 priorities and, of these, 68 were carotid-specific research priorities which were reduced to six main priorities recirculated for interim scoring. In the second phase (patient and carer-led survey), 373 patients and carers submitted 582 vascular research priorities. Of these, 18 carotid priorities were reduced to 10 and recirculated for interim scoring. In the third phase (consensus workshop), clinician and patient priorities were amalgamated into 14 priorities for discussion. Finally, a ranked final ‘top 10’ list of carotid research priorities was established addressing themes including risk predication, personalised treatment, prevention, screening and surveillance.
Conclusion: The ‘top 10’ carotid-related research priorities identify areas considered to be most important from the perspective of patients, carers and healthcare professionals. Researchers can now focus their efforts on addressing these important questions and funders should increase their investment to support new studies in these areas of greatest importance.
Background
Fifteen percent of ischaemic strokes are thought to be caused by thrombotic or embolic carotid artery disease, and these carotid-related strokes are commonly fatal or disabling.1 Globally, carotid disease and specifically carotid stenosis affects an estimated 21.2% and 1.5%, respectively, of those aged 39–79 years.2 In 2016, 9.6 million cases of ischaemic stroke led to 2.7 million deaths.3
Despite a wide range of treatment options for carotid artery disease and associated guidelines, the efficacy and cost effectiveness of these different interventions are still unclear. The recent ESVS 2023 Clinical Practice guidelines on the management of atherosclerotic carotid and vertebral artery disease has identified 24 unanswered questions, which remain important for the future management of carotid artery disease.4
To ensure optimal clinical carotid management more research is needed, but funding is limited and competitive. Funding bodies seek to ensure their limited investment is directed to areas with greatest potential for improving clinical services and health outcomes.5 Priority Setting Processes (PSPs) are an increasingly popular methodology to address this issue by systematically identifying and prioritising gaps in research, and they are seen as an effective way to highlight important topics for funding consideration.6
The Vascular Society of Great Britain and Ireland (VSGBI) in association with the James Lind Alliance (JLA) undertook a national PSP for vascular conditions.7 Prior to this, there were no specific patient-led research priorities in the vascular specialist community. The aim was to survey vascular health professionals, patients and carers, identifying and prioritising the most important research priorities. This paper presents an overview of the vascular condition PSP, focusing on the recommendations for carotid-related priorities and implications for future research in this area.
Methods
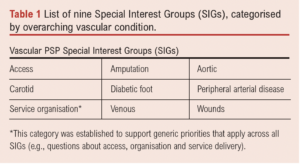
The VSGBI undertook a research priority setting process (PSP) in association with the James Lind Alliance (JLA) to identify research priorities for vascular conditions. The work was overseen by a steering committee involving representation from all the leading UK Vascular Societies and patients. Nine overarching vascular condition Special Interest Groups (SIGs) were established to help support the process and ensure that each area retained their important research priorities (Table 1). A detailed description of the process has been provided previously;8-14 however, the process is outlined again below and presented in Figure 1.
A clinician-led Delphi survey was conducted to produce a list of research priorities to reflect the opinions of vascular healthcare professionals. This was followed by a separate patient and carer-focused JLA survey to identify important research priorities from the perspective of vascular patients and carers. The two processes were then brought together at final workshops held separately for each SIG, where patients, carers and clinicians worked together to agree a shared list of ‘top 10’ research priorities.

Scope of the Carotid SIG
The remit of the Carotid SIG is to support research into the care of patients living with or affected by carotid conditions and the services that surround their treatment and management. The Carotid SIG aims to develop the list of top 10 priorities into funded carotid research studies that addresses these important areas.
Clinician-led research Priority Setting Process
Healthcare professionals were surveyed using a modified Delphi approach that consisted of:
Survey Round One: In the first round, an open-ended survey invited participants to submit their priorities for vascular research. An electronic link to the survey was emailed via the following membership bodies: The Vascular Society of Great Britain, The Society of Vascular Nurses, and The Society of Vascular Technicians of Great Britain and Ireland and the Rouleaux Club. Letters including the survey link were sent to each vascular unit registered on the National Vascular Registry (NVR) and the survey was also promoted via Twitter. Responses were collated and categorised into pathological topics and research themes by a core subgroup of the steering committee. Similar responses were amalgamated and summarised into an overarching priority. Responses considered out of scope (eg, too broad or logically unclear) were removed and remaining priorities checked for current evidence.
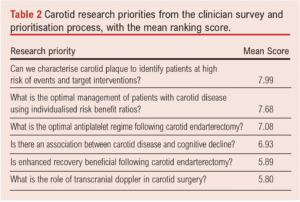
Survey Round Two: The refined list of priorities was redistributed in a second survey for scoring. Participants were asked to rate the importance of the summary priorities on scale of 1–10 (1 being the least important, 10 being the most important). This process was completed in 2018,10 and the results of clinicians’ carotid-related priorities are summarised in Table 2.
Patient/carer-led Research Priority Setting Process
Vascular patients and carers were surveyed using a modified JLA approach, with guidance from a JLA advisor, and used similar methodology as the clinician-led PSP.
Survey Round One: In the first round, patients and carers were invited to take part in an open-ended survey that asked them to submit their own research priorities. The survey was provided in paper and electronic format and advertised to UK-based societies involved with care of vascular patients. Participant packs were sent out to vascular units and included paper surveys with freepost return address and promotional materials such as posters and postcards that could be left in waiting areas. The survey was also advertised via social media (Twitter), websites and newsletters. Responses were categorised and delegated to each SIG for further review. Similar responses were amalgamated and summarised into an overarching priority. Responses considered out of scope (eg, too broad or logically unclear) were removed and remaining responses checked for current evidence.
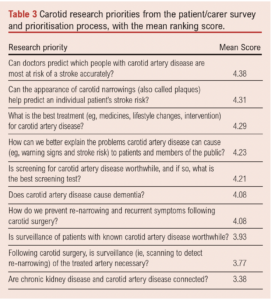
Survey Round Two: The refined list of priorities was redistributed in a second survey for scoring. Participants were invited to rate the importance of research priority using a Likert scale (scores ranged from “not at all important” to “extremely important”). This process was completed in 2020 and the results of patient and carer carotid condition priorities are summarised in Table 3.
Special Interest Group Prioritisation Workshops
For each SIG, the results of the clinician and patient/carer-led interim prioritisation processes were combined. Similar or duplicated priorities were amalgamated and any technically worded language from the clinician priorities was revised with patient input. Care was taken to ensure that the original substance of the priority remained. This process generated a refined list of joint priorities for discussion at individual SIG workshops.
The final prioritisation workshop for carotid conditions was conducted virtually on 21 September 2021 using the Zoom platform to accommodate COVID-19 restrictions. All attendees (including healthcare professionals, patients and carers) were recruited via direct contact or were approached if they expressed an interest during the initial prioritisation process. Participants were sent details of the workshop, an agenda and a list of the research priorities to be discussed in advance. Prior to the workshop, participants were asked to consider the combined list of clinician and patient research priorities shown in Table 4 and to rank them in order of importance from 1 (most important) to 14 (least important).

The workshop was led by two experienced JLA advisers, a JLA coordinator and a technical lead who were skilled in the JLA PSP process and leading such workshops. Members of the Carotid SIG attended as observers and to provide emotional support to attendees if required (they would join a separate breakout room). SIG members were not directly involved in the priority setting and had no influence over the final agreed list of priorities. Following welcome and introductions, participants were split into two breakout rooms which consisted of a mix of patients and healthcare professionals. Small group discussions were facilitated by an advisor and followed a nominal group technique to reach a consensus for an ordered list of ‘top 10’ priorities.
First round of discussion: Participants shared their top three and lowest three priorities with a brief explanation for why. This was followed by an open discussion about similarities and differences and any priorities that were not initially mentioned.
Second round of discussion: The JLA facilitator presented on-screen a potential order of priorities based on initial feedback and discussion. Participants had an opportunity to reconsider their initial placement of priorities whilst the facilitator moved priorities on screen to reflect an agreed order of priorities 1–14.
Third round of discussion: The ranked priorities of the two separate groups were combined by the lead facilitator using a geometric mean of the respective ranked positions. All participants came together as one group and the lead facilitator presented the combined results of the group rankings. Participants were then split into new groups and, again, participants had an opportunity to reconsider the order of priorities before reaching a final ranked ‘top 10’ list of carotid research priorities. As before, the ranked priorities of the separate groups were combined to form a final shared ranking.
Results
Clinician research priority identification and prioritisation
A total of 481 clinicians submitted 1,231 research priorities relating to vascular surgery in general. Of these, 68 carotid condition-related research priorities were submitted, 10 of which were excluded outright as they were too specific to single patient experience or there was no apparent question (eg, nonsensical or broad statement). The remaining 58 priorities were combined and summarised into six clinician priorities for scoring, the results of which are shown in Table 2.
Patient/carer research priority identification and prioritisation
A total of 373 patients/carers suggested 582 research priorities related to vascular surgery in general, of which 18 responses were specific to carotid conditions. After data cleaning (eg, removing nonsensical suggestions, separating out submissions with multiple suggestions and combining overlapping priorities), 10 research priorities were redistributed for scoring and the results are shown in Table 3. Prior to the workshop, the SIG team pooled clinician and patient/carer research priorities, resulting in a list of 14 for discussion (Table 4). In order to reduce the risk of bias, these priorities were randomly ordered and each assigned a letter (rather than a number).
Final prioritisation workshop
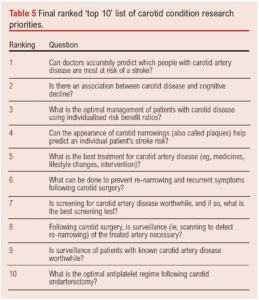
The final prioritisation process was conducted via a virtual online meeting on 21 September 2021. It was attended by eight patients and 11 healthcare professionals (stroke nurses, consultant neurologists, vascular surgeons, senior stroke fellow and a senior trainee) with five observers. The final prioritisation resulted in a final ‘top 10’ research priority list (Table 5). The priorities are ordered according to importance as determined at the workshop. There was general consensus that the list correctly represented the discussions and viewpoints which occurred in the breakout groups. Results from the participant feedback indicated that 100% agreed or strongly agreed that the process for determining the top 10 priorities was robust and fair.
Discussion
The ‘top 10’ research priorities for UK carotid conditions research have now been established. Using a modified JLA methodology, vascular healthcare professionals and patients with lived experience of carotid conditions have jointly agreed the most important priorities for future research in this area. It should be noted that there was some divergence between patient priorities which were more patient-centred, and clinician priorities which were more technical and procedural. This emphasises the importance of meaningful patient involvement and engagement in the priority setting process.
The four priorities that did not make the ranked ‘top 10’ list are still considered important. Overarching themes within the final ‘top 10’ list relate to: risk prediction and personalised treatment, prevention, screening and surveillance.
Strengths and limitations
The Vascular PSP used well established methodologies throughout, with oversight from a multidisciplinary steering committee. The Delphi method, often used in PSPs, is regarded as a flexible research technique but one that tends to focus on the identification of expert opinion.15 To mitigate this, the Vascular PSP sought the input of the JLA who provide a transparent and structured framework that emphasises patient participation in PSPs, with patients having an equal voice to clinicians and researchers in influencing the research agenda.16,17 It is possible that the modified approach of having two separate processes before bringing the clinician and patient views together may have resulted in a different ‘top 10’. However, during the amalgamation process there was already plenty of overlap with similar priorities and the format of the final workshops did establish shared priorities.
Due to the nature of survey data collection there is potential for responder bias,18 and consideration was given to whether responses would be adequately reflective of the opinions of people with lived experience of carotid conditions and those treating them. Under-representation is recognised as a limitation of many PSPs,19,20 and therefore there may have been potentially relevant priorities not submitted and consequently not considered within the analysis. However, the value of PSPs is not in their universal coverage but in eliciting some new insight and perspectives, especially from people with lived experience.
The Vascular PSP sought to minimise this risk in a number of ways. The survey was made available in electronic and hardcopy format (with freepost address) and it was promoted via a number of platforms with the help of affiliated charity groups and organisations who regularly work with the population targeted for input. Furthermore, the introduction of SIGs meant that each vascular condition area had a dedicated review of responses by a group of interested professionals and patients who could highlight if there were any expected topic areas missing.
Most workshop participants found the use of a virtual platform acceptable, although it is recognised that potentially lack of access to IT may have limited participation and altered representation. On the other hand, the virtual platform meant patients did not have to travel, and this may have made the workshop more accessible for some patients. Positive comments collected from the feedback survey following the final workshop demonstrated that clinicians and patients found the process of discussing priorities in mixed groups a positive and worthwhile experience. It gave participants an opportunity to hear about the experiences of others and to reassess their initial judgments.21 Although the mixed discussion groups were not strictly balanced in terms of patient attendance, this was carefully moderated through the skilled JLA facilitators who ensured that patient participants were regularly included and asked for their views. Some participants expressed a preference for a different ranking order of the priorities, but this is not uncommon for PSPs and is a known factor of a consensus approach.
Implications for future research
The carotid conditions priorities now provide researchers with essential guidance on where best to focus their efforts in the immediate and long term. Studies and projects should now be developed to address these important priorities and we call on funders to recognise and support the delivery of this work.
Conclusion
The Vascular PSP has established a ‘top 10’ list of priorities for UK carotid conditions research from the shared perspective of vascular patients, carers and health professionals. Researchers and funders can confidently invest resources into these areas of carotid conditions research with reassurance that they are clinically relevant and of practical importance to patients.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(3):134-140
Publication date:
April 20, 2023
Author Affiliations:
1. Department of Vascular Surgery, Oxford University Hospitals NHS Trust, Oxford, UK
2. Nuffield Department of Surgical Sciences, John Radcliffe Hospital, University of Oxford, Oxford, UK
3. Vascular PSP Coordinator, Hull York Medical School, University Road, Heslington, York, UK
4. Adviser at James Lind Alliance, National Institute for Health Research (NIHR)
5. Clinical Trial Service Unit and Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK; Medical Research Council Population Health Research Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK
6. Wolfson Centre for Prevention of Stroke and Dementia, Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, UK
Corresponding author:
Dominic PJ Howard
Wolfson Centre for Prevention of Stroke and Dementia, Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, UK
Email: dominic.howard@ ndcn.ox.ac.uk











