ORIGINAL RESEARCH
Restructuring of the UK Vascular Services: does the hub versus spoke model affect patient mortality in ruptured abdominal aortic aneurysms?
Nyamedom-Bonsi TA,1 O’Malley OT,1 Abbud N,1 Safar M,1 Neequaye SK1
Plain English Summary
Why we undertook the work: Ruptured abdominal aortic aneurysms are a serious, often fatal, condition. They require immediate specialist intervention. The Get It Right First Time programme recommended restructuring of UK vascular services. This led to a central hub site which would act as the referral centre for surrounding spoke sites for vascular pathology.
What we did: A retrospective review of data from 110 patients presenting to hub and spoke sites with ruptured abdominal aortic aneurysms from 2017 to 2020 was undertaken. We then investigated the possibility of a link between mortality and the presenting site.
What we found: Forty-one patients presented to the hub site and 69 patients presented to a spoke site. The overall mortality rate was 53%. There was no link between presenting site and patient death.
What this means: Our study is aligned with other published data which favour the centralisation of vascular services and therefore the transfer of patients to a specialist hub site.
Abstract
Background: Ruptured abdominal aortic aneurysms (AAA) are a frequently fatal vascular condition. The centralisation of vascular services in the UK was driven by the positive volume–outcome relationship witnessed within vascular surgery and other major surgical specialities. In 2018, The Get It Right First Time (GIRFT) programme officially recommended the restructuring of vascular services in England to a hub and spoke model where AAA repairs should be performed in higher volume centres, the hub sites. This study aims to assess the mortality rates in patients presenting at hub versus spoke sites in the Merseyside region.
Methods: We conducted a retrospective review from 1 January 2017 to 31 December 2020, identifying 110 patients with a ruptured AAA presenting to hub and spoke sites. We determined if there was any association between mortality and the presenting site.
Results: Forty-one patients presented to the hub site (Royal Liverpool University Hospital) and 69 patients to the spoke sites. 81% underwent operative intervention and 19% died in Accident and Emergency or were palliated. 57% of those who underwent an intervention survived. The overall mortality rate in hospital was 53% (58 patients). There was no association between mortality and transfer from a spoke site (p=0.585).
Conclusion: This study is concordant with further published data supporting the centralisation of services for ruptured AAA.
Introduction
Ruptured abdominal aortic aneurysms (AAA) are a frequently fatal vascular condition with a mortality rate of up to 80%.1 The Office for National Statistics (ONS) identified over 4,000 deaths from aortic aneurysm and dissection in England and Wales in 2019, with the highest prevalence in men over 65 years old.2 Current management involves either open surgical repair or endovascular aneurysm repair (EVAR).
The drive for centralisation of vascular services and the move towards hub sites was supported by the positive volume–outcome relationship noted within peripheral vascular surgery.3 A study looking at AAA repairs from 2006 to 2018 in England highlighted that volume had a profound impact on outcomes – more specifically, open repairs compared with EVAR.4 The current literature suggests that patient, hospital and surgeon factors all significantly influence outcomes such as mortality in patients presenting with a ruptured AAA.5 In 2018, the Get It Right First Time (GIRFT) programme recommended the restructuring of vascular services throughout the NHS in England.6 The implementation of a network consisting of a ‘hub and spoke site’ would primarily aim to reduce mortality for those patients with potentially fatal conditions such as ruptured AAA. This centralisation of vascular procedures would provide 24/7 care for elective and, more importantly, emergency procedures.6,7 A systematic literature review confirmed the notion that AAA repairs (elective and ruptured) should be performed at higher volume centres due to reduced mortality rates.8 Therefore, the reconfiguration of vascular services should positively influence the quality of patient care and outcomes.9 The Society for Vascular Surgery recommends target times of less than 90 min from presentation to treatment: 30 min diagnosis, 30 min transfer and 30 min door to intervention time.10
Current literature debates the effect of patient transfer from community to tertiary centres on mortality rate with a ruptured AAA. Some evidence suggests that, when patient-specific factors are taken into account, patient survival is lower in those being transferred.11 Other studies show that that there is no effect on mortality based on operative site, but patients transferred have a higher risk of complications.12 Morbidity rather than mortality is influenced in those studies.
The purpose of this study was therefore to investigate if there was a correlation between mortality and presentation site in patients with a ruptured AAA.
Methods
We conducted a retrospective review of patients presenting with a ruptured AAA to hub and spoke sites in the Merseyside Region from 1 January 2017 to 31 December 2020.
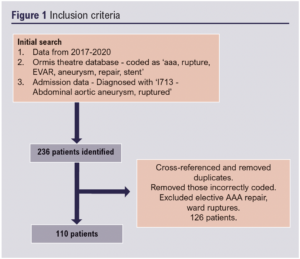
The theatre database was used to search for patients who had been coded as having ‘aaa, rupture, EVAR, aneurysm, repair, stent’. Admission data were used to search for patients by looking at those diagnosed with ‘I713 – Abdominal aortic aneurysm, ruptured’. Our initial search generated 116 emergency coded AAA repairs and 120 diagnosed on admission with ruptured AAA. We cross-referenced for any duplicates and excluded elective AAA repair, ward ruptures and those who had been incorrectly coded. This resulted in 110 relevant patients who had presented to the emergency department (ED) with a ruptured AAA over the 4-year period (Figure 1).
At initial assessment, demographics (age, gender) were recorded and the location of the presenting site. We also recorded whether a patient had a known AAA in their past medical history or if this was a new presentation. Intervention was separated into those who underwent an operation and those who were deemed inoperable, therefore palliated as a result. Method of repair, open or EVAR, for those who had an intervention was noted.
For all patients from spoke and hub sites, arrival to ED time, diagnosis to ruptured AAA time and arrival to theatre time was identified. The time for a spoke site patient to be transferred to the hub was also recorded. Diagnosis time was defined as the time of computed tomography (CT) scan.
Our primary outcome was to investigate if there was any significant difference in mortality in patients with a ruptured AAA presenting to a hub site over a spoke site. The secondary outcome was whether the overall length of pathway time from presentation to ED to intervention affected mortality. We also looked specifically at whether spoke sites target of <90 min from door to intervention influenced mortality.10
Data were collected, anonymised and entered into a standardised spreadsheet (MS Excel, Microsoft, USA). The association between presentation site and mortality was analysed with χ2 testing using SPSS statistics package (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 21.0. Armonk, New York, USA). A significant difference was defined by p<0.05.
Spoke site mortality rates were analysed using a χ2 test.10 The correlation between length of time from presentation to intervention on mortality was calculated using χ2 testing. Significance was defined as p<0.05.
Results
A total of 110 patients were identified. The mean age was 76 years (range 60–92) and 78% were male. Forty-one patients presented to a hub site (Royal Liverpool University Hospital) and 69 patients were transferred from the surrounding spoke sites (A, B, C). These sources of referrals from spoke sites included A:18, B:24 and C:18 and seven out of region.
Thirty-two patients had a previous AAA diagnosis and 56 patients were new presentations. Eighty-nine patients (81%) underwent operative intervention (76 patients open repair and 13 EVAR). Twenty-one patients (19%) died in ED or were palliated at admission.
Mortality
The overall mortality rate in hospital was 53% (58 patients). 47% (52 patients) survived after admission and were subsequently discharged from hospital. 57% of the 89 patients who underwent an intervention (open repair/EVAR) survived and 43% of patients died. The remaining 21 patients who did not undergo any intervention had a mortality rate of 95%. One patient survived to discharge.
There was a 55% mortality rate for those presenting to spoke sites compared with 66% mortality at the hub site. There was no association between the mortality rate and presenting sites (p=0.585).
Timings (Figure 2)
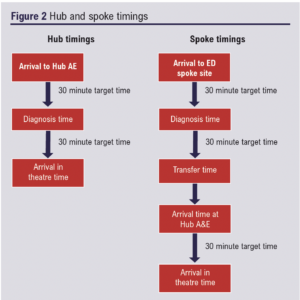
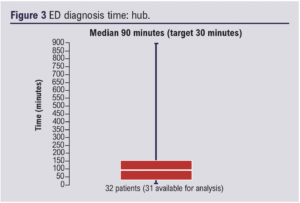
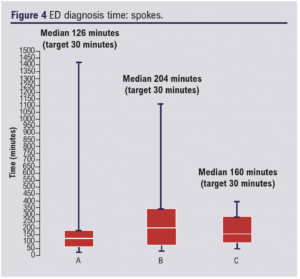
ED diagnosis time was recorded with a target time of 30 min; 83 patients were available for analysis. The median time for the hub site was 90 min (Figure 3). The median diagnosis time for the spoke sites also exceeded the target 30 min with three referring sites having times of A: 126 min, B: 204 min, C: 160 min (Figure 4).
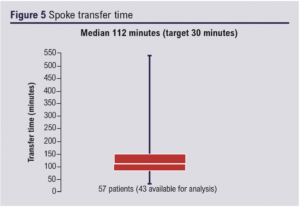
Transfer from spoke sites had an average time of 112 min, exceeding the target time of 30 min (Figure 5).
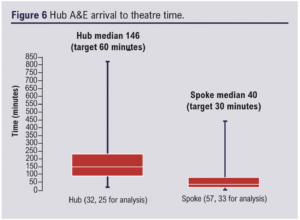
Arrival at hub A&E to theatre time was measured for both the hub site and spoke sites. Hub sites had a median time of 146 min, which exceeded the target of 60 min (30 min diagnosis time and 30 min arrival in theatre time). When measuring spoke sites, we looked at arrival at hub A&E after initial spoke site ED arrival, diagnosis and transfer time. Therefore, arrival at hub A&E to theatre time had a target time of 30 min. This time was exceeded with a median of 40 min (Figure 6).
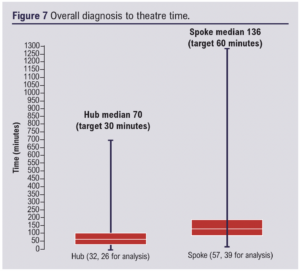
Overall diagnosis to theatre time had a median time for patients presenting to the hub of 70 min (30 min target) and for those presenting to the spoke sites of 136 min (60 min target) (Figure 7).
A comparison of overall targets from A&E arrival to intervention time for hub (60 min) and spoke sites (90 min) showed no significant association with mortality (p=0.585).
Discussion
Our study supports recently published UK data looking at outcomes in ruptured AAA following the centralisation of vascular services. Leighton et al reported no difference in 30-day mortality following ruptured AAA in South-West England post centralisation.13 Proctor et al found no difference in AAA mortality post centralisation but did find complications to have increased; however, they recommended prudent interpretation of their data given the small sample size.14
International studies appear to reinforce the UK data. Tripodi et al analysed the impact of centralisation in high volume centres in Catalonia for AAA repair.15 Their study supported this restructuring as it highlighted reduced mortality and length of stay.
An International Registry looked at the variation of vascular networks across 11 countries and the subsequent patient outcomes following repair of ruptured AAA. They concluded that perioperative mortality was lower in high-volume centres and suggested restructuring could improve this.16
The volume and outcome relationship in abdominal and vascular surgery was a significant driving factor in formulating specialist hub sites.8 It is well established, particularly in the USA, that hospital mortality is influenced by surgeon and hospital volumes.17,18 Increased volume centres result in reduced mortality rates. The mortality rates in an open AAA repair is significantly lower at specialist hub sites when both volumes of surgeons and hospitals are higher.12 Our study supports this narrative.
When managing a ruptured AAA, the Society for Vascular Surgery sets a target time of less than 90 min: 30 min diagnosis, 30 min transfer and 30 min door to intervention time.10 These targets were used as the framework for the secondary outcome in our study. Our secondary outcome showed no significant association of door to intervention time with mortality rate between spoke and hub sites.
Strengths and limitations
A strength of our study is the initial dataset and subsequent analysis of patients presenting with ruptured AAA from all sites across the Merseyside region. We were able to look at patient demographics, timings, previously diagnosed AAAs and type of intervention. This enabled us to establish the significant outcomes within our study whilst providing a foundation for future discussions.
This study has limitations. First, our small sample size limits definitive conclusions. However, our findings add weight and support to the currently available UK and international data focusing on pre- and post-centralisation outcomes. As this is a retrospective study with data collected from theatre and HES coding, it is possible that patients may have been missed or coded incorrectly.
A limitation of our study is that we have no data on patients with ruptured AAA at spokes who were not transferred. Patient transfer and intervention is primarily based on clinical judgement and/or professional opinions and there is ongoing debate regarding criteria for transfer of patients with ruptured AAA.19 The impact of transfer delays on mortality in patients with ruptured AAA is controversial.11,19-21
We also appreciate that our data highlight a bias towards open repair over EVAR, despite current data recommending EVAR for ruptured AAA.22,23 This is a reflection of the availability of hybrid theatre for emergency EVAR, particularly out of hours.
Lastly, some studies also focus on the concept of permissive hypotension during management of a ruptured AAA.24-26 This is recommended by NICE during regional transfer of a patient with a ruptured AAA.25 Fluid resuscitation is key preoperatively; however, if done aggressively before intervention, it has been shown to increase a patient’s risk of death.24 Our study obtained systolic BP on arrival, but the study design resulted in difficulty establishing volume of fluid administered to patients and subsequent preoperative blood pressures and therefore was not presented.
Conclusion
Our study supports the published data detailing that centralisation of vascular services has no detriment on mortality in patients with ruptured AAA. These findings support the transfer of patients to centralised high-volume sites whilst acknowledging various factors that influence arrival to intervention time. Further research and development to optimise this hub and spoke model throughout the UK may be beneficial.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(3):149-153
Publication date:
April 21, 2023
Author Affiliations:
1. Department of Vascular Surgery, Royal Liverpool University Hospital, Royal Liverpool and Broadgreen University Hospitals Trust, Liverpool, UK
Corresponding author:
Theona Nyamedom-Bonsi
Royal Liverpool University Hospital, Prescot Street, Liverpool L7 8XP, UK
Email: theonabonsi14@ gmail.com











