ORIGINAL RESEARCH
Short-term effects of the COVID-19 pandemic on vascular surgical training in Scotland: a trainee’s perspective
Walter AM,1 Bradley NA,2 Guthrie GJK,3 Suttie SA3
Plain English Summary
Why we undertook the work: The COVID-19 pandemic has affected surgery in many ways. Firstly, the NHS had to stop all routine non-urgent operations for patient safety, to maximise space for hospitalised COVID-19 patients and to minimise transmission of the virus. This has meant that surgeons in training have had less exposure to surgical procedures and this could cause potential problems in providing enough surgeons in the future.
What we did: We sent a survey to all training surgeons in vascular surgery in Scotland to compare their experiences in operating between two different time periods, before and during COVID-19. We examined the data and looked for significant changes in operating for the trainees for different key vascular operations. We also looked to see if other parts of the job were affected, such as examinations and courses.
What we found: We found that there was no significant change in the type and number of operations in which trainees were involved. They were affected by redeployment, rota changes, cancellation of examinations and courses.
What this means: Vascular surgical trainees have not had a significant change to their work, especially compared with other surgical trainees. All trainees have been able to progress through their year and reach their targets and requirements. This is promising for the future to provide enough consultant surgeons.
Abstract
Background: The COVID-19 pandemic has caused significant disruption to surgical training worldwide due to several factors, including the postponement of elective operating. This study aimed to evaluate the impact of the COVID-19 pandemic on vascular surgery trainees in Scotland.
Methods: A voluntary questionnaire was offered to all specialty trainees in vascular surgery in Scotland, comparing two one-year periods before (period A, 1 March 2012 to 28 February 2020) and during (period B, 1 March 2020 to 28 February 2021) the COVID-19 pandemic. The questionnaire assessed multiple areas including demographics, annual review of competence and progression (ARCP) outcome, logbook completion and supervision level of eight index procedures.
Results: All of the 11 eligible trainees completed the survey (100% response rate). No trainee had their ARCP outcome affected by the pandemic. Six (54.5%) had courses affected and seven (63.6%) were subject to rota changes. Of the eight index procedures, five procedures (62.5%) trended towards fewer procedures performed in period B (emergency open aneurysm repair (OAR), emergency endovascular aneurysm repair (EVAR), carotid endarterectomy (CEA), vascular access, percutaneous transluminal angioplasty (PTA)) and three (37.5%) trended towards more procedures performed in period B (elective OAR, elective EVAR, lower limb bypass), though these trends did not reach statistical significance. Four (50%) of the index procedures were performed more frequently as primary operator.
Conclusions: The pandemic has forced changes in surgical training but vascular trainees in Scotland have had minimal negative impact. This needs to be maintained for the trainees to progress in their surgical
Introduction
The COVID-19 pandemic has caused major disruption to clinical practice across the entire health service. Major changes to service delivery occurred across all specialties with the introduction of the national lockdown in the UK in March 2020. At the peak of the pandemic, overwhelming pressure caused staff shortages in all areas, reduced intensive care capacity and depleted theatre resources, leading to a government-mandated suspension of all non-urgent elective surgery for a minimum of three months.1 Doctors of all grades and specialties were redeployed to critical areas, whilst outpatient clinics and multidisciplinary meetings (MDM) were significantly reduced and delivered virtually where possible.2 Many courses and conferences were cancelled, and professional examinations postponed or restructured.2 Some of these developments may show long-term benefit to service delivery – for example, the use of telemedicine and virtual clinics. However, these organisational changes have been anecdotally reported as causing detrimental effects on surgical training and trainee progression across all specialties, with 66% fewer training opportunities for surgical trainees.3 This effect of the COVID-19 pandemic is significant as it may affect future recruitment and retention of surgical trainees and have a negative impact on those currently in training, hampering progression towards completion of training and certification.2,4
Vascular surgery has a large volume of cases categorised as urgent or emergency.5 Like all other surgical specialties, elective operating in vascular surgery was also restricted based on local resources and guidance from the Vascular Society of Great Britain and Ireland (VSGBI), which is the basis of many training opportunities for trainees.5,6 For vascular trainees in the UK, the total number of elective procedures fell significantly from an average of 3000 to an average 1000 cases between March and June 2020 on the online surgical logbook used in the UK, elogbook.7
The aim of this study was to assess if and how the training opportunities for current vascular trainees in Scotland have been affected by the COVID-19 pandemic.
Methods
A survey of all specialty surgical trainees with a national training number (NTN) in vascular surgery in Scotland was carried out with a voluntary questionnaire using Microsoft Word (Appendix 1 online at www.jvsgbi.com). The trainees were at least three years into their surgical training in the UK (ST3+). The survey assessed training over two time periods: before COVID (period A, 1 March 2019 to 28 February 2020) and during the COVID pandemic (period B, 1 March 2020 to 28 February 2021). A total of 14 trainees were invited to complete the survey. The survey was sent to trainees via email and subsequently returned directly and analysed by one of the authors (AW). The questionnaire consisted of drop-down options and trainees clarified further information where required in email responses. The survey was voluntary but, in order to maximise the response rate, up to five reminders were sent to individual trainees who had not responded between 18 February and 18 April 2021.
The questionnaire assessed multiple areas including demographics; logbook entries and operative supervision levels; redeployment; rota changes; access to outpatient clinics; access to MDM; impact on Intercollegiate professional examinations (Fellowship of the Royal College of Surgeons, FRCS), annual review of competence and progression (ARCP) outcomes, out of programme plans and consultant appointment. Logbook completion was specifically assessed in relation to case numbers at each supervision level for eight index procedures: elective open aneurysm repair (OAR), emergency OAR, elective endovascular aneurysm repair (EVAR), emergency EVAR, lower limb bypass, carotid endarterectomy (CEA), vascular access and lower limb percutaneous transluminal angioplasty (PTA). Initially, the questionnaire grouped the number of operations into five separate groups; however, we proceeded to update our methodology in order to collect raw numbers. These were collected by the Scottish Training Programme Director (TPD) via the e-logbook and were anonymised. This allowed more accurate analysis as some procedures were performed in small numbers. Trainees were subgrouped by seniority into ‘Senior’ (at 7th year of specialty training (ST7) or above during any part of the study period) and ‘Junior’ (below ST7 level for the entire study period) for analysis. These subgroups were decided due to the split in the new intercollegiate surgical curriculum programme (ISCP) which determines competency in early and late stages of training, respectively. Supervision levels were subgrouped into ‘Operator’ (performed, supervised-trainer unscrubbed, supervised-trainer scrubbed) and ‘Assistant’ (assisted) for analysis.
Paired t-tests were used to assess the difference between trainees’ operative exposure in the two study periods and a χ2 test was used to assess the difference between the supervision level of the procedures during the two study periods. Statistical significance was defined as p<0.05. Statistical analyses were carried out using SPSS Statistics v27.0 (IBM, New York, USA).
Results
Of the 14 trainees invited to complete the survey, 11 were eligible and the remaining three were ineligible as they did not rotate through vascular surgery during the study period. Survey completion rate was 100%. There were four senior trainees and seven junior trainees. In total, the trainees reported their experience from five different vascular units across Scotland: three units in East Scotland and two units in West Scotland. No trainee had their ARCP outcome affected by the COVID-19 pandemic. One trainee (9.1%) had to alter plans for a fellowship prior to certificate of completion of training (CCT) (cancelled plans but successful at substantive consultant level appointment) and in one case (9.1%) the plans to sit the FRCS examinations were disrupted due to postponement of Part B of the examination. Six trainees (54.5%) had plans for courses disrupted, one (9.1%) was redeployed to intensive care for three weeks to provide cover for COVID-19 specific services and seven trainees (63.6%) experienced changes to their working pattern in the form of a new rota without redeployment to providing non-vascular cover. Two (18.2%) trainees found this rota change worse than their original, one (9.1%) found it was improved and four (36.4%) did not feel it made a significant difference to their working pattern. Outpatient clinic activity appeared to be minimally affected, and all trainees attended at least one face-to-face clinic during both time periods with no significant difference between the two periods (period A 14 vs period B 15, p=0.91). There was no significant difference in MDM attended between periods A and B (11 vs 11, p=0.05), but seven (63.6%) trainees reported a shift from in-person to virtual meetings.
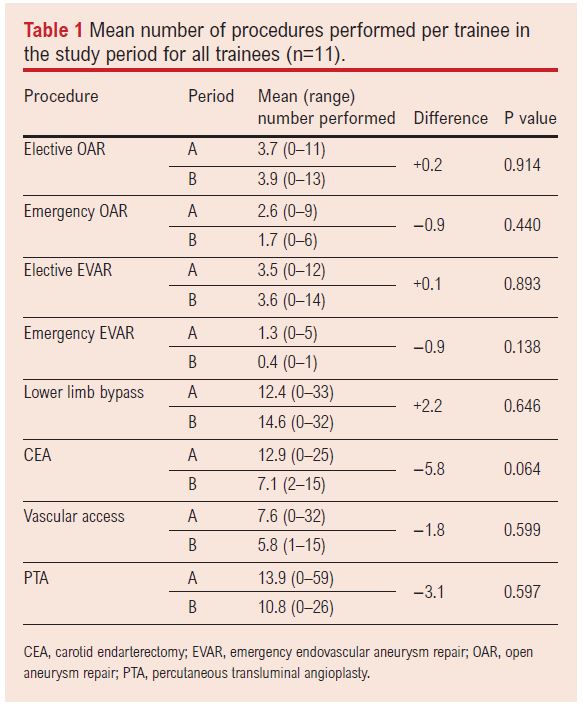
Table 1 shows the mean number of cases performed per trainee in periods A and B across the entire trainee cohort. There was a trend towards fewer CEA procedures being performed in period B (12.9 vs. 7.1, p=0.064), although this did not reach statistical significance. Of the eight index procedures, there was a trend towards fewer procedures being performed in five of the index procedures (62.5%) in period B (emergency OAR, emergency EVAR, CEA, vascular access, PTA) and three (37.5%) showed a trend towards more procedures being performed in period B (elective OAR, elective EVAR, lower limb bypass), although these trends did not reach statistical significance.
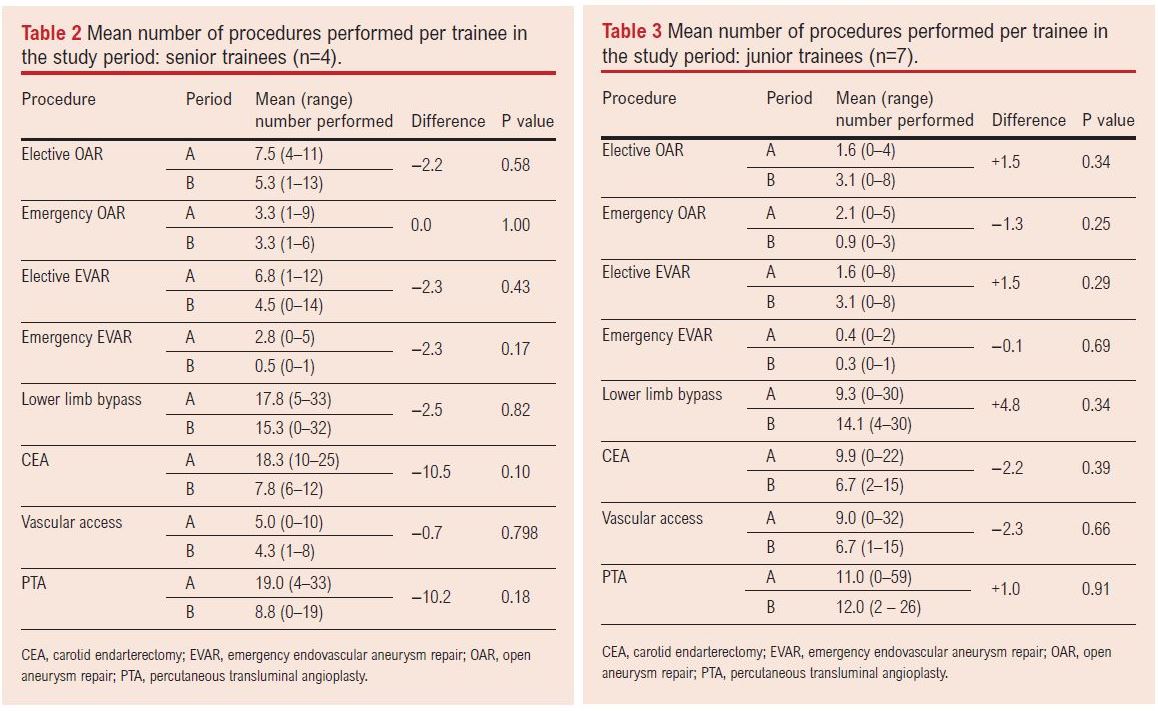
Tables 2 and 3 show the mean number of cases performed per trainee in periods A and B across the senior (n=4) and junior (n=7) trainee subgroups. In the senior trainee subgroup, seven (87.5%) of the index procedures trended towards fewer procedures performed in period B (elective OAR, elective EVAR, emergency EVAR, lower limb bypass, CEA, vascular access, PTA) and one (12.5%) was unchanged (emergency OAR). In the junior trainee subgroup, four (50.0%) of the index procedures trended towards fewer procedures performed in period B (emergency OAR, emergency EVAR, CEA, vascular access) and four (50.0%) trended towards more procedures performed in period B (elective OAR, elective EVAR, lower limb bypass, PTA). These subgroup trends did not reach statistical significance.
In order to adjust the analysis to account for the effect of trainees being out of programme during part of the study, the number of months each trainee spent in training during periods A and B was recorded. The number of procedures per month of training was calculated and results compared between periods A and B, as shown in Table 4. The results were largely similar to the unadjusted analysis, with the same five index procedures showing a decrease in numbers performed. Two procedures (elective OAR and lower limb bypass) increased in frequency in the unadjusted analysis and one (elective EVAR) decreased slightly in frequency compared with an increase in the unadjusted analysis. Despite these trends being observed, none of the comparisons reached statistical significance (p>0.05 for all comparisons).
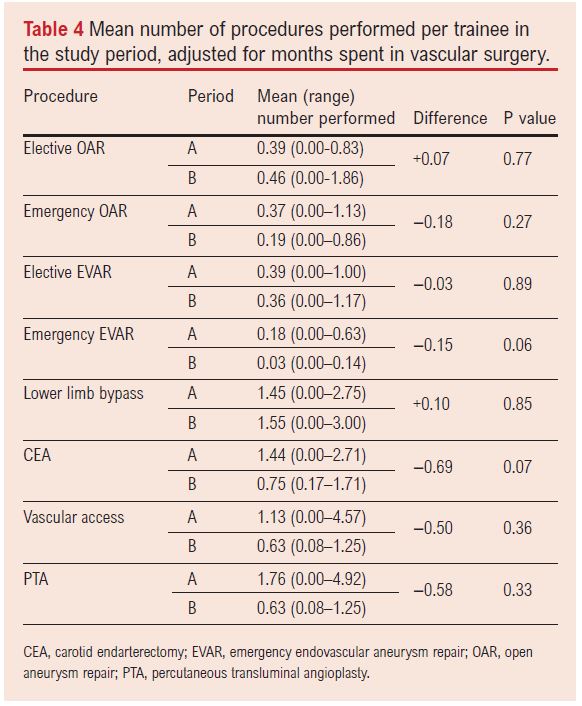
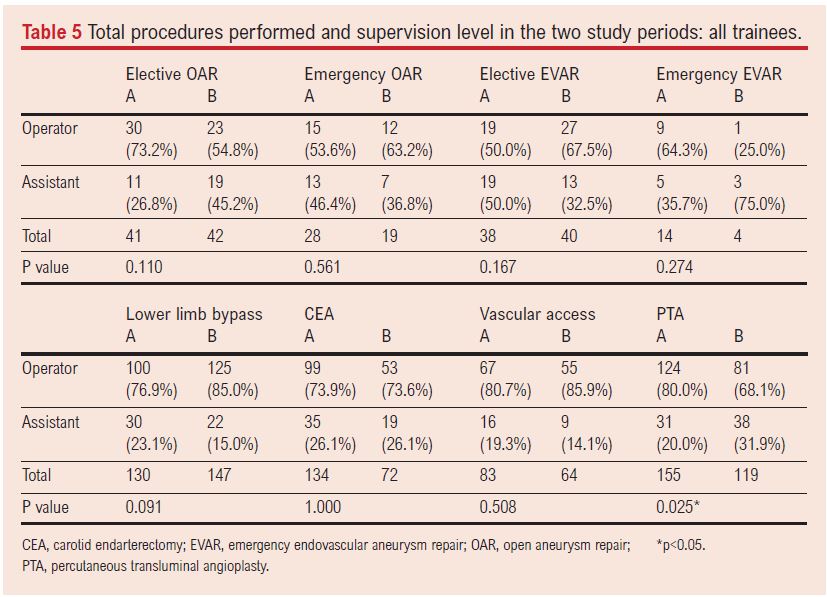
Table 5 shows the number of procedures performed in the two study periods and the supervision level at which they were performed. Significantly fewer PTA procedures were performed as primary operator in period B than in period A (68.1% vs 80.0%, p=0.026). Of the remaining index procedures, three (37.5%) were less frequently performed by trainees as primary operator in period B (elective OAR, emergency EVAR, CEA) and four (50.0%) were more frequently performed by trainees as primary operator in period B (emergency OAR, elective EVAR, lower limb bypass, vascular access). Other than PTA procedures, these trends did not reach statistical significance.
Discussion
A significant impact of the COVID-19 pandemic on surgical services is the suspension of non-urgent elective operating. In response to this, VSGBI published further guidance with instructions to defer all elective arterial and venous surgery, treat asymptomatic carotid artery disease with best medical therapy where clinically appropriate, and change the threshold of aneurysm repair for >7 cm or imminent rupture.6,8,9 This initial reduction was shown by the NVR report, which found that only 8–12% of elective abdominal aortic aneurysm (AAA) repairs were performed in April 2020 compared with April 2019 and 20% of lower limb bypass and 28% of CEA procedures were performed.10 In addition, units were advised to place consideration on endovascular options where possible to reduce morbidity, minimise occupancy of intensive care beds and length of inpatient stay.6,8,9 This was echoed by a slight national increase in the use of EVAR over OAR for elective and ruptured aneurysms of up to 18.2%.10,11 However, vascular surgery involves many procedures performed on an urgent or emergency basis, and the progressive nature of common vascular conditions such as AAA and chronic limb-threatening ischaemia means any delays to treatment will have both limb- and life-threatening consequences and will result in a significant burden to the services once capacity returns.
As the first lockdown lifted, VSGBI published further guidance on the resumption of these less urgent and elective cases.8 Although vascular units across the UK are still not back at normal operating capacity, changes such as preoperative self-isolation, uptake of vaccination and increased preoperative COVID-19 testing has allowed the resumption of most urgent and semi-urgent cases.8,12
Moreover, the pandemic has caused numerous short-term effects for surgical trainees such as redeployment, cancelled courses, reduced experience in operating, outpatient clinic and MDM, which will have implications for the future surgical workforce.2,4 The Vascular and Endovascular Research Network (VERN) showed that 29.0% of clinics were cancelled and up to 79.1% adopted the use of the ‘hot’ clinic to assess acute/urgent clinic patients.11 Our study has shown that trainees are still attending outpatient clinics, but does not comment on the type of clinic attended. Likewise, the Scottish trainees still had regular access to MDM, although globally they have reduced by 59.5%.11 In a comparative study of logbook numbers of surgical trainees in the UK, Clements et al showed that vascular surgery has been one of the least affected major surgical specialties for overall operative experience.7 As may be predicted, the number of urgent and emergency cases in vascular surgery recorded on elogbook have remained similar to pre-pandemic levels.7 Our results corroborate this and show that vascular trainees continued to gain good exposure to index procedures, which may be due to the emergency nature of vascular surgery.
In addition, Munro et al found that there has been a reduction of 50% in trainees as primary operators across all surgical specialties, which may substantially reduce their opportunities to achieve procedure competencies.4 The data described in our study show that Scottish vascular trainees are maintaining their exposure to procedures as primary operator. The exception to this is a statistically significant reduction in PTA as primary operator, despite total numbers remaining the same. This may be due to competition for training with interventional radiology (IR) trainees, reduction in IR room capacity and associated with guidance for increased consultant operating.1 Munro et al also suggest that senior trainees have been more affected than their junior counterparts, which becomes an obstacle to completing training.4 Although overall fewer cases were performed by the senior trainees in this study, they were not of statistical significance and this has not affected their ARCP/CCT (certificate of completion of training) outcome.
Despite retention of operating levels, Scottish vascular trainees have been subject to other disruptions to training due to the COVID-19 pandemic.4 Around two-thirds of trainees were subject to rota changes and redeployment whilst others had courses and professional examinations affected. Despite this, and the reduction in elective operating, vascular trainees in Scotland achieved satisfactory ARCP outcomes. Although the COVID-19 pandemic has resulted in fewer formal training opportunities, there have been notable positive effects. Several teaching webinars have been held, accessible to all trainees, as they are able to attend in their own time or watch retrospectively if recorded. With lack of formal courses and conferences, the trainees’ study leave budget (with trainees’ permission) was used to develop regional training opportunities such as cadaveric courses and a non-technical skills course.2 In addition, the pandemic has provided unique opportunities in audit and research. Further, the recognition of the impact on training has encouraged training bodies to adapt to and overcome the problems that have and may continue to arise in the future.4,5
Study limitations
The limitations of this study were that some trainees were out-of-programme or on a different specialty during part of the data capture periods, so true numbers may be slightly different. Both data capture periods were over annual changeover, where there is often service disruption due to changing shift patterns irrespective of the COVID-19 pandemic. Finally, the survey did not evaluate the mental health impact on trainees and therefore does not take into account whether they have taken time off due to self-isolation, shielding or burn-out, which many healthcare staff have been subject to during this time. We will need to continue to be vigilant of staff well-being as surgical services will be expected to catch up on the continually increasing workload in order to resume normal operating. We are yet to see the long-term effects on training and the surgical workforce.
Conclusions
Although the COVID-19 pandemic has had detrimental effects to healthcare worldwide and particularly to surgical training, vascular trainees in Scotland have not been as severely affected with training opportunities for index procedures remaining similar to pre-pandemic levels. The long-term impact of the pandemic on surgical training in the UK remains unknown; however, our data show some promise that training programmes can continue to deliver high-quality training in what has been an undoubtedly more hostile period for the provision of surgical services.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(2):42-47
Publication date:
February 23, 2022
Author Affiliations:
1.Clinical Fellow, Department of Vascular Surgery, Ninewells Hospital, Dundee, UK
2.Specialist Trainee Registrar, Vascular Surgery, Scottish Deanery, UK
3.Consultant Vascular Surgeon, Ninewells Hospital, Dundee, UK











