EDITORIALS
The 2021 Vascular Surgery Curriculum journey
Jones KG1
In August 2021 the new Vascular Surgery Curriculum became active as the approved framework for the training of doctors to the level of independent consultant practice in Vascular Surgery, inclusive of a change to phases of training (1–3) and the introduction of a new assessment system with the Multiple Consultant Report (MCR). The MCR has the component parts of nine Generic Professional Capabilities (GPCs) and five Capabilities in Practice (CiPs).
This 2021 curriculum change was not an isolated update just for Vascular Surgery; indeed, changes to all the surgical curricula were mandated by the General Medical Council (GMC) as a response to the criticisms of the existing competence-based assessment regime being used in a manner that emphasised the gaining of competencies too heavily in comparison with the use of professional judgement.1,2
This GMC-mandated change to all the surgical curricula was also driven by medical education research, which showed that global judgements by supervisors were better able to take account of the context of a trainee’s performance and were, therefore, more valid to assessment than deconstructed checklists.3
This research, in particular that of Olle Ten Cate, led to the concept of Entrustable Professional Activities, which proposed that performance was more than competence and included factors which could not be captured on a work-based assessment.4,5 This format focused on the performance of higher-level activities such as the management of an outpatient clinic, and from this evolved the curriculum design that the GMC described as outcomes-based.
The Shape of Training review and Excellence by Design: Standards for Postgraduate Curricula provided opportunities to reform postgraduate training so the curriculum will produce a workforce fit for the needs of patients, producing doctors who are more patient-focused, more generalist and who have more flexibility in their career structure.1,6 The GMC’s introduction of updated standards for curricula and assessment processes laid out in Excellence by Design required all medical curricula to be based on high-level outcomes. The high-level outcomes of the Vascular Surgery Curriculum are called Capabilities in Practice (CiPs) and integrate parts of the syllabus to describe the professional tasks within the scope of specialty practice. The supervision level these CiPs are assessed against is that of a day 1 consultant in Vascular Surgery. At the centre of each of these groups of tasks are Generic Professional Capabilities (GPCs), interdependent essential capabilities that underpin professional medical practice and are common to all who practise medicine.2 The GPCs are in keeping with Good Medical Practice,5 and equipping all trainees with these transferable capabilities should result in a more flexible, adaptable workforce.
So, for Vascular Surgery this meant that, through the Specialty Advisory Committee (SAC), we needed to produce a curriculum that would be deliverable, using this outcomes-based model and would better support the needs of patients and service providers by ensuring the medical workforce would be able to meet patient and population trends. Hence the Vascular Surgery Curriculum purpose statement states “The purpose of the curriculum for Vascular Surgery is to produce, at certification, competent doctors, able to deliver excellent outcomes for patients as consultant Vascular surgeons in the UK. Evidence from the last decade indicates significant improvement in outcomes with surgeons being trained in a special interest (Vascular Surgery rather than General Surgery with a special interest in Vascular Surgery), but also of the need to increase the consultant capacity to provide specialist Vascular Surgery in the United Kingdom and the Republic of Ireland”. This also highlights the vascular-focused training benefit within the new specialty.
Therefore, under the direction of the Joint Committee of Surgical Training, the SAC formed a Curriculum Writing Group which produced a purpose statement that was approved by the GMC’s Curriculum Oversight Group. This purpose statement had been requested to highlight that Interventional Radiology was clearly described within the scope of practice and that the future development of a Specific Capability in Practice common to all Specialty Curricula training in this skill be considered.
The next stage of the process was the writing of the new curriculum, with full stakeholder agreement, in order to submit to the GMC’s Curriculum Advisory Group. This process included meetings and correspondence with the comparable Interventional Radiology Curriculum Writing Group to discuss the development of the common ground, from which was developed the descriptions of collaborative working within the syllabus and the description of hybrid procedures involving common femoral artery surgery with inflow or outflow endovascular procedures as Combined Open With Endovascular Reconstruction (COWER). At a full stakeholder meeting, patient groups, human resources, all allied specialties and trainee representatives were all able to input and support planned revisions to the curriculum including specified index case requirements.7
The plan at this stage was to make minimal changes to the curriculum syllabus content, but to simply incorporate the higher- level outcomes. However, on final review our Interventional Radiology colleagues requested a further change as it was felt that the technical skill levels – especially those related to endovascular skills – were difficult to deliver without negatively affecting the development of Interventional Radiology trainees. A further small working group looked for a solution and determined that actually removing these technical skill levels would be beneficial. The syllabus was therefore completely rewritten as a series of objectives that could be assessed with the MCR as to whether the trainee would be appropriate for phase of training and finally at the level of a day 1 consultant. This approach recognises the variation that may occur due to different work patterns within units, and we ensured it was documented that trainees may undertake periods of training in other regions in order to gain appropriate experience. By making these changes we actually aligned the curriculum even more closely to the GMC’s higher-level outcomes with the development of the objectives assessed by the required supervision levels and the observed trainee performance by their Consultant Supervisors.
These changes enabled agreement from all stakeholder groups and subsequently from NHS employers. The GMC, in the Summer of 2020, approved the Vascular Surgery Curriculum, though due to COVID the implementation was delayed until August 2021 (although the Irish trainees started to use it in July 2021). The approval letter made it clear that Vascular Surgery trainees would learn endovascular techniques without limiting the training opportunities of Interventional Radiology trainees. As a further stipulation, the training of endovascular techniques would be monitored and any concerns about the accessibility to training of either group of trainees would be reported to the GMC. Both specialty groups would also be expected to report back about the deliverability at one year, in addition to the Joint Committee on Surgical Training implementation report regarding all curricula. The small joint specialty writing group considered the reciprocal training and training through collaborative procedures model. A typical example may be an Interventional Radiology trainee being taken through the iliac endovascular component of a COWER by a Vascular Surgery consultant in the hybrid operating theatre whilst the Vascular Surgery trainee is in the Interventional Radiology suite being supervised through a percutaneous lower limb angioplasty by an Interventional Radiology consultant.
For the trainee starting Vascular Surgery in 2021, the syllabus has six groups of topics including a group that covers the abdominal and general surgery objectives. The expectation is that the trainee will undertake one year of General Surgery placements within the first two years of the second phase of training and would not be expected to be on call for General Surgery beyond this time. Within the groups each topic has several components, each with an objective that will be assessed against the appropriate phase level or CiP supervision level within the MCR process. This makes it easy for a trainee to map their skill and knowledge progression against the objectives and be guided by the detailed feedback provided by the MCR and the Assigned Educational Supervisor directed learning agreements within the Intercollegiate Surgical Curriculum Programme (ISCP).
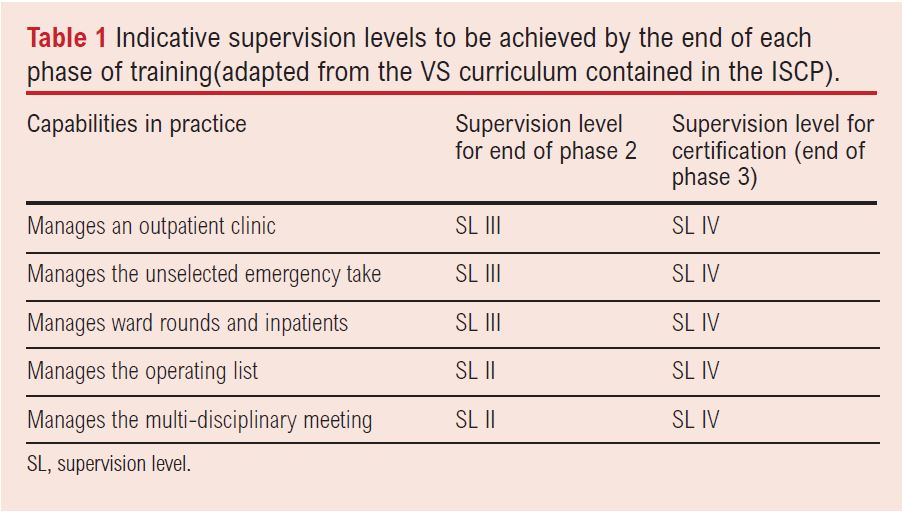
ISCP clearly sets out the expected CiP requirements at the critical progression points and for certification (Table 1). The most notable change is that the time requirement for training is removed and replaced by having achieved level IV or V in all the CiPs along with all the competencies in the nine domains of the GPC framework. This allows trainees to achieve a Certificate of Completion of Training more quickly than the indicative six years expected for the average trainee. These changes should specifically help the less than full time trainees with progression based on performance level and MCR feedback rather than purely a time requirement.
There was some concern over the removal of mandated components of the curriculum, such as no longer having to first author a peer-reviewed publication. However, four broad research areas are required for certification and require evidence of performance for clinical and educational supervisors and the Annual Review of Competence Progression (ARCP) panel to assess. The most straightforward method to generate this evidence may well remain a period of dedicated research towards a higher degree and associated publications. The certification requirements are clearly set out in the curriculum. Operative performance will be assessed as a component part of the ‘Manages the Operating List’ CiP and mapped against the phase relative objectives highlighted within the syllabus. Within this CiP and specific to Vascular Surgery is the requirement for trainees to determine the most appropriate environment in which to undertake an intervention (eg, operating theatre/hybrid or endovascular suite) and to be able to apply all the descriptors to optimally manage patients in all those environments.
As further guidance to trainees, the curriculum highlights key syllabus topics for learning which include Vascular Critical Conditions that specifically require evidence of being at the level of a day 1 consultant (ie, level 4 Case-based Discussion (CbD) or Clinical evaluation Exercise (CeX)). These are also assessed within the intercollegiate examination and supported by a satisfactory logbook. These Vascular Critical Conditions are Acute Limb Ischaemia, Abdominal Aortic Aneurysms and Fulminant Diabetic Foot Sepsis, which were chosen after extensive stakeholder feedback, and contain 11 groupings of cases with an indicative requirement to have 10 procedure based assessments (PBAs) that show progression to competence and to include four at level 4 by at least two trainers. Included within these groupings would be PBAs that also show collaborative working.
Finally, all mandatory courses have been removed from the curriculum with the exception of the Advance Trauma Life Support course, and even this allows equivalence to be undertaken. Previously undertaken courses such as Training the Trainers remain valuable examples of evidence for the relevant certification requirements. Again, these changes are common to all surgical curricula as directed by the GMC.
I hope I have described clearly the evolution of the 2021 Vascular Surgery Curriculum which contains syllabus objectives to improve and facilitate assessment of trainee performance and progression. The delivery of this curriculum will be enhanced by both trainer and trainee interaction with the MCR process. Within this process, I feel enhanced focused feedback from the supervisor to the trainee is the most important issue.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(2):18-20
Publication date:
February 21, 2022
Author Affiliations:
1.Consultant Vascular Surgeon, Chair of VS Education and Training Committee and Vascular SAC 2021 Curriculum Lead











