PROTOCOL
The DEFINITE Audit: a prospective audit of diabetic foot debridement in theatre – a protocol
The Vascular and Endovascular Research Network (VERN) Executive Committee: Hitchman L,1 Birmpili P,2 Gwilym B,3 Singh A,4 Onida S,5 Blair R,6 Dovell G,7 Dattani N,8 Saratzis A,8 Bosanquet D,3 Shalhoub J,5 Ambler G,9 Nandhra S,11 Benson R,10
Plain English Summary
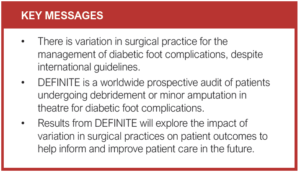
Why we are undertaking this work: Diabetes foot ulcers often become infected and require operations to treat the infection. The operation can either be to remove unhealthy tissue (debridement) or to remove infected toes (minor amputations). There are guidelines on the best way to perform these operations; however, there is variation in how these operations are performed.
What we will do: This is a worldwide study of patients with a diabetic foot complication who have a debridement or minor amputation. We will collect data on how surgeons treat patients before the operation, how surgeons perform the operation and the treatment patients receive after the operation. We will compare this to the guidelines. We will also collect data on how long wounds take to heal, the number of people who lose their leg (major amputation) and the number of people who died. This is to see if certain treatments result in better outcomes.
What this means: This study will help to identify areas for improvement in the care of diabetic foot complications and help to suggest which treatments result in better healing.
Abstract
Background: People with diabetes are commonly affected by foot ulceration (DFU) and subsequent or concurrent infection (DFI). Surgical debridement is often needed to contain infection. Despite international guidelines, there remains significant variation in surgical practice of diabetic foot wound debridement in the operating theatre.
Methods: Diabetic Foot Ulcer Debridement in Theatre Audit (DEFINITE) is a global multicentre, prospective audit of consecutive patients undergoing a debridement or minor amputation in theatre for a diabetic foot complication. DEFINITE is led by the Vascular and Endovascular Research Network (VERN). The primary outcome is adherence to recommended practice as outlined in the International Working Group on the Diabetic Foot and Global Vascular Guidelines. Secondary outcomes are incidence of healing, re-admission, further amputation (minor and major) and mortality at 90 days. Anonymised data will be collected via REDCap. Eligibility and study registration at all hospital institutions performing in-theatre management of diabetic foot complications are eligible to participate after obtaining appropriate institutional level audit approvals. A lead clinician will be responsible for approvals and data management.
Pathway to impact: This audit addresses shared patient-clinician priorities and is supported by the UK Vascular Society multidisciplinary Special Interest Group on the Diabetic Foot. The results will be presented at international scientific meetings and submitted for publication in peer-reviewed publications. The results will also be used to initiate improvement in patient care.
Introduction
People with diabetes are at high risk of developing foot ulceration (DFU). Once established, diabetic foot ulcers are at risk of rapid deterioration and infection which can lead to bacteraemia and sepsis. Infected DFU is associated with high morbidity, limb loss and death.1–3 The development of severe infection requires emergency hospital admission and surgery to remove necrotic and infected tissue, which is in turn associated with high levels of morbidity and mortality.4,5 Often multiple episodes of wound debridement, with or without minor amputation, and intravenous antibiotics are required to eradicate the infection. The economic impact is substantial with 0.9% of the UK National Health Service annual budget dedicated to the management of DFU.6
Patients and multidisciplinary clinicians recognise the scale and significance of this problem. Recently borne out in the Priority Setting Partnership led by the Vascular Society of Great Britain and Ireland (VSGBI) in collaboration with the James Lind Alliance (JLA),7 ‘improving outcomes in diabetic foot infections’ is a top shared research priority.8
There are guidelines available to support practice, primarily aimed at improving healing rates following debridement and reducing the incidence of major lower limb amputation.9-11 The International Working Group for Diabetic Foot (IWGDF) guidelines10 and The Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia11 outline critical recommendations on dealing with infected DFUs. In brief, these guidelines advise removal of all infected and necrotic tissue, drainage of sepsis, effective irrigation, sample collection for microbiological analysis, adequate dressing and sensitivity-driven antimicrobial use.
The Diabetic Foot Ulcer Debridement in Theatre Audit (DEFINITE) aims to assess the current pathways of care for patients with diabetes who undergo a digital amputation and/or foot wound debridement and compare surgical practice with the IWGDF and Global Vascular Guidelines. Secondary aims are to investigate if variations in practice are linked to wound healing rates, reoperation rates (further debridement or minor amputation), 3-month major lower limb amputation rates and 3-month readmission rates. It is hoped that the data gathered will support advances in diabetic foot care addressing a shared patient-clinician research priority.
Methods
Design
This is a multicentre, prospective service evaluation audit conducted in hospitals around the globe. It is delivered through the Vascular and Endovascular Research Network (VERN), a trainee-led national research collaborative that engages with research-active vascular trainees and allied healthcare professionals.
Eligibility criteria
All patients undergoing debridement of a foot wound or minor amputation in the operating theatre with a confirmed diagnosis of diabetes will be included in the audit. A separate record will be created if the patient undergoes debridement or minor amputation in the contralateral limb during the study period.
Patients will be excluded if they have foot wound debridement or minor amputation in a setting other than the operating theatre or if they are younger than 18 years. Patients who have undergone ipsilateral foot debridement or minor amputation in the preceding 6 weeks, and this index event is outside the study period, will also be excluded.
Outcomes measures
The primary outcome is adherence of current practice in debridement and minor amputation of diabetic foot disease to the recommendations outlined in the IWGDF9 and Global Vascular Guidelines10 (see Supplementary Information in Appendix 1 online at www.jvsgbi.com). Adherence is defined as the extent to which the procedure undertaken corresponds to the guidance. The audit will report adherence to each item in the guidance as well as overall adherence. Secondary outcomes are the incidence of healing at 3 months, the 3-month reoperation rate, readmission rate, minor and major lower limb amputation rates, the type of microorganisms isolated from diabetic foot tissue samples taken intraoperatively, and the duration and type of antibiotics administered after such procedures.
Recruitment
The DEFINITE audit is open to all centres which provide elective and/or emergency surgical management for diabetic foot infection. One team member acting as site lead clinician will be the point of contact between the DEFINITE audit team and the local audit team. They will register their hospital/site and team members for the audit by completing an online form found on the VERN website, that includes collection of information on existing diabetic foot services in the participating centres. The lead clinician will have overall responsibility for ensuring the audit is conducted according to the standards and methods described in this protocol at their hospital/site, and any instances of non-compliance will be reported by them to the DEFINITE audit team. The anticipated number of audit team members per centre is one lead clinician and five other team members, such as medical trainees, allied healthcare professionals and medical students. If centres include more than five additional team members, it is expected that allied healthcare professionals and/or medical students are included.
Prospective registration of the DEFINITE audit is required prior to data collection. It is the responsibility of the local audit lead to ensure this is complete.
Participant cases will be identified by a member of the DEFINITE team at each centre as per the inclusion/exclusion criteria, using acute admission lists, diabetic foot ward rounds and operating lists (as per local practice). Patient/disease registries will not be screened to identify potential participants. Queries regarding participant eligibility will be directed to the lead clinician, and non-resolution referred to the VERN team.
Data collection
The complete data collection form is available as Supplementary Information in Appendix 2 online at www.jvsgbi.com and at www.vascular-research.net/definite/.
Anonymised data collected will include baseline demographics (age, gender, smoking status), comorbidities, medications, American Society of Anaesthesiologists (ASA) physical status and previous re-vascularisation procedures.
Preoperative data will include COVID-19 status, use of variable rate insulin infusion, medications (regular insulin, steroids and anticoagulants), white cell count, and C-reactive protein, haemoglobin, creatinine and albumin levels. The audit will also collect the indication for the operative procedure, infection status of the contralateral limb, wound ischaemia foot infection (WIfI) stage,1 whether osteomyelitis was suspected and preoperative antibiotic use. Preoperative antibiotic use will include length of antibiotic course prior to procedure, route of administration, type of antibiotic used and whether any preoperative topical antibiotics were used.
Intraoperatively, the audit will collect data on the speciality which the procedure was performed under, the type of procedure (debridement, digit amputation, both), urgency of the procedure, operative time, skin preparation solution used, irrigation fluid used, packing material choice, local antibiotic use, use of a drain and dressing choice. The audit will also collect data on whether soft tissue and bone samples were sent for microbiology and histology and the method of tissue sample collection.
Postoperative data includes organisms grown from the microbiology samples, antibiotic use (route, length, type, sensitivity to organisms cultured), total length of hospital stay, postoperative morbidity grade (Clavien–Dindo), postoperative mobilisation status, length of drain use (if used), vascular imaging and revascularisation procedures. The audit will also collect data on return to theatre for further debridement or amputation and in-hospital mortality.
The 3-month data collection items are duration of antibiotic therapy, COVID infection status, complete wound healing at 90 days, readmission, further debridement, further amputation (minor/major) and mortality.
Data will be prospectively collected from paper or electronic hospital records. Preoperative data will be collected prior to the procedure, intraoperative data will be collected immediately after the procedure has taken place, postoperative data will be collected when the patient is discharged from hospital and 3-month data will be collected 3 months after the patient underwent the procedure. Data will be entered onto a purpose-built electronic database on the Research Electronic Data Capture (REDCap) platform, hosted by Newcastle Joint Research Office. Data will be collected and uploaded by a member of the audit team with appropriate REDCap training from VERN.
Data management
All audit data will be preferably uploaded directly to REDCap with printable case report forms (CRFs) available if required to facilitate data capture. Oversight of paper CRFs used at centres will be the responsibility of each centre’s lead clinician. All CRFs used will be securely stored in an appropriate location onsite until data are uploaded to REDCap, at which point the centre’s lead clinician will be responsible for ensuring they are appropriately destroyed.
Through the audit’s REDCap database design, no identifiable data can be uploaded. A specific audit identification number will be assigned to each patient to allow anonymised data to be collected. Patients may be enrolled twice if undergoing a procedure for both feet during the study period, and in these cases a unique study ID will be assigned to each procedure. Each centre’s lead clinician will be responsible for ensuring a database containing each participant’s local hospital ID and corresponding audit ID is maintained to ensure accurate follow-up data and stored securely on an appropriate hospital computer. Data will be kept for two years to allow a possible follow-up audit and will be destroyed thereafter. Data will be available to others. The minimum dataset will be included in the DEFINITE results paper as a supporting information file with fully anonymised patient data.
Data analysis
Descriptive analyses will be performed to describe variations in practice and examine secondary outcomes. Secondary outcomes will be compared between adherent and non-adherent groups. Continuous data will be tested for normality and parametric or non-parametric tests will be used as appropriate. The χ2 test will be used to analyse for differences in categorical variables.
Missing data will be analysed to determine the pattern of missingness and, if appropriate, multiple imputation will be used using the Markov chain Monte Carlo method. Sensitivity analyses will be conducted to compare the results of imputed data analysis with complete-case analysis.
Univariable and multivariable regression analyses will be used to identify independent predictors of further debridement/minor amputation, major lower limb amputation, and complete wound healing at 3 months following the index procedure. A p value of <0.05 will be used to define statistical significance.
Data quality
Following the initial data collection period, data completeness will be quantified. Patient records with less than 95% completeness of mandatory data points will be returned to the centre for completion and, if not possible, the record will be excluded from analysis. All centres will be required to validate data accuracy. Each centre will identify an additional team member (not involved in initial data collection) to recapture 25% of the data points (at random) for 20% of the cases (at random) for their centre. Any centre reporting less than 95% accuracy will be required to validate a further 20% of their cases, and the lead clinician to investigate and report back to the DEFINITE management team. All centres will be required to assess case ascertainment. The lead at each centre (or delegate of) will be required to review theatre records or registry data (eg, National Vascular Registry) and report the total number of eligible procedures performed during the study period to the DEFINITE management team for comparison with cases submitted to REDCap.
Regulatory approval and research governance
The audit will be conducted in compliance with the principles of Good Clinical Practice (GCP) guidelines and in accordance with all applicable regulatory guidance, including, but not limited to, the UK Policy Framework for Health and Social Care Research. Ethical approval is not required in the UK as this study is a service evaluation, which does not include any change in routine patient care, and no patient identifiable data will be collected. The lead clinician will be responsible for local audit governance approvals as per their hospital/site policy. Non-UK centres will be required to show evidence of appropriate approvals in accordance with local regulations; this may require institutional review board approval.
The audit departments at the following NHS trusts have approved the project locally: Hull University Teaching Hospital NHS Trust, Leeds Teaching Hospitals NHS Trust, Barts Health NHS Trust, St George’s NHS Foundation Trust, Worcester Acute Hospitals NHS Trust, NHS Tayside, Oxford University Hospitals NHS Trust, Manchester University Foundation Trust, London North West University Healthcare NHS Trust, South Tyneside and Sunderland NHS Foundation Trust, NHS Lothian, NHS Greater Glasgow and Clyde, South Tees Hospitals NHS Foundation Trust, Mid and South Essex NHS Foundation Trust, Manchester University NHS Foundation Trust, Nottingham University Hospitals NHS Trust, North Bristol NHS Trust, Shrewsbury and Telford Hospital NHS Trust, Frimley Health NHS Foundation Trust, Imperial College Healthcare NHS Trust, University Hospitals Sussex NHS Foundation Trust, NHS Grampian, Aneurin Bevan University Health Board, Royal Devon and Exeter Hospital, Countess of Chester Hospital NHS Foundation Trust, University Hospitals of Leicester NHS Trust, Cambridge University Hospital NHS Trust, University Hospitals of North Midlands NHS Trust, Belfast Health and Social Care Trust, Nottingham University Hospitals NHS Trust, University Hospitals of Southampton NHS Foundation Trust and Gloucestershire Hospitals NHS Foundation Trust. At international centres the audit has been approved by local boards at: Canberra Health Service, King Saud Medical City, Hippocratio Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece, University Hospital of Trieste, Dar Al-Elaj Specialized Hospital, Waikato Hospital, Christchurch Hospital, Canterbury District Health Board, University Hospital of Patras, University of Patras and Royal Adelaide Hospital.
Data protection and patient confidentiality
The auit will comply with the Data Protection Act 2018. Participants will be assigned a unique REDCap identifier upon enrolment into the audit to allow pseudonymisation of patient data. Access to patient identifiable information will be restricted to members of the patient’s usual clinical team. Hard copies of audit documents will be securely stored in an appropriate location at each centre and will be the responsibility of the lead clinician.
Authorship
A collaborative authorship model will be used for all dissemination methods. To qualify for collaborative authorship, individuals should review and approve any manuscripts for submission to peer-reviewed journals and should either have a significant role in the set-up and management of the DEFINITE audit (including audit department registration/institutional review board approval, creation of a data collection team and engagement with VERN to ensure timely upload of data) or capture sufficient data to warrant authorship. This would be the equivalent of collecting baseline and follow-up data on approximately 10 patients, although it is appreciated that individuals may participate in either baseline data collection or follow-up data capture only.
Current status
The DEFINITE study recruitment of new centres was between 1 December 2021 and 31 March 2022. The expected date of the last patient to be included is 30 June 2022 and data collection will end on 30 September 2022.
Discussion
The DEFINITE audit will capture current worldwide practice on diabetic foot debridement and minor amputation in theatre to identify variations in management and clinical outcomes. This will include information on known patient factors that affect wound healing,2 preoperative investigations, step-by-step operative details, use of antimicrobials and clinical outcomes to 90 days post-debridement.
Existing global guidelines for the management of at-risk lower limbs in people with diabetes include the IWGDF Guidelines on the diagnosis and treatment of foot infection in persons with diabetes and the Global Vascular Guidelines on the Management of Chronic Limb Threatening Ischaemia.10,11 There are variable levels of evidence supporting recommendations in these documents. Areas of most uncertainty include microbial sampling,12,13 wound irrigation,14,15 choice of dressings,16-20 ambulation status21 and use of antimicrobials.22,23 This audit will demonstrate whether there is significant variation in practice in these key aspects of management.
The guidelines recommend tissue samples should be obtained for isolating micro-organisms. This is supported by the CODIFI study, which also reports that clinicians are more likely to act on results obtained by tissue sampling compared with swabs.12 However, Travis et al reported no difference between tissue samples and swabs on microbial culture results.13 The ongoing CODIFI2 randomised controlled trial aims to compare the impact of tissue and swab sample results on DFU healing time.15 This audit will capture the methods used at different centres, will compare microbial growth obtained from different sampling techniques, and determine whether there are geographical differences in microbiological growth.
It is currently unknown whether skin preparation and/or irrigation solution choice impacts upon clinical outcomes for DFU patients undergoing debridement/minor amputation. The current guidelines on managing DFU infections reflect this uncertainty. The National Institute for Health and Care Excellence (NICE) guideline on preventing surgical site infection (NG125) recommends alcohol-based solution of chlorhexidine as first choice skin aseptic solution.24 Saline, antibiotic solutions, hydrogen peroxide, chlorhexidine and povidone-iodine solution are commonly used for wound irrigation. There has been no superiority shown between preparations; however, some are associated with severe adverse events.15,25 The DEFINITE audit will identify the frequency with which these skin preparation and irrigation fluid solutions are used in contemporary practice. The planned regression analyses will determine whether there are associations between skin preparation and irrigation fluid, and key clinical outcomes in this cohort.
Postoperatively, there is limited consensus on appropriate dressings for wound healing by secondary intention. A Cochrane review from 2018 compared negative pressure wound therapy (NPWT) to other dressings for post amputation or debridement in the diabetic foot, finding limited evidence for one dressing type over another in improving time to healing.16 This finding is not reflected in the IWGDF guidelines, which recommends NPWT post debridement in addition to standard care. The ongoing UK-based SWHSI2 randomised controlled trial aims to address this uncertainty around NPWT in wound healing by secondary intention.26 This audit will capture use of NPWT immediately post debridement or minor amputation in the diabetic foot.
Guidance on antimicrobial use post debridement recommends that antibiotics should be adjusted to the sensitivity of cultured organisms and given via the oral route. There is ongoing debate regarding the length and route of antibiotic treatment post debridement for the treatment of osteomyelitis in the diabetic foot.22 A pilot randomised clinical trial comparing 3 weeks to 6 weeks of antibiotics showed no significant difference in remission and adverse events.23 Antimicrobial prescribing practice will be explored in this audit.
The postoperative mobility status of patients is largely unknown and there is variation in the surgical community on weight-bearing status postoperatively. Offloading and specialist footwear are known to decrease the incidence of recurrence.21 Ambulation instructions for the immediate postoperative period will be collected in this study, and analysis will determine whether this is associated with clinical outcomes.
The collaborative model of this study is designed to capture practice in a large number of patients in a wide range of healthcare settings over a relatively short period of time. VERN has experience of delivering impactful international studies.27,28 Outputs from the DEFINITE study will inform future quality improvement and research projects to improve the care of patients with diabetic foot complications. One limitation of this audit will be the inability to determine direct causality between practice and outcome. The study aims to collect data from multiple sites in several countries; however, the results may not necessarily be representative of practice in areas where participation in the audit is low. Despite this, results from this audit will identify areas of variation in practice, identify compliance/non-compliance with international guidelines, and generate hypotheses to guide further research on improving clinical outcomes for this population.
Pathway to impact
This audit addresses shared patient-clinician priorities and is supported by the UK Vascular Society multidisciplinary special interest group on the diabetic foot. The results presented at national and international scientific meetings and in peer-reviewed publications will be used to initiate improvement in patient level care. A writing team, including those involved with the design, implementation and dissemination of the DEFINITE audit, will be responsible for presentation(s) and submission of manuscript(s) to peer-reviewed journal(s)/publications.
To prompt the results to patients and lay stakeholders, the writing team will work with patients and the public involved in the JLA Priority Setting Partnership to produce a patient-facing lay summary of the results. This will be distributed with support from the audit’s charitable supporters. A summary will also be sent to the JLA, Circulation Foundation and Diabetes UK for promotion.
In addition, the results of DEFINITE will be promoted through VERN’s Twitter account, newsletter and in dedicated webinars.
Conclusion
The DEFINITE study will provide a comprehensive overview of in-theatre debridement practice of diabetic foot complications worldwide and the associated clinical outcomes. This will identify variation and help target areas of care that can be improved.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(2):103-108
Publication date:
January 17, 2023
Author Affiliations:
1. Hull York Medical School, Hull, UK
2. Health Education North West, UK
3. Gwent Vascular Institute, Aneurin Bevan University Health Board, UK
4. Mid and South Essex NHS Foundation Trust, UK
5. Imperial College Healthcare NHS Trust, UK
6. Royal Victoria Hospital, Belfast, Ireland
7. Bristol Vascular Institute, North Bristol NHS Trust, UK
8. Leicester Vascular Institute, UK
9. Centre for Surgical Research, University of Bristol, UK
10. University of Birmingham, UK
11. Northern Vascular Centre, Newcastle Hospitals NHS Trust
Corresponding author:
Louise Hitchman
NIHR Doctoral Research Fellow, Academic Vascular Surgery Unit, 2nd Floor, Allam Building, Hull Royal Infirmary, Anlaby Road, Hull, HU3 2JZ, UK
Email: [email protected]











