CASE REPORT
A rare case of true tibioperoneal trunk aneurysm resulting in foot drop
Basra MS, Aziz O, Taumoepeau L
Abstract
A 75-year-old man presented with a six-week history of his right foot “making a slapping sound” whilst he walked and consequently having to adopt a “high-stepping gait”. Examination revealed a pulsatile swelling in his right popliteal fossa and signs of a peroneal nerve palsy. Computed tomography angiography (CTA) revealed a 2.5 cm tibioperoneal trunk aneurysm. True aneurysms of the tibioperoneal trunk are rare, and compression of surrounding nerves is an indication for surgical correction. This case highlights the importance of thorough vascular clinical assessment and prompt surgical intervention.
Case presentation
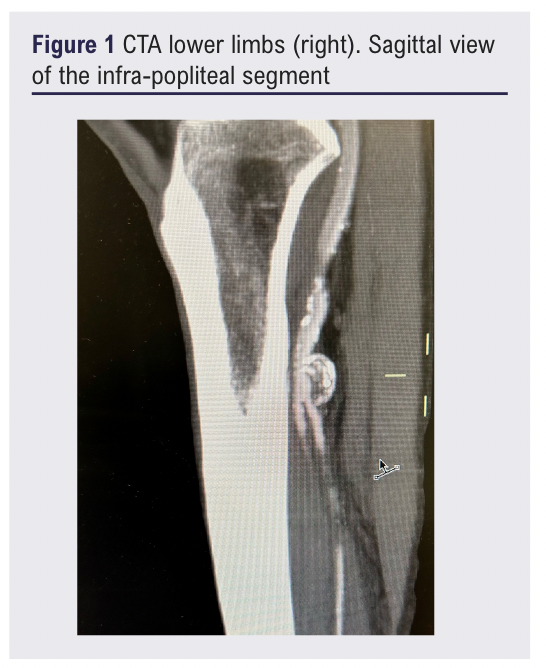
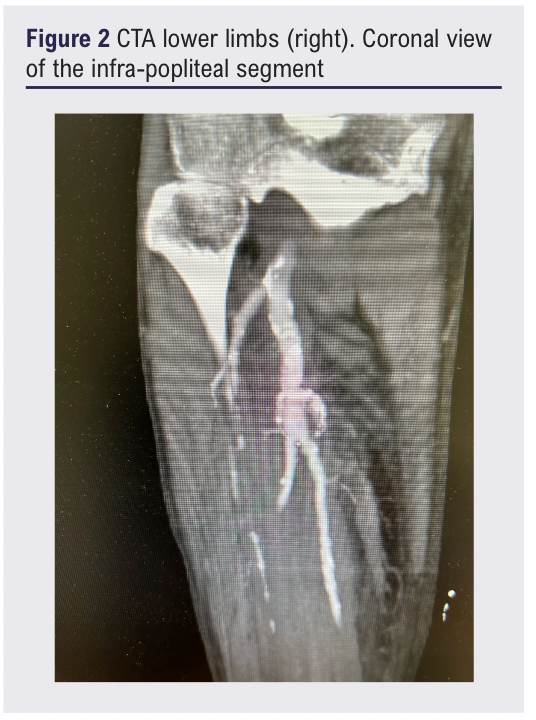
A 75-year-old man presented to the Orthopaedic outpatient clinic with a six-week history of an abnormal slapping sound from his right foot on walking. He had modified his walking to a high-stepped gait in order to avoid catching his foot and tripping. There was no history of trauma or previous lower limb surgery. The patient had no vascular risk factors and there were no features of critical limb ischaemia. Clinical examination confirmed a pulsatile swelling in the right popliteal fossa. The posterior tibial pulse was present, whereas the dorsalis pedis pulse was absent. Urgent computed tomographic angiography (CTA) of the lower limbs demonstrated a 2.5 cm tibioperoneal trunk aneurysm, with patent posterior tibial and peroneal arteries but an occluded anterior tibial artery in the proximal third (Figures 1 and 2).
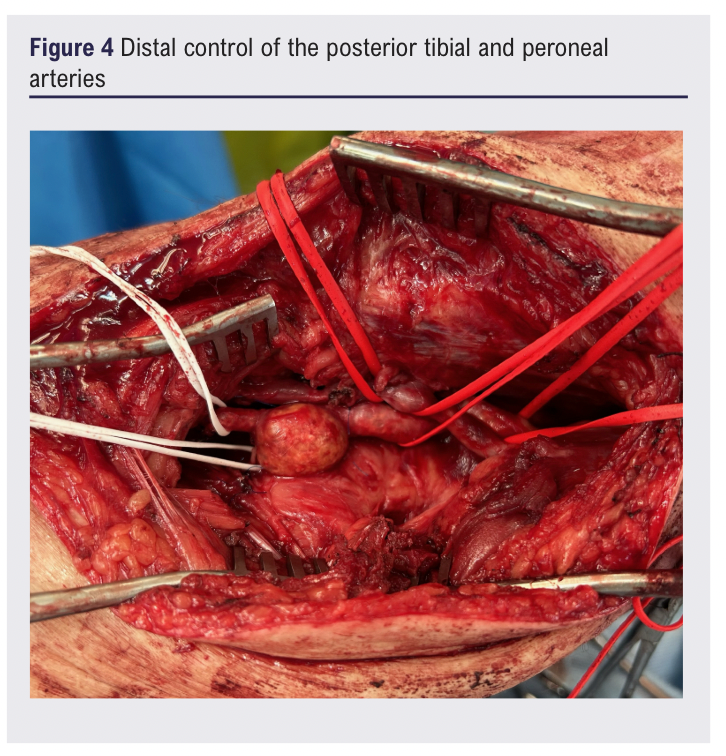
An open approach was selected to relieve the pressure of the aneurysm on the peroneal nerve, and to prevent embolisation of the distal run off. Under general anaesthesia, from a medial approach, control of the inflow from the below-knee popliteal artery was obtained using a silicone sling. Thereafter, the peroneal nerve was identified, preserved and carefully dissected off the aneurysm (Figure 3). The run-off vessels (peroneal and posterior tibial arteries) were also dissected and controlled with slings (Figure 4). The ipsilateral great saphenous vein had been dissected from the same incision prior to arterial dissection. After systemic heparinisation and clamping, the great saphenous vein was reversed and an interposition graft was fashioned, with the distal anastomosis incorporating the origins of both run-off arteries (Figure 5).

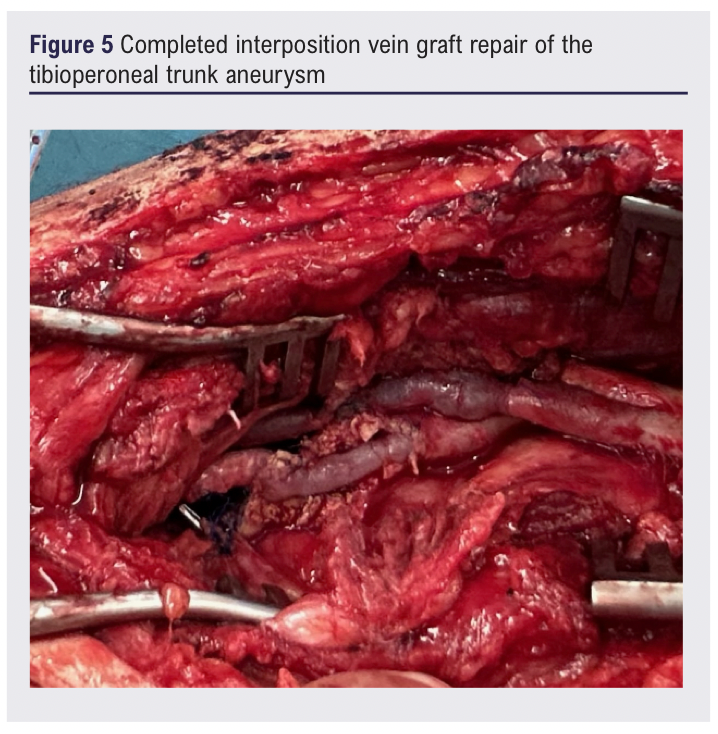
Post-operative ultrasound confirmed triphasic flow through the interposition graft into both run-off arteries and a strongly palpable posterior tibial pulse was detected. Five days post operation the patient was discharged on a statin and recommenced on his usual anticoagulation regime (rivaroxaban for atrial fibrillation).
At the six-week follow-up, the patient had resumed his usual activities, was weight-bearing and walking independently and his foot drop symptoms were improving with ongoing physiotherapy.
Discussion
True aneurysms of the tibioperoneal trunk are rare,1-5 and may present with atypical (non-vascular) signs and symptoms secondary to nerve compression.4 Thorough clinical assessment is mandated and high suspicion of a lower limb aneurysm should be managed with urgent arterial imaging (CTA or duplex), prompt vascular surgical review and consideration of surgical correction in order to prevent permanent nerve damage and disability.
Surgical management requires decompression of the aneurysm to relieve pressure on the nerve and distal revascularisation. In this patient, given that both patent run-off arteries were distal to the aneurysm, having gained proximal and distal control and opening the aneurysm sac a direct interposition graft repair was performed.
This case report of a true tibioperoneal trunk artery aneurysm resulting in peroneal nerve palsy and foot drop highlights the importance of vascular clinical assessment for atypical lower limb presentations in order to prevent missed or delayed diagnoses. We encourage surgeons to remain vigilant for rare lower limb aneurysms when presented with symptoms of foot drop and peroneal nerve palsy so that permanent nerve damage and morbidity may be prevented.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;4(2):115-117
Publication date:
February 28, 2025
Author Affiliations:
Department of Vascular Surgery,
Wellington Hospital,
New Zealand.
Corresponding author:
Melvinder Singh Basra
Department of Vascular Surgery, Wellington Hospital, 49-69 Riddiford Street, Wellington, 6021. New Zealand.
Email: [email protected]











