ORIGINAL RESEARCH
Research priorities for aortic diseases: results of the James Lind Alliance/Vascular Society GBI priority setting exercise
Lawson JA,1 Bown MJ,2 Bicknell CD,3 Long J,4 Gronlund TA,5 on behalf of the VSGBI Aortic Special Interest Group/ James Lind Alliance Priority Setting Partnership
Plain English Summary
Why we undertook the work: Researchers often focus on what they think is important, which can be different from what patients, carers and clinicians think. For this reason, it can also make it difficult for funding bodies to decide where best to target their limited funding. To address this issue, the Vascular Society of Great Britain and Ireland (VSGBI), with the James Lind Alliance (JLA), undertook a national Priority Setting Process (PSP) to identify the most important areas of vascular research in the UK. This paper presents the results of this process, focusing on aortic condition-related research topics.
What we did: The PSP was undertaken in three main phases. The first was an open-ended survey which aimed to collect the views of vascular healthcare professionals about their research priorities. The second phase was conducted in the same way but was aimed at gathering the opinions of vascular patients and carers about research topics that were most important to them. The third stage brought together the results of the two surveys and created a combined list of both vascular professional and patient research priorities. These priorities were discussed at a final workshop meeting attended by patients, carers and professionals who agreed an ordered ‘top 10’ list of research priorities for aortic conditions.
What we found: A total of 481 healthcare professionals and 373 patients or carers submitted research priorities about vascular conditions. These were amalgamated into a list of 18 priorities specifically about aortic conditions and were put into an order of importance at a workshop meeting. The final ‘top 10’ aortic research priorities related to improving how aortic conditions were identified and monitored, finding out how treatment options are decided, supporting recovery after an operation and more ways of predicting those at risk of having aortic conditions.
What this means: We have identified the most important research priorities for aortic conditions and encourage researchers and funders to focus their efforts in addressing these important topics.
Abstract
Background: In order to identify research priorities for aortic disease, a partnership between the Vascular Society of Great Britain and Ireland (VSGBI) and the James Lind Alliance (JLA) was established to capture the interests of a wide group of patients, carers and health professionals. One of the aims of the partnership was to establish the top 10 research priorities in the field of aortic disease.
Methods: A modified JLA Priority Setting Partnership was undertaken, during which healthcare professionals, patients and carers participated independently in two Vascular Society of Great Britain and Ireland (VSGBI)-led Delphi processes identifying research priorities in aortic disease. An aortic Special Interest Group composed of patients and healthcare professionals assessed the two lists of priorities, amalgamating similar priorities and generating a final list for ranking. An offer was sent to various patients, carers and healthcare professionals from different backgrounds with an interest in aortic disease to attend the final consensus workshop where a ranked top 10 list of aortic disease research priorities was produced using a nominal group technique.
Results: A total of 1,231 research priorities relating to general vascular surgery were submitted by 481 clinicians. From these, 162 aortic-specific research priorities were identified and combined into 15 final clinical priorities. In addition, 582 research priorities related to vascular surgery in general were submitted by 373 patients or carers. From these, 24 further aortic[1]specific research priorities were identified after combining similar priorities. Amalgamation of the clinician and patient priorities resulted in 18 priorities that were taken to the final consensus workshop, where a ranked top 10 list of aortic disease research priorities was produced. These priorities include themes of diagnosis, surveillance, management, recovery and predisposition. Conclusion: A collaborative effort between healthcare professionals and patients has identified a ranked top 10 list of aortic disease research priorities. This list will inform and guide clinicians, researchers and funders for the foreseeable future and will support future research that encompasses the important interests and representation of the wider network involved and affected by aortic disease.
Background
In the UK, aortic aneurysm affects approximately 4% or 80,000 men between the ages of 65 and 74 years.1 With a broad spectrum of rapidly evolving treatment options, advancing methods of management and investigation, many aspects of best clinical practice for aortic diseases are unknown.2 Aortic diseases are exemplified by aortic aneurysm, the most common aortopathy.3 Aortic disease research is integral to understanding the disease and guiding optimal management. In addition, it is imperative to consider the research goals and initiatives of all those involved in this vascular condition.4 To ensure treatment is aligned with the best interests of all involved, robust methodologies used to identify research priorities must be conducted. Disparities between what is traditionally deemed important by the clinicians and that which is perceived to be important by the patients, carers and families is a potential area of mismatch that can distort the areas of investigation. Another important consideration is that continued optimisation of patient care must occur within the constraints of research funding opportunities with finite resources and competitive processes. In combination, these factors demonstrate the need to have well thought out and important discussion involving all relevant individuals.
Optimal aortic disease management is multidisciplinary.2 Direct treatment of the aneurysm includes surgical and radiological intervention; however, pathways of care extend to a wider network including disease surveillance, rehabilitation and personal and professional support groups. To establish and develop key research priorities for aortic disease, the Vascular Society of Great Britain and Ireland (VSGBI) partnered with the James Lind Alliance (JLA) to conduct a validated research priority setting exercise reflective of both clinician and public interest.5 The aim was to generate a ranked list of aortic specific research priorities to appropriately direct future research and help set the agenda for impactful studies.
Methods
To identify public research priorities for vascular diseases the VSGBI in association with the JLA undertook a research priority setting exercise. Due to the large scale of this exercise, nine discrete working groups were formed, each focusing on a particular vascular or clinical area and each conducting a separate research priority setting exercise focusing on their particular area. This paper reports the outcomes from the aortic disease research priority setting exercise.
An initial Delphi survey was conducted to obtain clinician priorities, and this was followed by a JLA survey to gather the opinions of vascular patients and carers about their research priorities. The results of the clinician and patient surveys were amalgamated and final workshops held for each Special Interest Group (SIG), where patients and clinicians worked together to agree on a final list of joint research priorities.6-8
Scope of the aortic SIG
The remit of the aortic SIG is to support research into the care of patients living with or affected by aortic disease including preoperative, perioperative and postoperative care, and to develop the top 10 aortic research priorities. The top 10 priorities were established through a five-stage process (Figure 1).

Clinician-led Priority Setting Process
A clinician-led Priority Setting Process (PSP) was completed in 2018, which identified nine key vascular condition areas. These areas were obtained from 45 potential topics using a modified Delphi approach. The topics were collected through two rounds of online surveys involving the membership of the VSGBI, Society of Vascular Nurses (SVN), Society for Vascular Technology (SVT) and the Rouleaux Club (vascular surgical trainees). The first round invited any suggestions for research priorities in the broad scope of ‘vascular surgery’, which were then collated and categorised into pathological topics and research categories by a steering group. Priorities relating to the same fundamental issue were amalgamated. Summarised priorities were then recirculated in the second round for scoring according to importance. These results have been published,7 and the findings related to aortic disease are presented here.
Patient/carer-led research priority identification process
Patient and carer suggestions for research priorities were collected via an open-ended survey (27 August 2019 to 17 March 2020) which invited participants to submit their own opinions about vascular research priorities that they thought were important. The survey was available online and in paper format (with freepost return), and copies made available in outpatient clinics. SIGs took a lead in helping to distribute the surveys, with the aim to ensure a representative number of responses gathered for their specialty area. Charities and patient groups were contacted and asked to distribute the survey in newsletters and via websites. Submitted priorities were assigned to a SIG category for further review. SIGs were tasked with sorting the responses; those considered out of scope (eg, too broad, too specific or answered by existing evidence) were excluded and duplicates were combined and summarised into an overarching priority. A refined list was agreed for the next round of the survey (conducted between November 2020 and February 2021), which invited participants to select their vascular area(s) of interest and to score the priorities within this area using a Likert scale (ranging from ‘Extremely Important’ to ‘Not at all Important’ or ‘Don’t know’). All participants were invited to prioritise the Services Organisation priorities as these contained cross-cutting priorities that would apply to all vascular patients, regardless of their vascular condition.
Combining surveys process: sorting, interim prioritisation and amalgamation
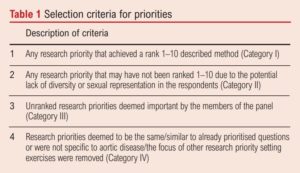
The clinician-led and patient and carer-led processes presented 39 aortic research priorities: 15 clinician-derived and 24 patient[1]derived. The aortic SIG reviewed for duplication or redundancy when amalgamating clinician and patient priorities. Clinician priorities were reviewed with patient input to reword any technical language to ensure patient participants at workshops would understand. To ensure meaningful discussion in the focus group meetings, a final revision process was conducted by the SIG to refine the list of priorities that would be taken forward to the final workshop. This research priority refinement was conducted in alignment with JLA methodology. The JLA advises a maximum of 18 priorities for discussion at a final workshop to promote manageable and invested discussion. Further reduction was therefore performed by categorisation. Categorisation included judging the importance of each of the priorities according to ranking using survey scores. Consideration of bias and inequality assessment (eg, women may have been underrepresented in the Delphi survey as aneurysm disease is 10 times less common in women, so questions regarding sex-specific treatments were considered) was then conducted to take into account the potential influence of participants’ demographics and influence on priority selection detailed in Table 1.
Final priority setting workshop
The aim of the workshop was to establish research priorities for aortic disease through facilitated, balanced and open conversation between patients, carers and healthcare workers. Participation of patients and carers in the final workshop was welcomed throughout the priority setting stages to ensure multiple opportunities for individuals to demonstrate interest and to share their views. Interested participants who have lived experience of aortic disease were then invited to attend the workshop to determine the top 10 research priorities. In addition, invitation through direct contact was made with patients/carers who are established members of patient representative bodies. Healthcare participants were contacted through direct communication with various national bodies, as well as through direct contacts of the SIG members. The workshop was held virtually to accommodate COVID-19 restrictions. To address potential accessibility and technical considerations as well as possible, induction sessions were carried out with participants as appropriate. Although presenting some limitations with the online virtual format potentially being a deterrent for participation, hosting a virtual workshop did enable the opportunity for some stakeholders to attend who ordinarily would not have been able to travel due to needs, caring or employment commitments. The experienced JLA facilitator opened the workshop and introduced the goals for the session. Participants were split into small breakout groups of approximately six, with a balanced representation of patients, carers and healthcare workers. Each small group was facilitated by a JLA representative, and members of the aortic SIG observed. All participants were informed of support services available to them during and after the workshop. Participants were reminded that the focus of the workshop was to help shape the research agenda with priorities that mattered to people with lived experience and the healthcare professionals who work with them. Participants were asked to consider the priorities on their own merit and not to be concerned about the feasibility of research. Participants had been sent the 18 priorities in advance of the workshop and asked to rank these for themselves before the event. The workshop approach was based on a ‘nominal group technique’ which allows participants to share their own initial thoughts and priorities. Through a structured and facilitated set of steps of clarification and consolidation, the group comes to a consensus ranking.
Overview of small group discussions
First round of discussion: Each participant was asked, in turn, to share their top three and lowest three priorities with the others in the group. The group was then facilitated to have an open discussion about the differences and similarities of their choices and to discuss any priorities previously not mentioned.
Second round of discussion: The same groups then entered a second round of discussion. Participants were provided with a shared screen showing an approximate positioning of the priorities on a preprepared ranking template, which had been prepared by the facilitator during the break. Participants were then given the opportunity to reconsider their initial set of priorities through discussion. The facilitator moved the priorities on the screen to reflect the agreed order from the group ranked 1–18.
Third round of discussion: The ranked priorities of the three separate small groups were combined by the lead facilitator using a geometric mean of the respective ranked positions. Taking into consideration the potential for anomalous positioning if groups have large discrepancies between ranking of a particular priority, a further round of discussion was held. New small groups were established, again with a balanced representation of patients, carers and healthcare workers, with at least one representative in each group from the initial group. This approach promoted diversity of participants, whilst permitting discussion as represented by previous considerations. Members of the second groups were then asked to review this combined ranking and to clarify their views and the views of others, with the focus on which priorities they wanted to see in the top 10.
Fourth round of discussion: All participants came together as one group to discuss the combined results of the rankings of the three groups
Results
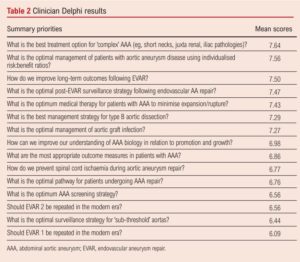
Clinician research priority identification and prioritisation A total of 481 clinicians submitted 1,231 research priorities relating to vascular surgery in general. 162 aortic-related research priorities were submitted, 16 of which were excluded outright as they were too specific to single patient experience. The remaining 146 priorities were combined and summarised into 15 clinician priorities for scoring, the results of which are shown in Table 2.
Patient/carer research priority identification and prioritisation
A total of 373 patients/carers suggested 582 research priorities related to vascular surgery in general, of which 140 were specific to aortic disease. After data cleaning (eg, removing nonsensical suggestions) and combining overlapping priorities, 24 research priorities were redistributed for scoring. Forty-eight patients or carers with experience of aortic disease participated in the scoring exercise and the results are shown in Table 3.

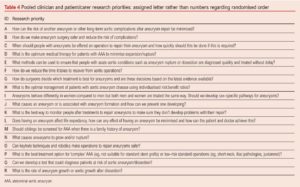
Prior to the workshop, the SIG team pooled clinician and patient/carer research priorities, resulting in a list of 18 for discussion (Table 4). In order to reduce risk of bias, these priorities were randomly ordered and each assigned a letter (rather than a number).
Final prioritisation workshop
The final prioritisation process was conducted via a virtual online meeting on 13 April 2021. It was attended by four patients and carers and eight healthcare professionals, with an additional five observers. The final prioritisation resulted in a final ‘top 10’ research priority list (Table 5). The priorities are ordered according to importance as determined by the workshop. There was general consensus that the list correctly represented the discussions and viewpoints which occurred in the breakout groups.

Discussion
Summary
Ranked research priorities in aortic disease have been clearly highlighted in a way that combines the opinions of all those involved. This robust method is designed to ensure alignment of priorities between clinicians and patients, mitigating disparity between what is deemed important by different perceptions.
Strengths and limitations
The JLA process is acknowledged to be a snapshot in time, and a different group of participants may have determined an alternative collection of priorities. To mitigate the impact of this, it is important that not all aortic research is limited to addressing the top 10 priorities. Additionally, in order to add new voices and thoughts, it is essential to include patients and representatives at all stages of research planning and delivery. The use of virtual platforms for the prioritisation workshops had potentially both positive and negative impacting factors by both facilitating and hindering participation. Travel challenges (eg, frail patients, large geographical distances) were essentially negated by this process. Technical literacy requirements and access may have limited certain participation. Workshop feedback gathered from a follow-up survey was positive overall. Most participants expressed that they enjoyed the process and found it provided an opportunity to learn from others. Some participants highlighted their personal preference for priorities that were excluded from the final top 10 or a preference for a different order; however, this is not uncommon for PSPs that use a consensus approach. There were comments regarding requests to further edit and merge some of the priorities due to perceived overlap. This was addressed directly during the workshops where emphasis was placed on respecting the methodology that had gone before in summarising priorities for the workshop. Most participants found the online format and length of the workshop acceptable, but it was suggested that the final session could have been longer to allow the new groups to fully discuss the rearranged priorities.
Implications for future research
Each of the top 10 priorities identified through this extensive process must now be scrutinised to determine the appropriate related research priorities, how these relate to existing evidence and current research, and what research design best addresses these priorities. Finally, it is hoped that funding bodies and decision makers will direct funding towards these priorities and increase investment in the delivery of new studies in these areas of greatest need and highest impact.
Conclusion
This collaborative effort between healthcare professionals and patients has identified the top 10 research priority areas focused on aortic disease which will guide researchers, clinicians and funders for the foreseeable future. The patient perspective In Table 6 each priority has been presented using terminology to improve clarity and understanding.

Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(2):34-41
Publication date:
February 16, 2022
Author Affiliations:
1. Junior Clinical Fellow, Department of Surgery and Cancer, Imperial College Healthcare NHS Trust, Queen Elizabeth the Queen Mother Wing (QEQM), St Mary’s Hospital, London, UK
2. Professor of Vascular Surgery, Department of Cardiovascular Sciences, University of Leicester, BHF Cardiovascular Research Centre, Glenfield General Hospital, Leicester and NIHR Leicester Biomedical Research Centre, UK
3. Clinical Reader, Department of Surgery & Cancer, Imperial College London and Consultant Vascular Surgeon, Imperial Vascular Unit,
Imperial College Healthcare NHS Trust, St Mary’s Hospital, London, UK
4. Vascular PSP Coordinator, Hull York Medical School, University Road, Heslington, York, UK
5. Adviser at James Lind Alliance, National Institute for Health Research (NIHR)











