ORIGINAL RESEARCH
Research priorities in diabetic foot disease
Collings R,1 Shalhoub J,2 Atkin L,3 Game F,4 Hitchman L,5 Long J,5 Gronland T,6 Russell D7
Plain English Summary
Why we undertook the work: More research is needed to help improve treatment and delivery of care for people with vascular conditions but funding is limited. The Vascular Society of Great Britain and Ireland (VSGBI) ran a Priority Setting Process (PSP) to find out the most important research questions. This helps researchers to better focus their work and helps funders to direct their support to projects that aim to answer these important questions. This paper presents the results of this process, focusing on research priorities related to diabetic foot problems.
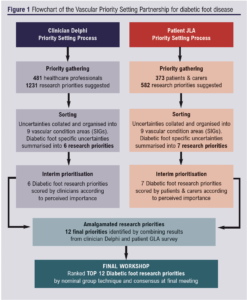
What we did: We asked vascular patients and healthcare professionals in separate surveys to suggest their own priorities for vascular research. Responses were summarised and organised into nine overall vascular condition areas. Summary questions were then sent out to the same participants for scoring. The lists of patient and professional priorities were then combined into a shared list for discussion at a final workshop meeting where a mix of patients and their carers with lived experience of diabetic foot problems and healthcare professionals agreed the ‘Top 12’ research priorities for preventing and managing diabetic foot problems research in the UK.
What we found: A total of 481 healthcare professionals and 373 patients or carers submitted research priorities about vascular conditions, which were consolidated into a final combined list of 12 priorities specifically about preventing and managing diabetic foot problems. At a final workshop involving patients, carers and clinicians, these priorities were put into a ‘Top 12’ list ranked according to perceived importance. There was a notable difference between participants who thought risk assessment and prevention of diabetic foot disease was most important and those who felt treating diabetic foot disease and improving outcomes was key. Many participants individually remarked that there was significant overlap between research questions.
What this means: The most important research priorities for the prevention and management of diabetic foot problems have been identified. Researchers and funders are encouraged to focus on addressing these priorities and supporting studies in these areas.
Abstract
Introduction: Diabetic foot disease is a life-changing event for patients and is associated with high burdens to society in terms of cost, mortality and morbidity. The Vascular Society Diabetic Foot Specialist Interest Group (VSDFSIG), in association with the James Lind Alliance (JLA), aimed to identify and develop key research priorities for preventing and managing diabetic foot disease.
Methods: A modified JLA Priority Setting Partnership was undertaken. Two separate processes to identify research priorities were undertaken with healthcare professionals and patients and carers, led by the VSDFSIG. This exercise produced a list of 12 research priorities. The final workshop was attended by patients, carers and healthcare professionals from a variety of backgrounds involved in the care of people with diabetes and foot pathology. The research priorities were graded to produce a final list of ranked priorities. A final sandpit event addressed the priorities to generate research projects or programmes of research.
Results: A total of 481 healthcare professionals and 373 patients and carers submitted over 100 research priorities relating to diabetic foot disease. These related to diabetic foot disease prevention (including prevention of recurrence and amputation), improving foot outcomes (treatment, risk assessment, blood flow, health promotion) and determining factors that affect healing time (delays in referral, foot infection, antibiotics, larval therapy). Four themes were discussed at the sandpit event relating to potential research projects.
Conclusions: The top 12 research priorities in the prevention and management of diabetic foot disease and potential research projects that will inform researchers, clinicians and funders on the direction of future research priorities are presented.
Introduction
Diabetic foot disease is among a number of serious complications of diabetes mellitus.1 In the UK there are over 7,000 diabetes-related lower limb amputations each year.2 Diabetic foot ulceration (DFU) precedes diabetes-related lower limb amputations in 80% of cases, with studies reporting a prevalence of DFUs as between 1%3 and 2%4 in people living with diabetes in the UK. Fifty percent of people with diabetes who have suffered a foot ulceration will not live beyond five years.5
The Global Burden of Disease study ranked diabetes mellitus-related lower extremity complications as 10th on a scale of leading causes of global years lived with disability in 2015.6 In 2014–2015, the estimated cost attributed directly to DFU and lower limb amputation in the National Health Service (NHS) in England was between £972 million and £1.13 billion.7 Increased personal and societal costs in terms of psychosocial and physical behaviours8 and reductions in quality of life9,10 are also important.
In an attempt to improve the health outcomes and reduce the burden of diabetic foot disease, the Vascular Society of Great Britain and Ireland (VSGBI) created the Vascular Society Diabetic Foot Specialist Interest Group (VSDFSIG) in October 2019. The VSDFSIG comprises a multi-disciplinary team of health professionals alongside patients and/or their carers with an interest in furthering research activity in the field of preventing and managing diabetic foot disease.
One of the first objectives of the VSDFSIG was to establish the research priorities in the prevention and management of diabetic foot disease in the UK. However, there is frequently a mismatch between patients and carers with lived experience of diabetic foot problems and health professionals in selecting and deciding the most relevant research priorities.11 Bridging this divide is essential to ensure any research is impactful and of relevance to policy makers and research funders.12
The James-Lind Alliance (JLA) Priority Setting Partnership (PSP) is one such approach to overcome the divide by bringing together patients, their carers and health professionals to identify and prioritise ‘evidence uncertainties’ in specific conditions or areas of healthcare.13 The PSP methodology aims to make patients and carers as empowered as health professionals in all stages of the process. Using the modified JLA PSP, we aimed to identify and prioritise the most important clinical research priorities in the field of diabetic foot disease, to guide the future research objectives of the VSDFSIG.
Methods
Using a modified version of the JLA PSP methodology, the aim was to identify and prioritise the most important diabetic foot disease prevention and management research questions. There were also questions about treatment, communication, education, assessment, service provision and diabetic foot clinical pathways. There was no formal requirement for ethics approval as the JLA PSP methodology is considered public and patient involvement in research and is not research in itself.
The VSDFSIG is a multidisciplinary team comprised of: vascular surgeons and trainees; diabetes physicians; podiatrists; podiatric surgeons; orthopaedic foot and ankle surgeons; vascular nurse specialists; and trial methodologists, all with experience of delivering diabetic foot research, in combination with patient representatives. The VSDFSIG combined with a support team from the Vascular Society and JLA to deliver the research prioritisation partnership.
A health professional-led priority setting process had previously been undertaken by the VSGBI to identify specific research priorities associated with diabetic foot disease prevention and management, details of which have been published previously.14 A Delphi consensus methodology was used and this process was completed in 2018.
Patient/carer-led research question identification process
A VSDFSIG and JLA-led priority setting partnership was delivered as part of a wider VSGBI initiative, details of which have been published previously.15 In brief, a first round of survey was open from August 2019 to March 2020 and invited any patients and carers who had been affected by vascular-related disease to submit their priorities for research (Figure 1). The survey was made available in electronic and paper format and was publicised via the following membership bodies; VSGBI, The Society of Vascular Nurses, The Society of Vascular Technicians of Great Britain and Ireland, the Rouleaux Club, BACPAR and BSIR. The survey was also promoted via twitter and in affiliated organisation group newsletters and websites. Similar responses were amalgamated, summarised and duplicates removed. A second round of prioritisation took place from November 2020 to January 2021 and asked participants to rate the importance of the summary list of research priorities using a Likert scale (scores ranged from ‘not at all important’ to ‘extremely important’).
Final consolidation workshop
The final prioritisation process was conducted via a virtual online meeting on 14 June 2021. Nine patient and carer attendees with lived experience of diabetic foot problems were recruited via direct contact from members of the VSDFSIG. Nine healthcare workers were recruited via direct communication with national bodies (eg, VSGBI, Royal College of Podiatry) and via direct links with members of the VSDFSIG.
The workshop was facilitated by the JLA and VSGBI. Members of the VSDFSIG (DR, JS, RC, LA) provided general support during the process, but had no influence over the process of priority setting, observed all sessions (muted with cameras off) and noted key points arising from the discussion.
The seven patient and carer research priorities from the JLA PSP were merged with the six priorities from the health professional PSP, and after removal of a duplicate question, 12 were taken forward to the final prioritisation workshop. One week prior to the workshop, the 12 research priority questions were circulated to attendees. Attendees reviewed and ranked the research questions in order of importance prior to the meeting.
The workshop commenced with an overview of the JLA process. Attendees were divided into three ‘breakout’ groups, each comprising a mix of patients/carers and healthcare professionals. Each breakout group was led by an experienced facilitator skilled in the JLA process.
In the first breakout session, each participant presented their ‘top 3’ and ‘bottom 3’ of the final research priorities. In the second breakout session, having heard a range of perspectives, the same groups were asked to arrange the priorities into a ranked order (numbered 1–12) by mutual discussion. The JLA facilitators collated the priority rank order from each group to generate a combined priority rank order of the research questions.
In the third breakout session, attendees were assigned to different groups for a third round of discussion based on the combined priority rank order, and encouraged to review the order in light of new perspectives. The results of each group’s rank orders were again combined to create a final ordered list. The finalised list of top 12 research priorities was presented to participants in the final workshop plenary to facilitate for reflection and comment.
Results
Results from the clinician-led research priority identification and prioritisation
A total of 481 clinicians submitted 1,231 research priorities relating to vascular surgery in general, of which 75 diabetic foot-related research priorities were submitted. These were reduced to six overarching summary priorities that were recirculated for scoring in the second round of the Delphi consensus.
Patient/carer-led research priority identification and prioritisation
There were 26 priorities related to diabetic foot submitted among 582 research priorities from 373 participants in the first round. Of these, five were excluded as they were individual patient specific and six were moved to other Vascular Society SIGs (3 wound, 3 amputation). The remaining 15 priorities were consolidated into seven overarching research priorities by the VSDFSIG chair and PPI representatives.
Final consolidation workshop
As part of the JLA PSP process, the VSDFSIG agreed a list of 12 research priorities (Table 1), derived from the initial survey responses prior to the workshop. The priorities were ordered randomly to reduce the risk of influencing bias and each was assigned an identifying letter (rather than a number).
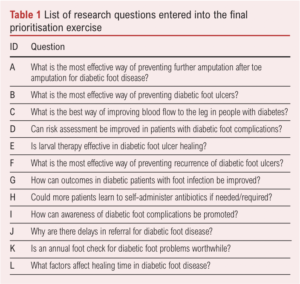
Following drop-outs on the day, the final consolidation workshop was attended by eight patients/carers and eight healthcare professionals, with an additional four observers from the VSDFSIG. The final top 12 research priority list, in rank order of importance, was defined (Table 2). The third priorities both scored the same score and are therefore ranked equal. Although the original aim was to determine the top 10 priorities, the group felt that all 12 research priorities merited inclusion in the final list.

A number of key points were prominent during the discussions in the workshop. There was a notable difference between participants who thought risk assessment and prevention of diabetic foot disease was most important (priorities 1, 2, 3a, 6, 7 and 10) and those who felt treating diabetic foot disease and improving outcomes was key (priorities 3b, 8, 5, 11, 12). Many participants individually remarked that there was significant overlap between research priorities. For example, priorities 1 and 7 concerned prevention of DFU.
Throughout the discussion, patients/carers expressed frustration with medical terminology, whilst also highlighting a desire to introduce specific timelines into priorities (eg, How long will it take a diabetic foot ulcer to heal?).
After prolonged discussion, the two research priorities numbers 11 (‘Could more patients learn to self-administer antibiotics if needed/required?’) and 12 (‘Is larval therapy effective in diabetic foot ulcer healing?’) were also included. Participants felt that both priorities remained important and are available to be researched.
Sandpit event
Six weeks following the final consolidation workshop, a sandpit event was organised to kick-start the process of generating research projects or programmes of research to address the priorities. This was again conducted online and attended by 16 participants, a mix of clinicians and patients with lived experience of diabetic foot problems. Furthermore, the former comprised a mix of clinical disciplines including vascular surgery, orthopaedic surgery, podiatry and diabetology. Prior to the meeting a mapping exercise was performed by VSDFSIG members to identify past, current and planned research against each research priority to identify the research gaps. Participants split into two groups of similar composition to independently discuss four themes (Table 3) which consider both the priorities and research gaps. Following discussions within the two groups, all participants reconvened and the emerging points were shared and discussed further amongst the complete group. Some of the key points are summarised in Table 3. It was clear that there was overlap and inter-dependence of the themes.

Discussion
Using a modified JLA PSP methodology, we identified and ranked the principal 12 research priorities in the prevention and management of diabetic foot disease. A two-round process produced 12 priorities for final ranking. Following discussion, consensus was reached with patients, carers and healthcare professionals to produce a top 12 ranked list of clinical research priorities in the prevention and management of diabetic foot disease.
Strengths and limitations
The strengths of this process include the use of the structured and modified JLA PSP process to integrate patients, carers and health professionals’ perspectives on the research priorities in the prevention and management of diabetic foot disease. Facilitation by skilled JLA advisors ensured that all participants contributed actively to the workshop and discussions.
Whilst the VSDFSIG attempted to include a range of participants from different geographical, socioeconomic and different lived experiences of diabetic foot disease, it is recognised that participants might not be truly representative of all stakeholders. However, this was mitigated by implementing the role of VSDFSIG who were able to provide a dedicated review of survey responses and highlight if there were any expected topic areas that could have been missed. Secondly, the risk of responder bias is prominent in this type of research that can limit the generalisability of any findings.
Implications for future research
Establishing the top 12 clinical research priorities will inform the future strategy of the VSDFSIG in contributing to the evidence base for the treatment and management of diabetic foot disease. These priorities will influence researchers and funders to ensure that the most important research priorities for both healthcare professionals and patients are considered. Furthermore, the themes and key points distilled through the subsequent sandpit event are available to the diabetic foot research community as key elements to take forward. The VSDFSIG are available to support any researchers interested in developing research proposals to answer these priorities.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(4):124-129
Publication date:
July 4, 2022
Author Affiliations:
1. Torbay and South Devon NHS Foundation Trust, Torquay, UK
2. Imperial Vascular Unit, Imperial College Healthcare NHS Trust, St Mary’s Hospital, London, UK
3. Mid Yorkshire NHS Trust, Wakefield and University of Huddersfield, Huddersfield, UK
4. Royal Derby Hospital, University Hospitals of Derby and Burton NHS FT, Derby, UK
5. Academic Vascular Surgical Unit Vascular Labs, Hull York Medical School, Hull, UK
6. James Lind Alliance Advisor, National Institute of Health Research, Leeds, UK
7. Leeds Institute of Clinical Trials Research, University of Leeds and Leeds Vascular Institute, Leeds Teaching Hospitals NHS Trust, Leeds, UK
Corresponding author:
Dr David Russell
Leeds Institute of Clinical Trials Research, University of Leeds and Leeds Vascular Institute, Leeds Teaching Hospitals NHS Trust, Leeds, LS2 9JT, UK
Email: [email protected]











