ORIGINAL RESEARCH
Research priorities for venous conditions: results of the UK Vascular James Lind Alliance Priority Setting Process
Long J,1,2 Atkin L,3,4 Gronlund T,5 Lane T,6 Nandhra S,7,8 Wilton E,9 Carradice D,1,2 on behalf of the Vascular Society of Great Britain and Ireland Venous Special Interest Group
Plain English Summary
Why we undertook the work: More research is needed to help improve care for people with venous conditions, but funding is limited. We ran a Priority Setting Process (PSP) to identify the most important research priorities to improve patients’ lives, and generated a ‘top 10’ list. This list will help focus research and funding on areas that matter most to patients, carers and healthcare teams.
What we did: Patients and healthcare professionals participated in rounds of survey and were asked to suggest priorities for vascular research. Responses were summarised and organised into nine overall vascular condition areas. Summary priorities were then sent out in a second survey for scoring according to order of importance. The lists of patient and professional priorities were then combined into a shared list for discussion at a final workshop meeting where a mix of patients and healthcare professionals agreed the ‘top 10’ research priorities for venous condition research in the UK.
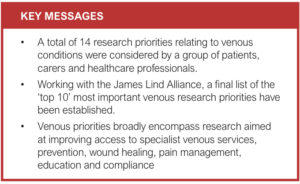
What we found: Research priorities about vascular conditions were submitted by 481 healthcare professionals and 373 patients or carers. A final list of 14 priorities specifically about venous conditions were discussed at a final workshop involving patients, carers and clinicians, and put into a ranked ‘top 10’ list according to perceived and shared importance. Research priorities relate to: access to venous specialist services, prevention, wound healing, pain management, education and compliance.
What this means: Research priorities have been identified by patients and health professionals with lived experience of venous conditions. Researchers and funders are encouraged to focus on addressing these priorities and supporting studies in these areas.
Abstract
Introduction: Venous disease comprises a range of conditions of varying severity, which can result in pain and discomfort and a reduced quality of life. The annual costs for the treatment and management of venous disease in the UK is in the order of billions of pounds. It is vitally important to direct finite National Health Service (NHS) funding into areas that will maximise health outcomes and reduce the burden on the NHS. To address the issue of where best to target resources and research, the Vascular Society of Great Britain and Ireland (VSGBI) in association with the James Lind Alliance (JLA) undertook a national Priority Setting Process (PSP) for vascular conditions. This paper presents the results of this process, with a focus on the topic of ‘venous conditions’.
Methods: A modified JLA Priority Setting Partnership was developed to gather clinician, patient and carer research priorities for vascular conditions. Consensus workshops were held to discuss clinician and patient priorities and agree a list of joint research priorities. Consensus was achieved using the nominal group technique and a ranked ‘top 10’ list of research priorities for venous conditions was established.
Results: In the first phase (clinician-led survey), 481 clinicians submitted 1,231 research questions related to vascular conditions in general. Of these, 130 venous-specific research priorities were reduced to 13 overarching summary priorities recirculated for interim scoring. In the second phase (patient and carer-led survey), 373 patients and carers submitted 582 research priorities. Of these, 101 venous-specific priorities were reduced to 22 overarching summary priorities and recirculated for interim scoring. In the third phase (consensus workshop), clinician and patient priorities were amalgamated into 14 priorities for discussion. The final ‘top 10’ list of venous condition research priorities relate to: access to specialist venous services, prevention, wound healing, pain management, education and compliance.
Conclusions: The ‘top 10’ venous-related priorities demonstrate the research areas considered to be most important from the perspective of patients, carers and healthcare professionals. Researchers can now focus their efforts on developing research questions and studies to address these priorities and funders should increase their investment to support new studies in these areas of greatest importance.
Background
Venous disease encompasses a range of conditions that vary in severity and, if left unmanaged, can lead to serious conditions such as leg ulcers. This presents a huge economic burden to the NHS, estimated to be between £1bn and £3bn per year for ulcers alone.1–3 Venous disease can negatively impact on quality of life with issues such as pain, restricted mobility and reduced psychosocial functioning.4-6
Despite a wide range of treatment options and guidelines, questions still remain unanswered about the efficacy and cost effectiveness of different interventions, with uncertainty over a selection of treatments.7-11 In a recent report published by the All-Party Parliamentary Group for Vascular and Venous Disease, the data show that more than half of clinical commissioning policies (64%) do not provide access to venous treatment in line with NICE guidance, and pathways for venous conditions do not exist in a significant number of NHS Trusts.12-15
In order to ensure optimal management of venous conditions, more research is needed; however, funding is limited and highly competitive. Funding bodies need to ensure their limited investment is directed to areas with the greatest potential for improving clinical services and health outcomes, whilst avoiding research waste.16 Priority Setting Processes (PSPs) are an increasingly popular method to address this issue; they systematically identify and prioritise research gaps and are seen as an effective way of highlighting important topics for funding consideration.17
The Vascular Society of Great Britain and Ireland (VSGBI) initiated a national PSP for vascular conditions in association with the James Lind Alliance (JLA) who specialise in facilitating patient involvement in research.18 Prior to this there was no agreement for research priorities within the vascular specialist community. The aim of the Vascular PSP was to survey vascular health professionals, patients and carers to identify and prioritise the most important research priorities. This paper presents an overview of the vascular condition PSP, focusing on the recommendations for venous-related priorities and implications for future research in this area.
Methods
A detailed description of the process has been provided previously.19-25 A summary of the process is outlined below and presented in Figure 1.

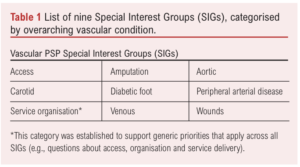
The VSGBI undertook a research PSP in association with the JLA to identify research priorities for vascular conditions. The work was overseen by a steering committee involving representation from all the leading UK Vascular Societies and patients. Nine overarching vascular condition Special Interest Groups (SIGs) were established to help support the process and ensure that each area retained their important research priorities (Table 1).
Initially, due to resource limitations, a clinician-led Delphi survey was conducted to produce a list of research priorities to reflect the opinions of vascular healthcare professionals. This was followed by a separate patient and carer focused JLA survey to identify important research priorities from the perspective of vascular patients and carers. The two processes were then brought together at final workshops held separately for each SIG, where patients, carers and clinicians worked together to agree a shared list of ‘top 10’ research priorities.
Scope of the Venous SIG
The remit of the Venous SIG is to support research into the care of patients with venous conditions. The Venous SIG aims to develop the list of top 10 priorities into funded venous research studies that address these important areas.
Clinician-led research Priority Setting Process
Healthcare professionals were surveyed using a modified Delphi approach that consisted of two rounds:
Survey Round One: In the first round, an open-ended survey invited participants to submit their priorities for vascular research. An electronic link to the survey was emailed via the following membership bodies: The Vascular Society of Great Britain, The Society of Vascular Nurses, and The Society of Vascular Technicians of Great Britain and Ireland and the Rouleaux Club. Letters including the survey link were sent to each vascular unit registered on the National Vascular Registry (NVR) and the survey was also promoted via twitter. Responses were collated and categorised into pathological topics and research themes by a core subgroup of the steering committee. Similar responses were amalgamated and summarised into an overarching priority. Responses considered out of scope (eg, too broad or logically unclear) were removed and remaining priorities checked for current evidence.
Survey Round Two: The refined list of priorities was redistributed in a second survey for scoring. Participants were asked to rate the importance of the summary priorities on scale of 1–10 (1 being the least important, 10 being the most important). This process was completed in 201821 and the results of clinicians’ venous-related priorities are summarised in Table 2.

Patient/carer-led research Priority Setting Process
Vascular patients and carers were surveyed using a modified JLA approach, with guidance from a JLA advisor and used similar methodology as the clinician-led PSP.
Survey Round One: In the first round, a survey invited patients and carers to submit their own research priorities. The survey was provided in paper and electronic format and advertised to UK-based societies involved with care of vascular patients. Participant packs were sent out to vascular units and included paper surveys with freepost return address and promotional materials such as posters and postcards that could be left in waiting areas. The survey was also advertised via social media (twitter), websites and newsletters. Responses were categorised and delegated to each SIG for further review. Similar responses were amalgamated and summarised into an overarching priority. Responses considered out of scope (eg, too broad or logically unclear) were removed and remaining responses checked for current evidence.
Survey Round Two: The refined list of priorities was redistributed in a second survey for scoring. Participants were invited to rate the importance of research priority using a 5-point Likert scale (scores ranging from 1 = “not at all important” to 5 = “extremely important”). This process was completed in 2020 and the results of patient and carer venous condition priorities are summarised in Table 3.

Special Interest Group Prioritisation Workshops
For each SIG, the results of the clinician and patient/carer-led interim prioritisation processes were combined. Similar or duplicated priorities were amalgamated and any technically worded language from the clinician priorities was revised with patient input. Care was taken to ensure that the original substance of the priority remained. This process generated a refined list of joint priorities for discussion at individual SIG workshops.
The final prioritisation workshop for venous conditions was conducted virtually using the Zoom platform to accommodate COVID-19 restrictions. All attendees (including healthcare professionals, patients and carers) were recruited via direct contact or were approached if they expressed an interest during the initial prioritisation process. Participants were sent details of the workshop, an agenda and a list of the research priorities to be discussed in advance. Prior to the workshop, participants were asked to consider the combined list of clinician and patient research priorities shown in Table 4, and to rank them in order of importance from 1 (most important) to 14 (least important).

The workshop was led by two experienced JLA advisers, a JLA coordinator and a technical lead who were skilled in the JLA PSP process and leading such workshops. Members of the venous SIG attended as observers and to provide support to attendees if required (they would join a separate breakout room). SIG members were not directly involved in the priority setting and had no influence over the final agreed list of priorities. Following welcome and introductions, participants were split into two breakout rooms which consisted of a mix of patients and healthcare professionals. Small group discussions were facilitated by an advisor and followed a nominal group technique to reach a consensus for an ordered list of ‘top 10’ priorities.
First round of discussion: Participants shared their top three and lowest three priorities with a brief explanation for why. This was followed by an open discussion about similarities and differences and any priorities that were not initially mentioned.
Second round of discussion: The JLA facilitator presented on screen a potential order of questions based on initial feedback and discussion. Participants had an opportunity to reconsider their initial placement of priorities whilst the facilitator moved priorities on screen to reflect an agreed order of priorities 1–14.
Third round of discussion: The ranked priorities of the two separate groups were combined by the lead facilitator using a geometric mean of the respective ranked positions. All participants came together as one group and the lead facilitator presented the combined results of the group rankings. Participants were then split into new groups and, again, participants had an opportunity to reconsider the order of priorities before reaching a final ranked ‘top 10’ list of venous research priorities. As before, the ranked priorities of the separate groups were combined to form a final shared ranking.
Results
Clinician research priority identification and prioritisation
A total of 481 clinicians submitted 1,231 research priorities relating to vascular surgery in general. Of these, 130 venous condition-related research priorities were submitted, 28 of which were excluded outright as they were too specific to single patient experience or there was no apparent priority (eg, nonsensical or broad statement). The remaining 102 priorities were combined and summarised into 13 clinician priorities for scoring, the results of which are shown in Table 2.
Patient/carer research priority identification and prioritisation
A total of 373 patients/carers suggested 582 research priorities related to vascular surgery in general, of which 102 responses were specific to venous conditions. After data cleaning (eg, removing nonsensical suggestions, separating out submissions with multiple suggestions and combining overlapping priorities), 22 research priorities were redistributed for scoring, the results of which are shown in Table 3.
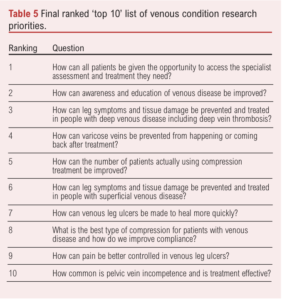
Prior to the workshop, the SIG team pooled clinician and patient/carer research priorities and, after removing duplicate questions, 14 were taken forward for discussion at the final workshop (Table 4). In order to reduce risk of bias, these priorities were randomly ordered and each assigned a letter (rather than a number), before they were circulated to attendees in advance. Attendees reviewed and ranked the research questions in order of importance prior to the workshop.
Final prioritisation workshop
The final prioritisation process was conducted via a virtual online meeting on 27 September 2021. It was attended by two patients and six healthcare professionals (specialist vascular nurses and vascular surgeons) with four observers. The final prioritisation resulted in a final ‘top 10’ research priority list (Table 5). The priorities are ordered according to importance as determined at the workshop. There was general consensus that the list correctly represented the discussions and viewpoints which occurred in the breakout groups. Results from the participant feedback indicated that 100% agreed or strongly agreed that the process for determining the top 10 priorities was robust and fair.
Discussion
The ‘top 10’ research priorities for UK venous conditions research have now been established. Using a modified JLA methodology, vascular healthcare professionals and patients with lived experience of venous conditions have jointly agreed the most important priorities for future research in this area. The four priorities that did not make the ranked ‘top 10’ list are still considered important.
Overarching themes within the final ‘top 10’ list relate to access to services, prevention, wound healing, pain management, education and compliance.
Strengths and limitations
The Vascular PSP used well established methods throughout, with oversight from a multidisciplinary steering committee. The Delphi method, often used in PSPs, is regarded as a flexible research technique but one that tends to focus on the identification of expert opinion.26 To mitigate this, the Vascular PSP sought the input of the JLA who provide a transparent and structured framework that emphasises patient participation in PSPs, with patients having an equal voice to clinicians and researchers in influencing the research agenda.27,28 It is possible that the modified approach of having two separate processes before bringing the clinician and patient views together may have resulted in a different ‘top 10’. However, during the amalgamation process there was already considerable of overlap with similar questions and the format of the final workshops did establish shared priorities.
Due to the nature of survey data collection, there is potential for responder bias,29 and consideration was given to whether responses would be adequately reflective of the opinions of people with lived experience of venous conditions and those treating them. Under-representation is recognised as a limitation of many PSPs,30,31 and therefore there may have been potentially relevant priorities not submitted and consequently not considered within the analysis. However, the value of PSPs is not in their universal coverage, but in eliciting some new insight and perspectives, especially from people with lived experience.
The Vascular PSP sought to minimise this risk in several ways. The survey was made available in electronic and hardcopy format (with freepost address), and it was promoted via the affiliated charity groups and organisations who regularly work with the population targeted for input. Furthermore, the introduction of SIGs meant that each vascular condition area had a dedicated review of responses by a group of interested professionals and patients that could highlight if there were any expected topic areas missing.
Most workshop participants found the use of a virtual platform acceptable, although it is recognised that potentially lack of access to IT may have limited participation and altered representation. On the other hand, the virtual platform meant patients did not have to travel, and this may have made the workshop more accessible for some patients. Positive comments collected from the feedback survey following the final workshop demonstrated that clinicians and patients found the process of discussing priorities in mixed groups a positive and worthwhile experience. It gave participants an opportunity to hear about the experiences of others and to reassess their initial judgements.32 Although the mixed discussion groups were not strictly balanced in terms of patient attendance, this was carefully moderated through the skilled JLA facilitators who ensured that patient participants were regularly included and able to contribute their views. The final ranking was acknowledged as a compromise, but all participants had some of their high ranked priorities in the final ‘top 10’. This is not uncommon for PSPs and is a known factor of a consensus approach.
Implications for future research
The venous condition priorities now provide researchers with essential guidance on where best to focus their efforts in the immediate and long term. Studies and projects should now be developed to address these important priorities and we call on funders to recognise and support the delivery of this work.
Conclusion
The Vascular PSP has established a ‘top 10’ list of priorities for UK venous conditions research from the shared perspective of vascular patients, carers and health professionals. Researchers and funders can confidently invest resources into these areas of venous conditions research with reassurance that they are clinically relevant and of practical importance to patients.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;2(1):26-32
Publication date:
November 21, 2022
Author Affiliations:
1. Hull University Teaching Hospitals NHS Trust, Hull, UK
2. Academic Vascular Surgical Unit, Hull York Medical School, Hull, UK
3. Division of Podiatry and Clinical Sciences, University of Huddersfield, UK
4. Vascular Nurse Consultant, Pinderfields Hospital, Wakefield, UK
5. James Lind Alliance, UK
6. Imperial College Healthcare NHS Trust, London, UK
7. Population Health Sciences Institute, Newcastle University, Newcastle upon Tyne, UK
8. Northern Vascular Centre, Freeman Hospital, Newcastle upon Tyne, UK
9. Oxford University Hospitals NHS Foundation Trust, Oxford, UK
Corresponding author:
Judith Long
Vascular Office, 2nd Floor,
Allam Diabetes Centre,
Hull Royal Infirmary,
Anlaby Road, Hull, HU3 2JZ, UK
Email: [email protected]











