ORIGINAL RESEARCH
Patient-reported quality of life factors in vascular surgical wounds healing by secondary intention (SWHSI): a qualitative patient and public involvement (PPI) exploration
Sidapra M,1 Ramakrishnan P,2 Siracusa F,1 Walshaw J,1 Long J,1 Arundel C,3 Chetter I1
Plain English Summary
Why we undertook the work: There are times when surgical wounds cannot be closed with staples or stitches after an operation because of infection or other concerns about the wound (called ‘open surgical wounds’ or ‘surgical wounds healing by secondary intention’ (SWHSI)). In these situations, these wounds are often allowed to heal naturally and monitored by the healthcare team in the community. To understand how living with open surgical wounds affects the patient’s day-to-day life, we brought together a group of patients and carers with experience of this.
What we did: We identified 12 patients with experience of living with a SWHSI, along with those caring for a person with a SWHSI. Two small informal focus group sessions were conducted over a 1-month period, guided by the research team. These sessions were recorded, transcribed and were analysed for common themes amongst the group discussions.
What we found: After analysing the group discussions, we found that the impact of SWHSIs on quality of life in these patients could be divided into four main categories: mental health, physical symptoms, lifestyle symptoms and service-based impacts. We also found that people experienced these symptoms differently and to varying extents.
What this means: This exploration helps us to better understand the experience of living with a SWHSI and will help us target future research into tackling the areas that impact patients the most. This may include targeting new treatments or services to improve areas that cause the biggest negative impacts on quality of life.
Abstract
Background: Surgical wounds healing by secondary intention (SWHSI) represent a significant burden to patients and services. An understanding of quality of life factors affecting this population is essential to recognise the impact of this wound entity on patients. Understanding of the patient experience is necessary to building effective services and designing high-quality research studies to improve care in this population.
Methods: Twelve individuals with lived experience of living with a SWHSI or caring for a person with a SWHSI were recruited to one of two focus groups. Participants were identified from those who had previously been recruited into the NIHR-funded SWHSI-2 trial (NIHR17/42/94; a study assessing healing of surgical wound healing by secondary intention). All participants in this cohort had lower limb SWHSIs and a history of peripheral vascular disease. Sessions followed a general topic guide and were guided by the research team. Sessions were audio-recorded, transcribed and analysed using thematic analysis methods.
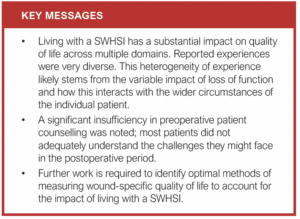
Results: Four main areas of impact on quality of life were identified: mental health, physical symptoms, lifestyle symptoms and service-based impacts. There was a clear heterogeneity of experience seen within the group, with some reporting a more significant impact than others. This was ascribed to the loss of social and professional functioning, and the subsequent impact on mental health. There was a differential impact of this on younger participants (who tended to be employed and hold caring roles for children or family members) compared to older participants who did not have these social roles to fulfil, and were less affected in these areas. The need for improved preoperative counselling was highlighted, as many participants reported feeling unprepared for the postoperative course.
Conclusions: This study considered the experiences of patients with a SWHSI and identified the main areas of impact on quality of life. This work will help to underpin future research into treatments and services for the SWHSI population. It may also form the basis for identifying an appropriate patient-reported outcome measure (PROM) related to quality of life in SWHSI for use in the research setting. Limitations of the study included the number and diversity of participants, and the impact of the SARS-CoV-2 (COVID-19) pandemic on the experiences of participants. Further exploration of the area through formal qualitative study is warranted to understand the breadth, generalisability and possible future applications of the work.
Introduction
Over 10 million surgical interventions are performed in the National Health Service (NHS) every year.1 Most surgical wounds are closed by primary intention and the edges of the wound are held together with sutures, staples or glue. In cases of wound infection, contamination, dehiscence or where wound edges cannot be approximated, surgical wounds may be managed by secondary intention, allowing healing to occur from the wound bed up.2,3
Treating surgical wounds in this way can have significant effects on patients’ quality of life. A qualitative study specifically designed to explore patients’ perspectives of living with an open wound found a range of wound-related factors had a detrimental effect on daily life, physical and psychosocial functioning, and wellbeing.4 Participants reported heavy amounts of exudate, malodour and difficulties with personal hygiene due to the wound, which resulted in withdrawal from normal daily activities and socialising. The extended time to healing was difficult for many and all participants interviewed expressed a longing for complete wound healing. Participants reported feeling disconnected from their normal lives and many participants experienced worsening mental health.
This qualitative exploration aims to build on previous work to further analyse and categorise the lived experiences of patients and carers and their ideas, concerns and expectations relating to surgical wounds healing by secondary intention (SWHSI) in the vascular surgery population. In this paper, the phrases ‘SWHSI’ and ‘open surgical wounds’ will be used interchangeably.
Background
Large and robust epidemiological datasets of SWHSI are generally lacking. In recent years, several projects have been conducted to quantify and characterise the population living with open surgical wounds in England.5-8 Hall et al8 surveyed over 1000 people in Leeds, UK and found a prevalence of 0.07 dehisced surgical wounds per 1000 population. Chetter et al5 surveyed 187 patients in Hull and East Riding of Yorkshire and calculated a prevalence of 0.41 SWHSI per 1000 population. For a UK population of 67.3 million people, this amounts to an annual prevalence of approximately 27,500 people living with a SWHSI.
Chetter et al9 conducted a prospective cohort study looking at clinical characteristics, outcomes and quality of life in patients with SWHSI. They found that participants fell broadly into three groups: individuals with abdominal wounds after colorectal surgery, leg/foot wounds following vascular surgery, and a third mixed group. The most prevalent locations for wounds were the abdomen, foot and perianal area.
Physiologically, wound healing occurs in four phases: haemostasis, inflammation, proliferation, and remodelling. There is overlap between these phases and time for each phase will vary based on numerous factors. In the proliferation phase, granulation tissue is formed and fills the wound, edges are pulled together (contraction) and epithelialisation can occur.2 In healing by secondary intention, these four phases still occur but granulation tissue must fill the wound from the bottom up and the wound must contract significantly prior to epithelialisation.3
Management of SWHSIs creates a large burden of care on community and primary healthcare services with a requirement for frequent dressing changes, advanced topical therapies including negative pressure wound therapy (NPWT) and specialised nursing care.10 Occasionally, hospital review or admission may be required for treatment of infection or wound debridement to promote healing.10,11
Evidence for effectiveness of different types of treatment is limited. Vermeulen et al12 summarised the evidence for effectiveness of different dressings and topical agents for SWHSIs. The 13 trials included used a variety of different interventions, control groups and endpoints. Most studies were underpowered. There was insufficient evidence to support any significant difference between types of dressings and topical agents. A Cochrane systematic review summarising evidence on NPWT for SWHSI included only two studies with a total of 69 patients.10 The studies were underpowered, data limited, and risk of biases were unclear.
This lack of effective and accessible treatments to facilitate wound healing in this population means that many patients will live with these wounds and their potential impacts for extended periods of time, with the median time to healing for a SWHSI being 86 days.13 A patient-centred understanding of this experience is essential to allow any future research in this population to be valid, valuable and impactful.
Methods
Patients enrolled within the NIHR-funded SWHSI-2 trial (NIHR17/42/94; a study assessing healing of surgical wound healing by secondary intention) recruited from vascular wards and outpatient clinics, as well as carers and family members, were invited to participate in a patient and public involvement (PPI) focus group exercise exploring their experiences of living with a SWHSI. Patients were approached via telephone call and invitation letter, which included an information sheet regarding the purpose of the recruitment into the focus group. Written informed consent forms were signed on the days of the meetings.
Participants were interviewed in two small focus group sessions of six participants (while maintaining social distancing) over a 1-month period. Funding was provided by the Yorkshire and Humber Research Design Service Patient and Public Involvement grant, and funding constrictions limited the size of the sample we were able to recruit. Participant costs were reimbursed, in addition to a stipend provided according to the NIHR public contributor payment policy for their time.14 The meetings were conducted in an informal manner and consisted of open-ended questions followed by discussion amongst the members. Each session was aimed to last approximately 90–120 minutes. At the beginning of the second session, feedback and ideas from the previous meeting were presented to explore them in detail with the new panel members and gain valuable and meaningful insights. All sessions were recorded with written consent from panel members.
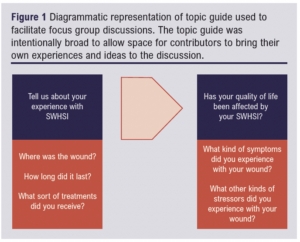
The groups were facilitated by a research doctor and chaired by a senior member of the vascular academic unit. A pre-prepared topic guide was used to guide the conversation (Figure 1).
Following the sessions, the interview transcripts were reviewed by a research doctor and primary coding of key themes for thematic analysis was undertaken. Thematic analysis is a commonly accepted tool for analysis of qualitative data, initially utilised in the field of psychology but now frequently employed in qualitative studies in the health sciences.15 It is distinct amongst qualitative analysis methods as it offers a flexible and pragmatic method of analysis that is not bound to the strict principles of methodology required in other approaches.16 Thematic analysis took a theoretical approach and was based around a research question of “How does having a SWHSI affect quality of life?” This process is presented in Figure 2.
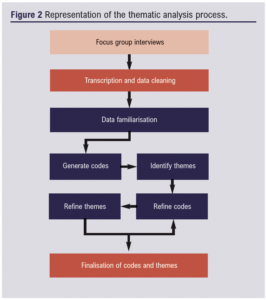 This involved identifying recurring and emphasised ideas, points that elicited a great deal of agreement from the group and ideas that generated significant discord or disagreement. The data were further recoded, with redundant codes eliminated and overly broad codes expanded through multiple cycles until a final list of codes was obtained. This list was felt to encompass the breadth of experience shared in the focus group meetings and reflected the most pertinent data points. These codes were assigned to overarching sematic themes.
This involved identifying recurring and emphasised ideas, points that elicited a great deal of agreement from the group and ideas that generated significant discord or disagreement. The data were further recoded, with redundant codes eliminated and overly broad codes expanded through multiple cycles until a final list of codes was obtained. This list was felt to encompass the breadth of experience shared in the focus group meetings and reflected the most pertinent data points. These codes were assigned to overarching sematic themes.
As these sessions were undertaken as a PP) exercise to inform the foundations of future research, no ethical approval was required in accordance with guidance from the Health Research Authority (HRA).
Results
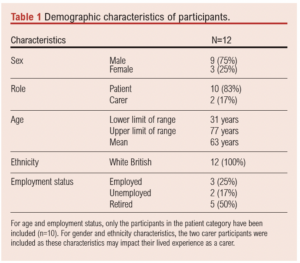
Twelve individuals (nine men and three women) participated in the meetings (Table 1). Two of these members were carers of a patient. The participants of the focus groups were given opportunities to speak to their personal experiences of living with a wound if they so wished; all participants verbally consented to share their stories during the session. Diversity of age, employment status, health status, education and circumstance between the participants allowed for a range of experiences to be heard. A lack of diversity in ethnicity was reflective of the population local to and served by the research centre, and posed a significant limitation to the generalisability of the results beyond a white English population. This is further explored in the Discussion section.
Thematic analysis of the transcripts identified four main domains of impact on quality of health, with 23 sub-themes distilled from 81 primary individual finalised codes (Figure 3).
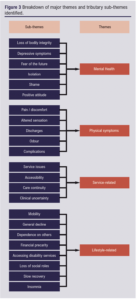
Mental health
A prominent and recurring theme for participants was the effect on mental health; most patients reported that their mental health was affected to some extent by the experience of having an open wound, with severity of impact varying greatly between patients. This was also reflected in the experiences of carers and family members. Participants almost universally reported some level of depressive symptoms, and often these contributed to wider issues with isolation, loss of social functioning and emotional deterioration.
Many patients reported a visceral reaction to the loss of bodily integrity, with feelings of ‘disgust’ reported by multiple participants. This experience was commonly compared to a form of grieving for the previous healthy state and a deep sense of loss. The impact of this was reported to be less keenly felt in those participants who regained the functional capacity of the injured body part (ie, those who were able to return to walking or their normal activities) and retained a mostly cosmetic impairment following healing, while those whose injury was associated with a loss of functioning reported a much greater sense of loss.
Physical
Most patients reported a mixture of physical symptoms, the most common being pain and altered sensation of various kinds. This included perceptions of burning, tingling, itching and a feeling of wetness. Experiences of pain tended to be more common in the acute phases of injury and improved with time and healing, although some patients did report longstanding ‘phantom’ pains and altered sensation.
Participants also described swelling of the affected area and foul-smelling discharge. Often these symptoms were related to wound deterioration or attributed to delays in dressing changes and routine care. Participants strongly linked physical symptomatology to service-related issues and these areas were often spoken about together. Overall, though physical symptoms were common, most participants felt they were more manageable than the psychological impacts of the wound on mental health.
Lifestyle
Lifestyle or general living symptoms encompassed a wide range of impacts reported on the participant’s ability to live, work, socialise and generally function in their daily life as they would have prior to the development of the wound. Patients reported extensive impairments including loss of mobility, difficulty sleeping, loss of independence, financial loss and inability to work.
The severity of impact varied hugely between participants depending on the individual circumstances, family and social support and wider governmental support available to them. The impacts were also not contained to the participant’s singular experience and had a ‘ripple’ effect extending to partners, dependents and employees. Loss of social roles such as that of ‘provider’ or ‘breadwinner’ reduced the ability to participate actively in parenting, and loss of positions of responsibility at work or in wider life were also noted to have significant impacts on this patient group. These impacts were also closely interrelated with issues with mental health and deterioration of general physical health.
Service-related
All participants reported a significant impact on quality of life related to the extensive burden of care involved with an open wound. This included routine interactions with planned care primarily facilitated by community and district nurses, primary care practices and wound care clinics. It also encompassed a level of interaction with unscheduled care including emergency departments, urgent care centres and inpatient services in cases of wound deterioration, or occasionally experiences of wound care in these settings when admitted for management of another condition.
The participants shared a varied range of experiences, some excellent and some poor. Many key themes emerged including unfamiliarity of healthcare staff with managing and dressing wounds. Participants reported often feeling unsupported in their wound management, while also often having to take on an ‘expert’ role when interacting with services that seemed to the participant to be unfamiliar with the requirements of wound care.
Participants also reported the difficulty in scheduling visits, irregular timing of attendances and unreliability of wound care services, resulting in a further deterioration of the participant’s ability to engage in general life. Additionally, the high number of interactions with healthcare staff resulted in a further burden of care.
Participants reported a variety of attitudes towards the level of care they received, with some reporting a feeling of over-interaction with services and others who reported a preference for more frequent reviews.
Discussion
This qualitative exploration of the patient experience of living with SWHSIs identified major recurring themes that would need to be addressed by future wounds research. Participants reported many quality of life aspects that were impacted in living with a SWHSI. Through the process of thematic analysis, these have been summarised into the categories of mental health, physical symptoms, lifestyle symptoms and service-related issues.
Experiences varied depending on the type and location of wounds. All participants interviewed in this exercise had experienced wounds that resulted from a primary diagnosis of peripheral vascular disease and all wounds were located on the lower limb, but even within this subgroup there existed a degree of heterogeneity of experience. This was mostly reflected in how participants interacted with their changed circumstances – some were able to maintain higher levels of mobility, general functioning and participation in their usual daily lives and roles, while others reported experiencing a much greater breakdown in their ability to sustain usual activities and routines. Impairment of individual mobility, restrictions on driving and reduced ability to perform in their usual social roles were highlighted by some participants and identified as a significant psychological burden. Others, whose social roles did not require them to fulfil these specific functions, did not report this particular impact and burden on their lives.
Participants also reported a lack of understanding or forewarning about the probable postoperative course. Given that most of these operations were emergency procedures with a significant risk to life or limb without urgent surgical management, the participants felt satisfied in their understanding that an operation was necessary but discussion amongst the participants revealed that most of them did not fully appreciate what living with a SWHSI might mean for them. Previous studies have shown that almost half of all SWHSIs are planned. However, from our exploration it is clear that there remains a gap in patient education that requires addressing in this population.17
While there is reason to hypothesise that the experiences of other groups commonly experiencing SWHSI may be similar, it must be stated as a clear limitation of this study that participants with other common SWHSIs (eg, from abdominal surgery or perianal wounds) were not represented in the sample. However, studies which have explored the psychological effects of surgical wound complications such as dehiscence, which is often managed by secondary intention following initial wound breakdown, found similar effects in these patient groups as were noted in this exercise.18-20
Impacts on working life were noted to be significant, ranging from the need for extended absence from the workplace through to inability to maintain business functioning and loss of entire businesses. These impacts were more heavily reported in younger participants who often maintained active working lives, while older participants tended to be retired from formal employment. This finding further reinforced the need for appropriate preoperative patient education and counselling, as the wider impacts of the postoperative course on employment and financial considerations were often underestimated.
It was outside the scope of this exercise to attempt to quantify the independent and relative impacts of each of these symptom areas on overall quality of life. However, some aspects – such as poor mental health resulting in feelings of anxiety, stress and severe depression – were emphatically reported and were almost ubiquitous within the interviews.
The focus group exercises were undertaken in October 2021, just as policies from the government and health service regarding the SARS-CoV-2 (COVID-19) pandemic were moving towards reducing precautionary restrictions in healthcare settings, as well as in wider life. However, the experiences recalled during the focus group sessions had occurred while public health measures were in force throughout the UK. The impact of the SARS-CoV-2 pandemic and related measures on the reported experiences of the group cannot be isolated from the overall wound-related experience of the participants, and presents a significant confounding factor in the findings.
Additionally, this exercise was undertaken in East Riding of Yorkshire where 94.6% of the local population identify as white British, English, Welsh, Scottish or Northern Irish.21 All participants in the study were of white British ethnicity, which limits the validity of the findings among the general UK population. It is therefore advised that further qualitative and explorative work is undertaken with a broader sample of the UK population to ensure future research is valid, appropriate and acceptable to the experiences of this population at large.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(3):154-159
Publication date:
March 27, 2023
Author Affiliations:
1. Academic Vascular Surgery Unit, Hull York Medical School, Hull, UK
2. Leeds Teaching Hospitals NHS Trust, Leeds, UK
3. York Trials Unit, University of York, York, UK
Corresponding author:
Misha Sidapra
Academic Vascular Surgery Unit, Hull York Medical School, Allam Diabetes Building, Hull Royal Infirmary, Anlaby Road, Hull, HU3 2JZ, UK
Email: [email protected]











