CASE REPORT
A rare case of a dog bite leading to bilateral lower limb amputations
Jones AE,1 Moore P,2 Frewin R,3 Vardhan V,1 Kulkarni SR1
Abstract
Capnocytophaga canimorsus is a rare cause of bacteraemia, occurring usually after dog bites, and can have devastating consequences for patients. This report describes the case of a 65-year-old woman who presented acutely unwell 6 days after being bitten on the hand by a dog. She suffered consequences of overwhelming sepsis, disseminated intravascular coagulation and bilateral acute limb ischaemia requiring bilateral major lower limb amputations. C. canimorsus-associated sepsis is extremely rare, but early (prophylactic) antibiotic treatment after a dog or cat bite could prevent serious complications associated with this bacterium.
Introduction
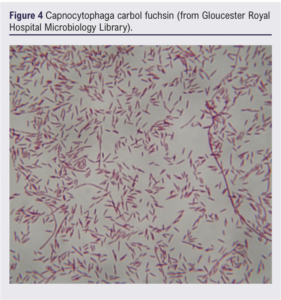
Capnocytophaga canimorsus is a Gram-negative bacterium that is part of the normal gingival flora of both dogs and cats. When humans are infected, C. canimorsus can lead to fulminant sepsis. The most common cause of human infection with C. canimorsus is from a dog or cat bite. Patients most susceptible to this infection are immunocompromised patients, those who have had a splenectomy or those with a history of heavy alcohol use.1 With doubling of dog bite-related admissions between 1998 and 2018, more patients are likely to be admitted with this bacterial infection.2 A case of fulminant C. canimorsus sepsis from a dog bite leading to disseminated intravascular coagulation (DIC) and eventual bilateral major limb amputation and ultimately death is described.
Case report
A 65-year-old woman was admitted via ambulance with confusion and reduced consciousness on a background of being bitten by a dog on the left hand 6 days prior. The patient had known small sub-threshold abdominal aortic and iliac aneurysms with a past history of two caesarian sections and a hysterectomy. She was a current smoker of 30–40 cigarettes per day, but did not have a history of alcohol excess and lived independently. On initial assessment she was hypoxic with an 8 L oxygen requirement and a Glasgow Coma Scale score of 12/15. Her initial blood results showed a platelet count of 17,000 per μL (normal range 150,000–400,000 per μL), lactate 3.3 mmol/L (normal range 0.5–2.2 mmol/L), C-reactive protein 254 mg/L (normal range <5 mg/L), a high D-dimer (greater than measurable) and a prolonged clotting time. A dog bite was noted on the left wrist which was small but deep and, although the wound showed signs of healing, there was surrounding erythema. During her initial assessment there were no issues noted with her limb perfusion. Following blood cultures, she was started on treatment for sepsis (presumed secondary to community acquired pneumonia) and transfused with platelets for thrombocytopenia, considered due to sepsis-related DIC.
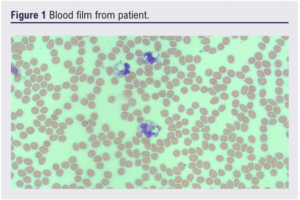
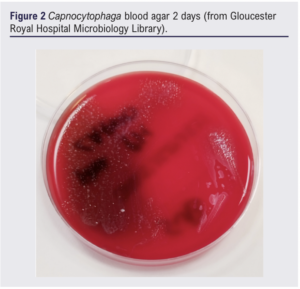
Twenty-four hours into her admission there were concerns about her feet becoming ischaemic. She was assessed overnight; no foot pulses were clinically palpable, hand-held doppler signals were absent on the left but audible over the right dorsalis pedis and posterior tibial arteries. A heparin infusion was initiated for acute limb ischaemia after discussion with a haematology consultant, due to risks of complicating her coagulopathy. An urgent CT angiogram showed no arterial flow in the lower limb crural circulation below the left mid-calf or right ankle. A vascular consultant review documented bilateral insensate feet with fixed mottling and no ankle/foot movement in the ankles, concluding that the left leg and possibly the right leg were unsalvageable. At this stage her initial blood culture result flagged positive and, although no organisms were cultured, the presence of possible intracellular organisms in the blood film were noted. Later analysis of the culture by 16S rRNA polymerase chain reaction (PCR) confirmed the organism as likely to be Capnocytophaga canimorsus (there was no growth on direct or enrichment culture) (Figure 1-4). Microbiological opinion was sought and the antibiotic treatment was escalated to meropenem, linezolid, clarithromycin and gentamicin. Due to the risk of operating given concurrent thrombocytopenia, a multidisciplinary discussion between the vascular surgeon, haematologist and intensivist was arranged. She underwent left above-knee amputation and right below-knee amputation 3 days into admission.

The patient was stepped down to the ward from the intensive care unit 3 days postoperatively and was deemed medically fit for discharge 7 days postoperatively. The patient was finally discharged to a community rehabilitation hospital nearer to her next of kin 2.5 weeks postoperatively. Unfortunately, the patient became unwell 9 days after discharge (<4 weeks postoperatively) and was re-admitted to hospital where she died on the day of admission. A post mortem found the cause of death to be (1a) pulmonary embolism and (1b) deep vein thrombosis of the right leg.
Discussion
Infection with C. canimorsus is rare. A national surveillance study in the Netherlands in 2011 showed an incidence of 0.67 cases per million per year,3 with only one of the 32 bacteraemic patients requiring bilateral lower limb amputation. A 2022 review described 207 cases of C. canimorsus infection, 22 of which included irreversible digit or limb ischaemia as a complication.5 Furthermore, a retrospective review of patients in a Helsinki ICU cohort between 2005 and 2014 found 65 patients with C. canimorsus bacteraemia,5 all of whom were in contact with dogs but only 37% had a history of a dog bite, suggesting that patients can become infected from close contact as well as a physical break in the skin. This study also found that the most commonly affected body system was coagulation (94%), with three of the 65 patients requiring lower limb amputation for tissue necrosis. A review of 484 laboratory-confirmed cases found that patients can present with severe sepsis/septic shock, gangrene of digits or extremities, meningitis and endocarditis and found a fatality rate of 26%. Major lower limb amputation secondary to acute limb ischaemia is therefore a relatively rare consequence of this infection, but septic shock and DIC have a high mortality rate.6,7
C. canimorsus is a highly virulent bacterium due to its catalase and sialidase production, as well as gliding mobility, cytotoxin production and unique lipopolysaccharide.7
On review of the patient notes, the dog bite was mentioned in the initial clerking but it was not documented as the presumed source of sepsis until the blood culture result was known. The patient had already been initiated on piperacillin-tazobactam and clarithromycin from the start of the admission, which are acceptable treatments for C. canimorsus, therefore it is difficult to know whether earlier recognition of the source of the sepsis would have improved the outcome in this case. However, had the patient been initiated on a penicillin-based antibiotic at the time of the dog bite, this might have prevented her presentation to hospital in a severely unwell state 6 days after the dog bite. Furthermore, this case highlights the importance of further analysis of blood cultures using 16S rRNA PCR when there is a clinical suspicion of C. canimorsus without growth on initial direct or enrichment culture.
Conclusion
C. canimorsus is a rare cause of sepsis in humans, occurring usually after bites or licks to the skin from dogs or cats. It has severe complications as demonstrated by this case, therefore early treatment with antibiotics for dog or cat bites as a prophylactic measure could prevent life-changing or even fatal consequences.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(3):170-172
Publication date:
May 14, 2024
Author Affiliations:
1. Department of Vascular Surgery, Gloucester Royal Hospital, Gloucester, UK
2. Department of Microbiology, Gloucester Royal Hospital, Gloucester, UK
3. Department of Haematology, Cheltenham General Hospital, Cheltenham, UK
Corresponding author:
Sachin Kulkarni
Department of Vascular Surgery, Cheltenham General Hospital, Sandford Road,
Cheltenham GL53 7AN, UK
Email: [email protected]











