ORIGINAL RESEARCH
A survey of early year consultant vascular surgeons in the UK to assess well-being, support and the availability of mentoring
Sritharan K,1 Popplewell M,2,9 Coughlin P,3 Travers H,4 Dawkins C,5 Egun A,6 Winterborn B,7 Garnham A8
Plain English Summary
Why we undertook the work: The transition from resident doctor into consultant life is recognised to be a challenging period. The aim of this survey is to understand the support available to newly appointed consultant vascular surgeons following a complication or complaint; to explore the incidence of bullying, undermining and harassment (BUH), burnout and imposter syndrome; and to understand the attitudes towards mentoring within this group.
What we did: UK consultant vascular surgeons in the first 5 years since their appointment were surveyed online over a 6-week period in 2023. The responses were collected using the survey server (SurveyMonkey) and analysed.
What we found: Almost half of all consultant vascular surgeons (45%) experienced BUH. In most cases the perpertrator(s) was a consultant colleague (63%), a colleague from a different specialty (41%) or a manager (30%). Most cases (70%) were not effectively managed by the employer and only one in three of those bullied were provided with the support they required; 39% of consultant vascular surgeons witnessed BUH in the workplace. Following a serious complication, one in four consultant vascular surgeons said that they did not receive any support, and almost one in three (31%) did not feel supported after a complaint, investigation or other regulatory process. Almost half (47%) of consultant vascular surgeons in the early stages of their career encountered a significant life event, with a third (34%) stating that they did not receive the support they required during this period. 16% reported symptoms related to post-traumatic stress disorder (PTSD) and 38% experienced burnout, with 68% feeling at risk of burnout. 55% reported imposter syndrome. Only one in three consultant vascular surgeons (34%) were working their ideal job plan, with the majority (58%) feeling unable to negotiate something better. Half of all consultant vascular surgeons (48%) surveyed had considered leaving the NHS and almost one in three (32%) regretted vascular surgery as a career choice. Only 43% had access to a mentor, with most (86%) believing that all newly appointed consultant vascular surgeons should have a mentor.
What this means: The survey reveals unacceptable levels of BUH in the workplace and failures to provide consultants with the necessary support following a complaint, complication or significant life event. The high self-reported rates of PTSD and burnout and the considerable number of consultants who have considered leaving the NHS is incredibly concerning. Unless the factors contributing to this are urgently addressed there will be a significant impact on recruiting and retaining future vascular specialists.
Abstract
Objectives: To explore the support available to newly appointed consultant vascular surgeons following a complication or complaint; to evaluate the incidence of bullying, undermining and harassment (BUH), burnout and imposter syndrome; and to understand the attitudes towards mentoring within this group.
Methods: A validated 59-question online survey was distributed by the Vascular Society of Great Britain and Ireland (VSGBI), British Society of Endovascular Therapy (BSET), and the Rouleaux Club through their national mailing lists between October and November 2023. Responses were collated using the survey server (SurveyMonkey). The results were summarised using descriptive statistics.
Results: Sixty-five consultant vascular surgeons responded, representing 54% of the target population. Eighteen (28%) were female and 47 (72%) were male. Forty (62%) had experienced a serious complication, with 25% not receiving any support. Sixteen (25%) had faced a complaint, investigation or other regulatory process, following which 31% (n=5) did not receive any support. Support when received was effective in 87% and 91% following a complication and complaint, respectively. Twenty-seven (45%) experienced BUH, the perpetrator(s) in 17 cases (63%) being a vascular surgeon colleague, in eleven cases (41%) a consultant colleague from another specialty and in eight (30%) a manager. Most cases (n=19, 70%) were not effectively managed. Support was provided in only nine cases (33%) and was effective in six (67%) of these. Twenty-three (39%) witnessed others being bullied; the subject of BUH in 83% of cases was a vascular surgeon colleague and in 52% (n=12) a trainee. Only one case (4%) was effectively managed. Twenty-seven (47%) had encountered a significant life event since becoming a consultant, with only 18 (64%) receiving support. Nine (16%) reported post-traumatic stress disorder (PTSD), with 43% describing symptoms suggestive of PTSD including: re-experiencing of events (24%), avoidance of reminders of events (21%), negative emotions related to an event (35%) and chronic hyper-arousal syndrome (14%). Twenty-one (38%) experienced burnout and 38 (68%) felt at risk of burnout. Thirty-one (55%) reported imposter syndrome. Only 19 (34%) worked their ideal job plan, with the majority (58%, n=18) not feeling in a position to negotiate a better job plan. 48% (n=27) had considered leaving the NHS and 32% (n=18) felt they had made the wrong career choice. Only 24 (43%) had a mentor. All of those who had a mentor reported the relationship to be beneficial. Forty-eight (86%) believed that all newly appointed consultants should have a mentor.
Conclusions: This survey is concerning and reveals significant distress amongst early-stage consultant vascular surgeons. Unless the areas highlighted are urgently addressed there will be a significant impact on recruitment and retention in vascular surgery in the future.
Background
The transition from resident doctor to consultant surgeon is regarded to be a period that can be extremely challenging for clinicians.1 Over the past decade the UK surgical workspace has become more testing due to a reduction in clinical experience as a result of both the European Working Time Directive and the ‘modernising medical careers’ initiative.1 These, amongst other factors, have been associated with increasing complaints and litigation, which promotes defensive management strategies and can have negative personal consequences.2 In addition, vascular surgery is a unique specialty in that more than 70% of the workload is emergent, dealing with frequent life and limb threatening emergencies in a co-morbid patient population. Adverse outcomes including patient death are therefore, unfortunately, not uncommon.
In the future there is predicted to be a critical shortage in the vascular surgery workforce. Protecting the workforce and addressing the factors which affect recruitment and retention into vascular surgery has therefore never been more important.
The aim of this survey is to explore the support available to early year consultant (EYC) vascular surgeons, to understand the incidence of bullying, undermining and harassment (BUH), burnout and imposter syndrome in this cohort and their attitudes towards mentoring.
Methods
The Checklist for Reporting of Survey Studies (CROSS)3 was used to compile this report. This online cross-sectional survey was aimed at UK consultant vascular surgeons in the first five years of independent practice. The questionnaire was designed and developed by five consultant vascular surgeons at varying stages of their career. Following multiple consensus meetings regarding important topics and questions, a survey was developed of 59 questions divided across 10 broad areas: demography; complications and complaints; bullying, undermining and harassment (BUH); sexual harassment; significant life events; PTSD; burnout; imposter syndrome; job plans and work-life balance; and the availability of mentorship (see Appendix 1 online at www.jvsgbi.com). Following inception, the survey was validated by a group of independent consultant vascular surgeons. Questions were a mixture of open and closed questions, and all closed questions were mandatory. All responses were anonymised and confidential.
There are an estimated 120 consultant vascular surgeons in their first 5 years of consultant practice. This figure is based on the numbers that were invited and/or have attended the ASPIRE 8 consultant preparation course over the last 5 years. The survey was distributed via email by the Vascular Society of Great Britain and Ireland (VSGBI), British Society of Endovascular Therapy (BSET) and the Rouleaux Club through their national mailing lists. Eligible participants within the first 5 years of their consultant practice were invited to complete the survey. The survey was administered and the responses collated by the survey server (SurveyMonkey) over a 6-week period from October 2023 to November 2023. There were no set exclusion criteria, and all responses were analysed using descriptive statistics and the appropriate tests. Incomplete responses were included in the analysis and participants were not excluded; however, the denominator is clearly adjusted in the results section to account for any missing data fields. Ethical approval was not sought due to the nature of the survey and not meeting the criteria set for research as described by the Health Research Authority (https://www.hra-decisiontools.org.uk/ research/). The principles of Good Clinical Practice were adhered to (https://www.nihr.ac.uk/career-development/clinical-research-courses-and-support/good-clinical-practice).
Results
Background
There were 65 respondents, giving an estimated response rate of 54%. Eighteen (28%) were female and 47 (72%) were male. One respondent (1.5%) was aged 30–34 years, 22 (34%) were aged 35–40 years, 30 (46%) were aged 41–44 years and 12 (19%) were aged 45–49 years. Twelve (18%) had been a consultant for one year or less, 17 (26%) for 1–2 years, 12 (18%) for 3–4 years and 15 (23%) for 4–5 years. Fifty-four (83%) held a permanent consultant post and 11 (17%) were in a locum or temporary consultant position.
Complications
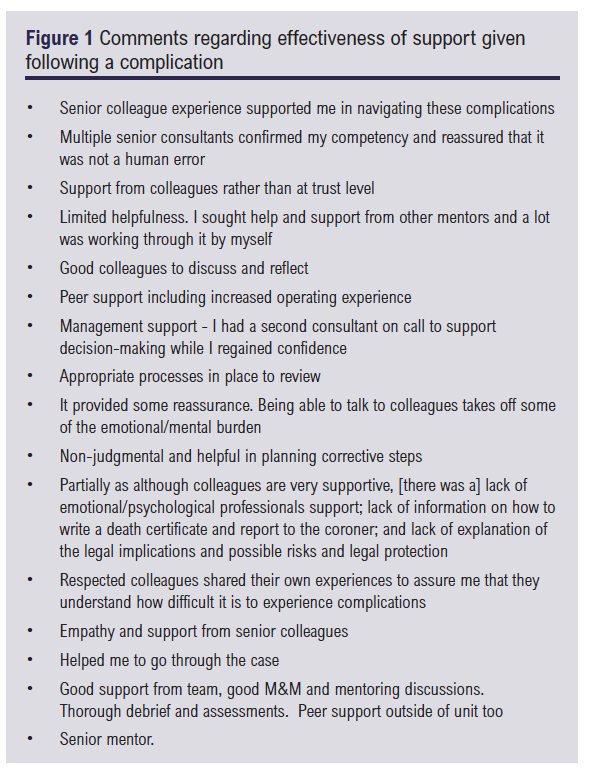
Forty respondents (62%) had experienced a serious complication and 25 (38%) had not. Serious complications were defined and included: unexpected death (83%; n=33); unexpected amputation (2.5%; n=1); stroke (10%; n=4); major amputation (15%; n=6); paraplegia (7.5%; n=3) and other (13%; n=5). Thirty respondents (75%) had received support during this period and 10 (25%) had not. Of those who received support, 86% (n=25) felt it was effective whilst 14% (n=4) did not; one person did not answer this question. The free-text comments are shown in Figure 1. In terms of the support that they would have liked to receive, 13 (43%) gave a response, of which 23% (n=3) would have liked a timely formal debrief; 69% (n=9) a timely informal debrief; 62% (n=8) for the vascular clinical director/lead to reach out; 38% (n=5) counselling; and 15% (n=2) recommendation or referral to attend a course.
Complaints
Sixteen respondents (25%) had experienced a complaint, investigation or other regulatory process since becoming a consultant, 46 (71%) had not and three (4.6%) did not provide an answer to this question. Of those who had experienced a complaint, 11 (69%) received the support they required and five (31%) did not. In most cases (91%, n=10) the support when received was effective but in one case (9.1%) it was not. Of the 31% who felt unsupported, 40% would have liked management support in responding to the complaint; 60% support from the Trust medicolegal team on how to respond to the complaint; 40% a timely both formal and informal debrief; 40% the offer of time away from work for themselves; 40% dedicated administration time to address the complaint; and 20% would have liked counselling.
Bullying, undermining and harassment (BUH)
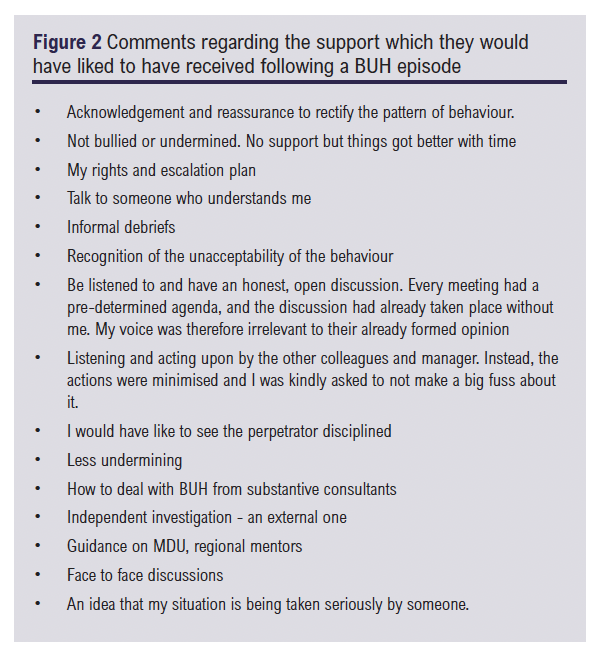
Of those that answered the question (92%), 45% (n=27) reported having experienced BUH and 55% (n=33) had not. Of those that had experienced BUH, the perpetrator(s) in 63% of cases (n=17) was a vascular surgeon colleague, in eleven cases (41%) a consultant colleague from another specialty and in eight cases (30%) it was a manager. In most cases (70%, n=19) the BUH episode(s) was not effectively managed and in 30% (n=8) it was effectively managed. Only in nine cases (33%) was support provided. This support when available was reported to be effective by 67% (n=6). The free-text comments on the support respondents would have liked to have received are given in Figure 2. Of those that answered the question (91%), 39% (n=23) reported witnessing others being bullied and 61% (n=36) did not. The subject of BUH included vascular surgeon colleagues in 83% of cases (n=19), trainees in 52% (n=12), colleagues from other specialties in 9% (n=2) and management in 4% of cases (n=1). Only in one case (4%) was the episode managed effectively by the Trust; 14 cases (61%) were not effectively managed and the outcome was unknown in eight (35%).
Sexual harassment
Of the 23 (35%) who responded to this question, two (9%) reported experiencing sexual harassment in the workplace. One was male and the other female. In half of the cases reported, the episode(s) was managed effectively. No support was given to the victim of sexual harassment in either case. A further three respondents (13%) had witnessed sexual harassment in the workplace, of which only one (33%) was managed effectively by the employer.
Significant life events
Of the 58 (89%) who responded to this question, 27 (47%) reported that they had experienced a significant life event since starting their consultant post. Of those who had a significant life event, 18 (64%) had received the support they required but 10 (36%) had not. Significant life events were not defined in this survey.
PTSD, burnout and imposter syndrome
Of the 58 (89%) who responded to this question, nine (16%) reported having experienced PTSD, 76% did not and 8.6% did not know if they had. Twenty-five (43%) reported experiencing symptoms suggestive of PTSD which included re-experiencing of events (24%), avoidance of reminders of events (21%), negative emotions related to an event (35%) and chronic hyper-arousal syndrome (14%). Of those who responded (87%, n=57), 16% (n=9) reported experiencing workplace PTSD, 77% did not and 7.0% did not know if they had.
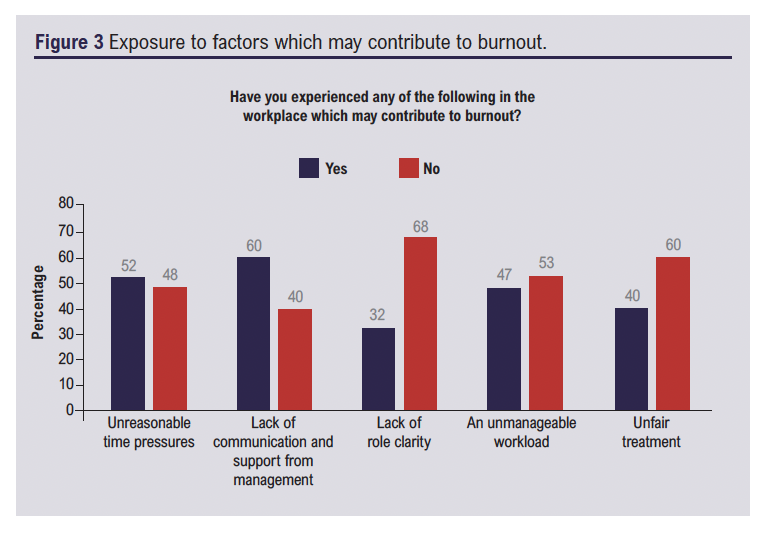
Of the 86% (n=56) that responded, 38% (n=21) had experienced burnout as a consultant, 46% (n=26) had not and 16% (9) did not know. Moreover, 68% (n=38) had experienced emotional exhaustion, 30% depersonalisation/cynicism and 50% (n=28) a decreased sense of accomplishment and professional efficacy, which are aspects suggestive of burnout. Thirty-eight (68%) felt that they were at risk of burnout, 11 (20%) did not feel they were and seven (13%) did not know. Figure 3 shows the exposure to factors which may contribute to burnout.
Of the 56 (86%) who responded, 31 (55%) had experienced imposter syndrome, 23 (41%) had not and two (4%) did not know.
Job plan and work-life balance
Of the 56 (86%) who responded to this question, only 19 (34%) reported that they were working their ideal job plan, with the majority (55%, n=31) reporting that they were not and 11% (n=6) did not know. Of those not working their ideal job plan, the majority (58%, n=18) did not feel in a position to negotiate a better job plan with only 32% (n=10) feeling that they could.
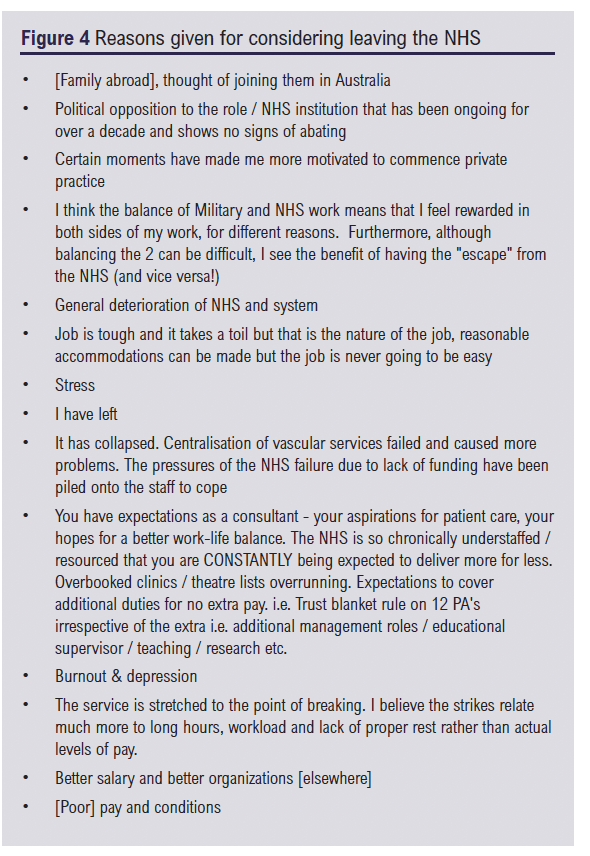
Concerningly, 48% (n=27) of consultant vascular surgeons in this study had considered leaving the NHS and 32% (n=18) felt that they had made the wrong career choice of vascular surgery since becoming a consultant vascular surgeon. The reasons given are shown in Figure 4. Only 30% (n=17) believed that they had achieved the correct work-life balance, the majority did not (55%, n=31) and 14% (n=8) did not know.
Mentoring
Of the 56 respondents (86%), only 24 (43%) had a mentor. Most mentorship relationships (79%) were informal with 79% of mentors originating from the same department and 9.5% outside of the mentee’s usual place of work. All of those who had a mentor reported that the relationship was beneficial. Nineteen (58%) of those who did not have a mentor did not know how to access one. Forty-eight (86%) believed that all newly appointed consultants should have a mentor with 3.6% not sure. The majority (73%) believed that consultant mentors should be job-planned for this commitment.
Discussion
Complications
Surgical complications form an inherent part of surgical practice. Unsurprisingly, given the co-morbid nature of vascular surgical patients and the complexity of many of the procedures performed, almost two-thirds (62%) of EYC vascular surgeons in our survey experienced a serious complication. Surgical complications can have a profound impact not only on the patient and their family but also on the surgeon, over time resulting in feelings of guilt, shame, embarrassment, anxiety, sleep disturbances, professional self-doubt, depression, burnout, PTSD and reduced job satisfaction.4-6 The surgeon then becomes the ‘second victim’.6,7 The lack of institutional support after an adverse event is recognised to be a major contributor to becoming a second victim,8 yet one in four EYC vascular surgeons in our survey reported not receiving any support following their complication. It is unknown whether a service was available but not accessed; regardless, a structured peer-support system should be provided by the employer and appropriately sign-posted.
Complaints
One in four EYC vascular surgeons in our survey were involved in a complaint, investigation or other regulatory process. Complaints in the UK NHS are common and, in one study of 10,930 UK doctors, over 6,000 had experienced a complaint with 42% of those facing a complaint reporting emotional distress as a result.2 In other studies, complaints have been linked to burnout and depression.4,8 In our survey, support was not provided to the individual in almost one in three cases (31%), even though in most cases when support was received it was regarded as being effective.
Physician burnout
Burnout is a work-related syndrome involving emotional exhaustion, depersonalisation and a sense of reduced personal accomplishment. In this survey, 38% experienced burnout as an EYC and 68% felt at risk of burnout, with 40–60% of respondents experiencing factors which are known to contribute to physician burnout such as unreasonable time pressures, lack of communication or support from management, lack of role clarity, unimaginable workloads and unfair treatment. The incidence of burnout reported in our study is similar to that seen in a large survey of US vascular surgeons conducted by the Society of Vascular Surgery in 2021.9 Physician burnout is recognised to influence quality of patient care, patient safety and patient satisfaction and, for the physician, contributes to relationship failures, alcoholism, decreased career longevity, depression and physician suicide.9,10 It is therefore imperative that this is addressed. One way of reducing the risk of burnout is to offer professional coaching. A randomised clinical trial published in 2019 found a significant reduction in emotional exhaustion and overall symptoms of burnout, as well as improvements in overall quality of life and resilience in the group who received coaching.11
Work-life balance
Worryingly, nearly half of all consultants in this survey had considered leaving the NHS with 32% feeling they had made the wrong career choice. The general deterioration of the NHS, the tough nature of the job, the lack of work-life balance, increasing workload, stress, burnout and poor pay and conditions were cited as the reasons for wanting to leave. Poor work-life balance is also implicated as a cause of UK trainees resigning from their training post in vascular surgery12 and, in a study of US trainees in vascular surgery, those in the highest quartile of burnout, as assessed using the Oldenburg Burnout Inventory, were less likely to reconsider vascular surgery as a career if given the chance to do it over again.10
Imposter syndrome
Imposter syndrome can have a significant impact on physical, psychological and professional well-being and is often linked to burnout, suicidal ideation, compromised wellness, low self-esteem and a lack of professional fulfilment.13 In our study, 55% reported experiencing imposter syndrome, and this is not surprising as the transition from trainee to consultant is often associated with increased responsibilities and stress. In one study of young consultants and resident doctors in neurosurgery, level of education, female sex and academic achievements were identified as factors predictive of developing imposter syndrome14 and, when comparing junior and senior consultants, junior faculty reported more anxiety and self-doubt compared with their senior counterparts.15
BUH
BUH has been put under the spotlight over the past few years. Despite this, 45% experienced BUH in this survey with the perpetrator in most cases being a consultant vascular surgeon colleague, a consultant colleague from another specialty and/or a manager. The incidence of bullying experienced in our cohort is similar to other studies16-18 and suggests that little has changed over the past few years. Disappointingly, most episodes of BUH were not effectively managed by the employer and only a minority of those experiencing BUH felt supported. More needs to be done to address BUH in vascular surgery, with clearer lines of accountability and safe spaces created for victims.
Only 9% reported being the subject of sexual harassment in our survey, which is far below the 63% reported by a recent study looking at the incidence of sexual harassment in the UK surgical workforce.19 Of note, only 35% of our survey participants completed this question and therefore the actual figure is likely to be much higher.
Mentoring
Those who had a mentor in our survey found it extremely useful and most respondents felt that all newly appointed consultants should have a mentor. Moreover, it has been shown that vascular surgical resident doctors who have a self-identified mentor have lower burnout scores.10 It could reasonably be assumed that this advantage would also be conferred to EYC surgeons.
Limitations and generalisability
Although the message of our survey is powerful and concerning, there are obvious limitations that must be recognised. First, the viewpoints of the participants are only representative of around half of the target population. It is possible that those who did not complete the survey had not experienced the problems described in our cohort; this would represent selection bias. However, the converse may also be true. Second, this survey was cross-sectional and can only represent the views and opinions of those participants at the specific time the survey was conducted. In addition, some of the survey component responses were lower than others, particularly in segments related to more personal and sensitive issues, suggesting that, even though anonymised, participants were reluctant to answer questions relating to their home or personal life and therefore these responses may be under or overestimated. Thirdly, the surveyed population practised vascular surgery in the UK and Ireland with the proportion of male and female respondents (72% and 28%, respectively) similar to those reported in the recent VSGBI Provision of Vascular Services for People with Vascular Diseases 2024 report.20 The data are therefore likely to be generalisable to other EYC vascular surgeons in the UK, but not necessarily similar cohorts in other countries or healthcare systems. Finally, validated questionnaires or tools were not used to assess burnout, imposter syndrome and PTSD. The incidences of burnout, imposter syndrome and PTSD reported were instead established on the perception by the respondents that they suffered these conditions based on the descriptors provided in the questionnaire. The true incidence of these conditions may therefore be lower than reported in this survey, although they are in line with other studies where validated tools were used.
Conclusion
This survey is concerning and reveals significant distress amongst EYC vascular surgeons. Unless the areas highlighted are urgently addressed, there will be a significant impact on future recruitment and retention in vascular surgery.

Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;4(3):124-130
Publication date:
May 29, 2025
Author Affiliations:
1. Consultant Vascular Surgeon, Department of Vascular Surgery, York & Scarborough Teaching Hospitals NHS Trust, York, UK
2. Consultant Vascular Surgeon, Department of Vascular Surgery, Black Country Vascular Network, Dudley, UK
3. Consultant Vascular Surgeon, Department of Vascular Surgery, Leeds General Hospital, Leeds, UK
4. Consultant Vascular Surgeon, Department of Vascular Surgery, Royal Devon University Healthcare NHS Foundation Trust, UK
5. Consultant Vascular Surgeon, Department of Vascular Surgery, Newcastle upon Tyne Hospitals NHS Foundation Trust, UK
6. Department of Vascular Surgery, Lancashire Teaching Hospital NHS Foundation Trust, Preston, UK & Chairperson Workforce Committee, VSGBI
7. Vascular Surgeon & Certified Coach and Trainer, Becs Winterborn Coaching
8. Royal Wolverhampton Hospitals NHS Trust, Wolverhampton, UK
9. Department of Applied Health Sciences, University of Birmingham, UK.
Corresponding author:
Kaji Sritharan Consultant Vascular Surgeon, Department of Vascular Surgery, York & Scarborough Teaching Hospitals NHS Trust, York, UK
Email: [email protected]











