ORIGINAL RESEARCH
Current practice in ultrasound grading of carotid artery stenosis in the UK and Ireland
Trochowski S,1 Akhtar A,1 Bond K,1 Corby A,1 Hiscocks C,1 Howard D,2 Potter R,1 Rothwell P,2 Waldegrave E,1 Webb A,2,3 Llwyd O1,2
Plain English Summary
Why we undertook the work: Ultrasound uses sound waves to create an image from inside the body. It is commonly used to assess the blood vessels in the neck. This can determine the speed of blood flowing through the vessel and if there is any disease and a significant narrowing within the blood vessel. The speed of the blood within a diseased vessel can help classify and determine the amount of disease within the blood vessel. Twenty years ago (early 2000s) it was reported that vascular centres used different ultrasound practices to classify disease within blood vessels. Guidance on how to classify disease within blood vessels of the neck were then published in the UK and Ireland in 2009 to help standardise practice between vascular centres in different hospitals.
What we did: This audit determined whether vascular centres now follow the guidance that was set out 15 years ago or whether variation still exists. An online questionnaire form was sent out to all the hospital trusts in the UK and Ireland that perform surgery on blood vessels in the neck. The form asked how they use ultrasound to classify the amount of disease in blood vessels in the neck.
What we found: The form was answered by 46/80 (58%) vascular centres in the UK and Ireland. 70% of respondents reported using the 2009 UK recommendations, while 22% reported using some. To classify moderate and severe disease many centres now use the same speed of blood flow, with some practices being used by as many as 81% (for moderate disease) and 90% (for severe disease) of centres. However, this audit identified that there was still variation between centres in other practices that classify severe disease, particularly in practices that were not covered by the 2009 recommendations. The audit also showed that fewer centres have the time and resources to perform their own internal audits.
What this means: The 2009 recommendations have helped to standardise the practices and the speed of blood flow that is used to classify moderate and severe disease within blood vessels of the neck. However, vascular centres do vary in how they apply these recommendations. There remains variation in practices used to classify severe disease, along with inconsistent practices on internal audits.
Abstract
Introduction: Ultrasound is usually the first-line imaging modality in the UK and Ireland for evaluating the severity of carotid artery disease. The last UK and Ireland audit on grading of internal carotid artery (ICA) stenosis with ultrasound was reported in 2006 whilst UK recommendations were published in 2009. This audit aims to summarise current practices.
Methods: Seventy-two UK hospital trusts and eight within Ireland that perform carotid surgery were identified. One vascular unit from each trust (n=80) was invited to complete an online questionnaire based on their current carotid ultrasound assessments including velocity thresholds (peak systolic velocity (PSV); end diastolic velocity (EDV)) and PSV ratios (PSV in the ICA:PSV in the common carotid artery (CCA)) used to grade a stenosis, the use of St Mary’s ratio (PSV in the ICA:EDV in the CCA) and the criteria prioritised to grade a stenosis.
Results: The questionnaire was answered by 58% (46/80) of vascular units. 70% of respondents reported using the 2009 UK recommendations, with 22% reported using a subset. To grade moderate disease (>50% stenosis), 81% use a PSV of >125 cm.s-1, only 36% use EDV and 71% use a velocity ratio of >2.0–4.0. To grade severe disease (>70% stenosis), 90% use a PSV of >230 cm.s-1, 43% use EDV and 86% use a velocity ratio of >4.0. Whilst the majority (78%) of units use the St Mary’s ratio to grade in deciles, there was more variation in the number of PSV and EDV thresholds used by different centres to grade severe stenosis. There was a combined total of 13 distinct (PSV, EDV and ratios) thresholds being used to grade >80% stenosis. The criteria prioritised to grade a stenosis and how near occlusion was defined on duplex imaging was variable, and there were inconsistent practices on internal audits and quality assurance.
Conclusion: The 2009 recommendations have standardised key practices in grading moderate and severe disease with PSV, velocity ratios and in the use of the St Mary’s ratio to grade in deciles. However, vascular units vary in the application of these recommendations and the use of indices not included in the guidelines.
Introduction
The degree and severity of a stenosis near the carotid bifurcation and internal carotid artery (ICA) will determine the risk/benefit relationship for a patient undergoing carotid endarterectomy surgery.1 The diagnostic accuracy of duplex ultrasound in grading ICA stenoses is comparable to computerised tomographic angiography (CTA) and magnetic resonance angiography (MRA), and it remains an instrumental diagnostic tool for identifying and grading the severity of carotid artery disease.2,3 By exploiting the exponential relationship that exists between an increase in blood velocity and a narrowed lumen,4 velocity thresholds and protocols have been published to promote consistency in how ultrasound can be used and interpreted to grade the severity of carotid disease.5-7 However, the specific velocity thresholds and the choice of parameters that are used to estimate the narrowing can still vary considerably between vascular units. A recent study in the USA reported that, due to the differences that exist between vascular units, twice as many patients would be diagnosed with a moderate (>50%) stenosis if they had been assessed at a different unit.8
The vascular units in the UK and Ireland that were audited in 19999 and in 200610 also demonstrated differences in the duplex parameters and velocity thresholds that were used to grade a carotid artery stenosis. In 2009 this prompted a working group for the Vascular Society of Great Britain and Ireland to release recommendations for reporting carotid ultrasound investigations.6 These recommendations reiterated an earlier consensus by the Society of Radiologists in Ultrasound (SRU) in how to grade moderate (>50%) and severe (>70%) disease.5 The UK recommendations also promoted the use of the St Mary’s ratio criteria to grade in deciles >50%11 and the use of a criterion to grade >90% stenosis12 that is not string flow or near occlusion. More recently, these recommendations were highlighted by the European Society for Vascular Surgery guidelines.2,13 Thus, the objectives of this audit were to describe the current clinical practices for grading carotid artery disease within the UK and Ireland and to determine whether vascular units follow the UK working group’s recommendations6 that were set out 15 years ago.
Methods
To evaluate the current ultrasound criteria that are used to grade carotid artery stenosis, an audit of vascular units in each of the UK and Ireland hospital trusts was conducted between February and July 2023. One vascular unit from each of the NHS trusts (n=72) in the UK (identified by their listing on the National Vascular Register) and Ireland (n=8) that perform carotid surgery were invited to take part (total n=80). Data were collected using an online questionnaire (Online Surveys, Jisc, UK). Vascular units were invited via email to complete the questionnaire. Units that had senior members and contact details registered on a database by the College and Society for Clinical Vascular Science of Great Britain and Ireland (CSVS; previously known as the Society for Vascular Technology of Great Britain and Ireland, SVT) were approached to answer the questionnaire. Suitable participants from vascular units that were not registered on the CSVS database were contacted by telephone and/or email to take part.
Questionnaire development
The questionnaire was devised by the Oxford University Hospitals (OUH)’s Carotid Audit team that includes clinical vascular scientists, vascular surgeons and neurologists who specialise in stroke. A panel discussion was used to accept, adapt or reject questions to be asked, with the aim of keeping the questions brief, easy to answer and to a limited number. The strengths of the questionnaire, according to the Survey Checklist Manifesto,14 were that it avoided statements, constructed specific response options with options to specify and expand on key questions, avoided multi-barrelled items, asked each question at a time, used positive language and avoided reverse-scored items. Having an appropriate number of response options was not possible in some of the questions asked, particularly in Q4 where the requirement was to enter several velocity thresholds and ratios. It was decided that a question with many specific response options with the possibility to expand was a better approach than to limit the number of response options. The Online Surveys (Jisc, UK) platform added a professional visual layout, consistency and clarity to each of the questions.
The short questionnaire included 14 questions that were based on current clinical practices when performing carotid ultrasound assessment (see Appendix online at www.jvsgbi.com) and previous audits in the field.8-10 This included completing a table (early in the survey, Q4) on the velocity thresholds (peak systolic velocity (PSV); end diastolic velocity (EDV)) and PSV ratios that are used to grade each stenosis category, whether their criteria used the St Mary’s ratio (PSV at the ICA:EDV at the common carotid artery (CCA)), the criteria used, the criteria prioritised to grade a stenosis, the criteria used to define string sign or near occlusion and whether quality assurance (QA) or an internal audit had been completed in the unit recently. Each question had a section for the participant to add any other information that was deemed relevant, including any use of their own criteria that had been developed within the unit and that was not listed within the questionnaire. Only one question, based on the location of the vascular unit, was made compulsory to help identify any duplicate answers that would come from the same vascular unit or trust. The primary objective was to determine for each stenosis category the number of distinct thresholds used for each velocity criteria (PSV, EDV, PSV ratio) and their distribution. The second objective for this audit was to determine whether units were using the 2009 UK recommendations or their own criteria, and the methods used to determine a unit’s own criteria (and three questions about pre-surgery decisions from the questionnaire have been omitted from further analysis).
Data and statistical analysis
Data from each questionnaire were extracted and managed in Excel (Microsoft) before being analysed using R (RStudio) and Prism (GraphPad). Data with multiple choice answers were categorised and reported accordingly. Any information that was text based was reviewed, interpreted and defined by a senior vascular scientist and a clinical vascular scientist who had previous experience in qualitative research.
Results
Population
Forty-six vascular units, each from separate healthcare trusts, answered the survey, corresponding to 58% of the trusts that perform carotid surgery within the UK and Ireland (n=35, 4, 4 and 3 for England, Scotland, Wales and Ireland, respectively), with only one duplicate response that was excluded. Most of the questionnaires were answered by responders affiliated with the CSVS (93%), with 11% also affiliated with the British Medical Ultrasound Society (BMUS) and 2% only affiliated with BMUS or the Society of Radiographers (SOR). When reporting whether they followed the Joint Recommendations for Reporting Carotid Ultrasound Investigations in the United Kingdom,6 70% said yes, 22% said some, 7% were unsure and 2% reported ‘other’.
Velocity criteria
Due to an incomplete response, four units were excluded from further data analysis on the velocity criteria and data are presented for the other 42 separate units (91% of the respondents). Table 1 shows the number of different PSV, EDV and PSV ratio thresholds used to grade each stenosis category. For PSV ratios, the highest number (n=5) of distinct thresholds was for grading >50% stenosis. Together with the PSV and EDV thresholds, the highest total number of distinct thresholds (n=13) was for >80% decile. Interestingly, all units reported using a PSV for grading >70% stenosis whereas, in comparison, PSV ratio and EDV were only used by 90% and 43% of the vascular centres, respectively.
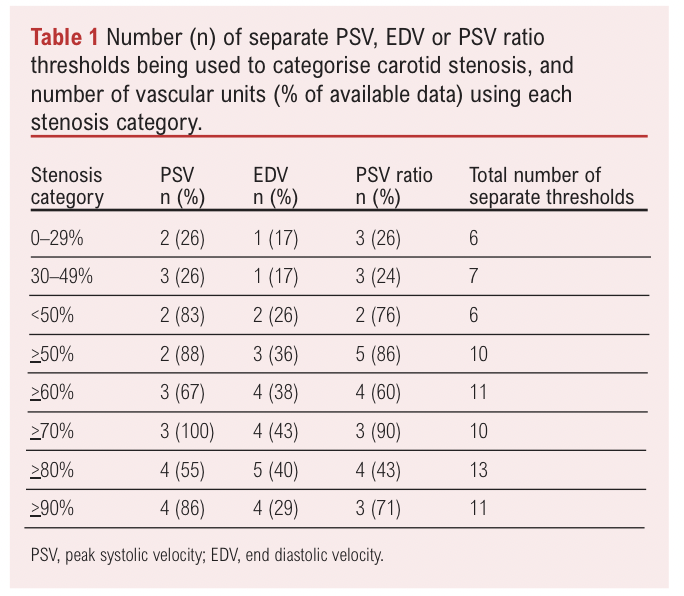
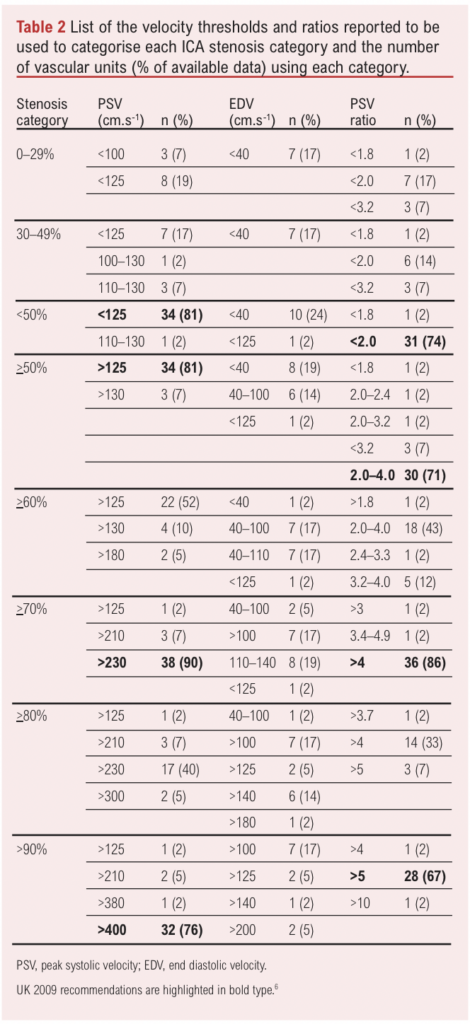
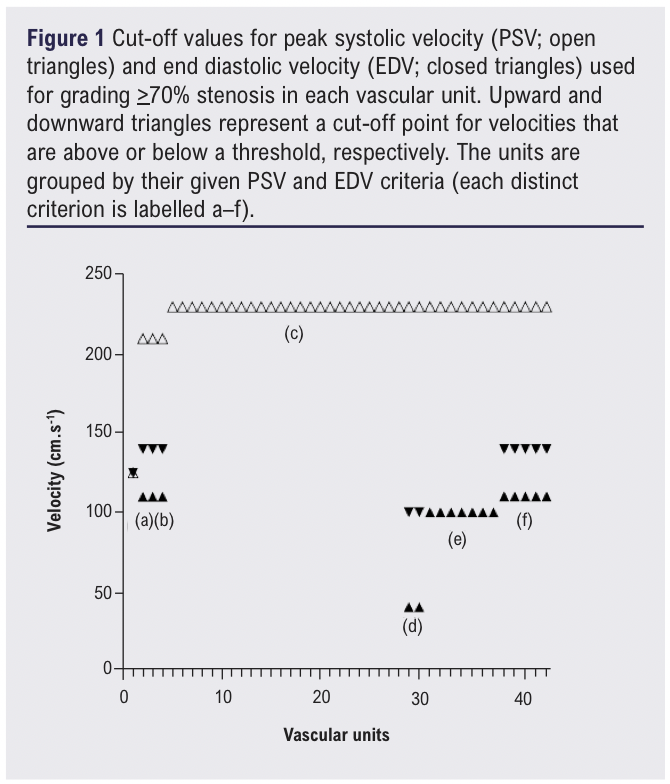
Table 2 shows each distinct threshold used for grading a carotid stenosis and the number (%) of units using each threshold. The majority of units use the PSV and PSV ratios recommended in the UK guidelines (highlighted in bold in Table 2). For grading moderate disease (>50% stenosis), a PSV of >125 cm.s-1 and PSV ratio of 2–4 is used by 81% and 71% units, respectively. For grading severe disease (>70% stenosis), a PSV of >230 cm.s-1 and PSV ratio of >4 is used by 90% and 86% of units, respectively, but fewer units use the recommended criteria for grading >90% ICA stenosis with a PSV >400 cm.s-1 and PSV ratio >5 (76% and 67%, respectively). Some vascular units did report the use of EDV, particularly when grading a severe stenosis, with 43%, 40% and 29% reporting the use of EDV criteria to grade >70%, >80% and >90% stenosis, respectively. Figure 1 shows each PSV and EDV threshold used by every vascular unit to grade >70% stenosis and highlights that, by using these two parameters, there are five different criteria (labelled a–f) currently in use to grade a severe stenosis.
Criteria prioritised to grade a stenosis
All vascular units reported on which parameters are used when grading a carotid stenosis. A mean±SD of 5±2 separate ultrasound parameters are used by each unit to grade a carotid stenosis, with the most common criteria being PSV (used by 94% of the units) and PSV ratio (83%), followed by use of St Mary’s ratio (78%) and B-mode assessment (74%). EDV is used by 46% of the units, North American Symptomatic Carotid Endarterectomy Trial (NASCET) calliper and European Carotid Surgery Trial (ECST) calliper measurements by 44% and 17% of units, respectively. Other criteria commented on were the use of colour Doppler assessment by 11%, one (2%) reported using their own PSV criteria and 11% highlighted the use of ECST calliper measurements only in the presence of a large carotid bulb.
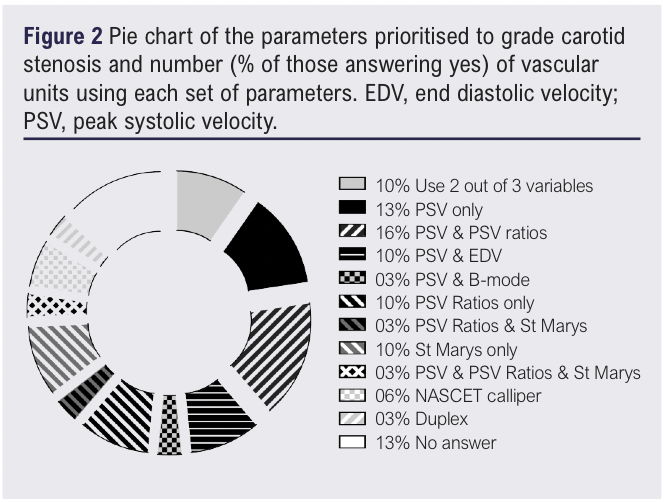
When asked which parameters were prioritised when grading a carotid stenosis, 65% of vascular units reported that they did prioritise, 30% reported that they did not prioritise and 4% did not know. A list of the criteria prioritised and number (% of those reporting yes) of responses for each set of criteria is shown in Figure 2. Overall, the most popular criteria included the use of PSV (28%) with or without another parameter, followed by PSV ratio (20%), St Mary’s ratio (11%), B-mode (2%), EDV (7%) and NASCET calliper (4%).
Near occlusion
Forty-five units (98%) answered the question on how they defined ‘near occlusion/string sign based on duplex imaging’. To define string sign, the appearance of a narrow channel of flow characterised using colour Doppler (89%) and velocity measurement (76%) was the most common answer. 70% of units highlighted the importance of using low velocities, but only a small proportion of units mentioned a specific velocity criterion of <20 cm.s-1 (4%) and >400 cm.s-1 (2%). The use of B-mode (30%) and waveform characteristics (22%) was also reported, as was the collapse of the distal vessel (7%), power Doppler (9%), EDV (4%) and B-flow/microvascular imaging (4%).
Internal audits and quality assurance
All units answered whether they performed an internal audit or QA in relation to the use of ultrasound to grade a carotid stenosis; 22% of units reported that they had, 37% reported they had not with 26% reporting that they ‘would like to but no time’ and ‘other’ was reported by 15%. Some (39%) expanded on how recent the last review occurred. One unit had just completed an audit, one reported performing regularly, three within the last year, three within the last three years and two within the last 10 years. Some of the responses highlighted the ongoing comparisons during MDTs of duplex with other imaging modalities (eg, CTA) or following surgery, particularly if there were discrepancies, or regularly sampling either 5% of all the scans or comparing assessments that have been repeated before surgery. Forty-five units (98%) answered the question on whether there was intention to perform an internal audit in the future and when this would take place, whereas 53% reported not applicable, and 11%, 13% and 9% reported that it will be performed in 6 months, 12 months or 2 years’ time, respectively, and 13% reported ‘other’. Two units expanded on their answers and reported that it would occur when staffing levels are sufficient.
Discussion
This audit confirms that most vascular units within the UK and Ireland now use the same PSV and PSV ratios for grading moderate and severe carotid artery disease and that the 2009 UK recommendations have been well received. However, some disparity remains between vascular units, with more variation in grading severe rather than moderate disease, some units also use EDV to categorise a stenosis, a lack of consensus in the parameters that should be prioritised when grading a stenosis or in how a near occlusion and string flow is defined on ultrasound, and inconsistent practice on internal audits and QA.
When comparing the results from this audit to the two previous audits conducted in the UK and Ireland,9,10 there is much less variability apparent in current practice. The most popular criterion used in 2000 to categorise a carotid stenosis was the ratio of the PSV to the EDV in the ICA (used by 36% of the units), with many cut-off values reported to have been devised in-house. Only one vascular unit reported using an in-house criterion within this audit. Other vascular units reported PSV, EDV and PSV ratios established within the literature, such as those recommended by the SRU in 20035 and later supported by the Vascular Society of Great Britain and Ireland in the UK in 2009.6 The recommendations in the UK were prompted by the 2006 UK and Ireland audit10 which highlighted that a variety of PSV and EDV criteria were being used to categorise severe stenosis of >70%. This audit confirms that these published guidelines and recommendations have reduced the variability between vascular units but, specifically, only in the PSV and PSV ratio criteria being used to grade a >50% stenosis (81% use >125 cm.s-1 and 71% use a ratio of 2–4) and a >70% stenosis (90% use >230 cm.s-1 and 86% use a ratio of >4).
However, there remains considerable variability in the practices and criteria not reported within current UK recommendations. Although the UK recommendations report that the EDV within the ICA should be recorded, it does not expand on an EDV cut-off value that can be used to grade a stenosis. This contrasts with the SRU 2003 guidelines which recommend using EDV values in the ICA of 40–100 cm.s-1 to grade 50–69% stenosis and >100 cm.s-1 to grade >70% stenosis. The CSVS (to which 93% of responders to this audit were affiliated) guidelines on performing carotid ultrasound reports on the usefulness of using EDV values suggested by the SRU 2003 guidelines to grade a stenosis.15 In this audit 46% of the vascular units reported using ICA EDV cut-off values, with up to 17% specifically using values that are recommended by SRU guidelines (see Figure 1e). Thus, with some vascular units also using EDV to grade >70%, >80% and >90% stenosis, vascular centres have opted to use a range of previously published thresholds, adding to the variability in practices. Of note, Columbo et al8 recently described considerable variation in the thresholds used for carotid stenosis grading using ultrasound between centres in the USA and concluded that this variation could change the diagnosis of patients, depending on where the carotid ultrasound was performed. Their audit of 338 vascular testing centres described a total of 29 and 37 different PSV, EDV and PSV ratio thresholds for grading >50% and >70% stenosis, respectively. There is a similar amount of variability present in the UK and Ireland, with a total of 10 and 13 different separate cut-off values used among just 42 centres.
Although 65% of vascular units said they prioritised a specific criterion to grade a stenosis, which criteria they used varied, indicating there is uncertainty as to which are the best criteria to use. Only 10% reported using the UK recommendations (an agreement between two out of three parameters is used to grade a stenosis). Prioritising the use of a single velocity measurement parameter such as the PSV with visual appearance (B-mode and colour Doppler) is supported by SRU 2003.5 More recent guidelines by the Neurosonology Research Group of the World Federation of Neurology7 highlight the variability that can arise between measurements from using only the PSV (due to technological limitations and complexity of the circulation) and the benefit of using a multi-parametric approach. Although uptake of some of this guidance was apparent with half of the vascular units using PSV in combination with other parameters, there was no consensus on which group of parameters is best to grade a stenosis.
The St Mary’s ratio (comparing PSV in the ICA to the EDV in the CCA) is recommended in the UK to grade in deciles >50% and is currently being used by 78% of vascular units. However, the accuracy of ultrasound to stratify disease and separate deciles within moderate (>50% vs >60%) or severe disease (>70% vs >80%) has been disputed and discouraged in current guidelines.5,7 What was apparent within this audit was that some vascular units use EDV to grade >60% and >80% stenosis, as the PSV and PSV ratios in their respective deciles (50% and 70%) are the same. There is now growing evidence that asymptomatic patients have a higher risk of stroke when categorised with an 80–99% stenosis compared with a 50–79% stenosis,16 possibly warranting consideration for vascular intervention. Thus, there is clinical need to stratify significant disease outside the current dichotomised norm of >50% and >70% stenosis.
Only 17% of the vascular units reported using the ECST calliper method to measure the degree of stenosis, and this was in relation to the recommendation of it being an additional measurement in the presence of a large carotid bulb. Although Walker and Naylor10 reported that 43% of respondents indicated that they did not know which criteria they were using, in those that did report using the ECST method, velocity cut-offs were generally around a PSV of 180 cm.s-1 or lower. These velocities were reported by one vascular unit in this audit (Figure 1) who did not expand on whether this was due to ECST-based criteria. However, Figure 1 also confirms the shift to grading the stenosis using NASCET-based ratios and velocity criteria, which could be one reason why the data for PSV had less variability. Of note, by only comparing PSV and EDV to categorise >70% stenosis (Figure 1), there were 25 different criteria being used in 2006. This number has now decreased substantially to six (labelled a–f in Figure 1). However, although 90% of the vascular units now use the same PSV of >230 cm.s-1 to grade >70% stenosis, 57% follow the UK guidelines (Figure 1c) with the other 43% reporting a mixture of EDV and PSV to grade this category. Additionally, there was a mixed response to defining near occlusion or string sign based on duplex imaging. The UK recommendations6 describe near occlusion with a PSV that is high, low-string flow with a variable PSV ratio and St Mary’s ratio. Although the use of colour Doppler and velocities were common answers to the question in this audit, there was no clear definition on the criteria and parameters to stratify this clinically important disposition.
Finally, only 24% of centres reported that they have performed an internal audit or a QA. In comparison, the audit in 2000 by Perkins et al9 described 51% of the vascular units validating their duplex criteria against angiography, with 36% using criteria validated in the literature or by another vascular unit. In our study, few vascular units clearly described the practice of comparing the ultrasound data to other imaging modalities, with many describing lack of time and resources as a key factor in not conducting any audit. Although there is renewed guidance on performing QA and audits on staff performance17 and equipment,18 it is apparent that there is now more of an emphasis on using criteria published in the literature without performing additional internal audits to corroborate the suitability of the criteria to their own practices or equipment, which could influence the grading of the severity of the disease.19-21 The 2006 Health Technology Assessment in using imaging modalities to assess carotid stenosis in the UK22 reported the cost effectiveness of ultrasound and its comparability to other imaging modalities in accurately grading carotid artery disease. However, it was also reported that ultrasound imaging should be carefully audited when used routinely in clinical practice to maintain accuracy. To increase consensus and lessen the variability between centres, it could be recommended that a central audit office is formed to regularly analyse, monitor and compare the diagnostic accuracy of each vascular centre.22
Limitations
There was a good overall response rate to the questionnaire (58%), and although the response was a little lower than the two previous audits in the UK, there was a greater emphasis within this audit on gaining a response from each separate health board trust that performs carotid endarterectomy rather than gaining many vascular units or vascular scientists to complete the questionnaire. It was also presumed that separate tertiary vascular units would follow the same protocol and criteria and, to evade duplicate answers, it was decided that a response from one vascular unit from each trust would suffice. There was also emphasis on gaining a broader response in the clinical practice of the vascular units, which included a combination of velocity cut-off values for each stenosis category, parameters used, how near occlusion is defined and on whether internal audits are performed without jeopardising an incomplete response. Using a forced choice format would have added a substantial amount of time to answering the questionnaire but would have ensured that each question was answered and highlight any questions unanswered.14 A check-all-that-apply format could also have resulted in respondents picking more items towards the top of the list.14 However, this was not apparent in the data collected. Despite only making one question compulsory (location of the vascular unit), there was an excellent response to each of the questions, excluding the four incomplete answers received for the velocity cut-off criteria. Some questions could have been more specific about the vascular unit’s practice; however, it was decided that giving the option to further expand on all the questions was better practice than having a substantial number of incomplete answers. Finally, the method of promoting and dispersing the questionnaire, with the help of the CSVS database, could be interpreted as being reflected in the affiliation of each respondent to the society (93%), but this could also reflect the association and impact of the CSVS within vascular units in the UK and Ireland.
Conclusion
This audit demonstrates that previous guidelines and recommendations have had an impact on clinical practices in grading carotid artery disease within the UK and Ireland. The 2009 UK recommendations have standardised key practices when grading moderate and severe disease with PSV, velocity ratios and in the use of the St Mary’s ratio to grade in deciles. But vascular units do vary their practices in areas of carotid ultrasound that are not reported in the current recommendations, such as the use of EDV, prioritising parameters to use when grading a stenosis and in how near occlusion is defined. Together with a lack of emphasis by vascular units to perform internal audits and QA, there is room for further guidance in these important practices when performing carotid ultrasound.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;4(1):41-47
Publication date:
November 25, 2024
Author Affiliations:
1. Jackie Walton Vascular Studies Unit, John Radcliffe Hospital, Oxford University Hospitals, Oxford, UK
2. Wolfson Centre for Prevention of Stroke and Dementia, Department of Clinical Neurosciences, University of Oxford, Oxford, UK
3. Department of Brain Sciences, Imperial College London, London, UK
Corresponding author:
Osian Llwyd
Clinical Vascular Scientist,
Jackie Walton Vascular Studies Unit, John Radcliffe Hospital, Oxford University Hospitals,
Oxford, UK.
Email: [email protected]











