ORIGINAL RESEARCH
Defining priorities in vascular access research
De Siqueira JR,1 Fielding CA,2 Pettigrew GJ,3 Robson MG,4 Rogers SK,5 Steiner K,6 Withers W,7 Long J,8 Gronlund T,9 Chetter I,8 Smith GE8 on behalf of the VSGBI Vascular Access Special Interest Group/James Lind Alliance Priority Setting Partnership
Plain English Summary
Why we undertook the work: People with kidney failure need to be connected to dialysis machines by lines which provide access to high volumes of blood; this is called vascular access and can be delivered through direct connections to the main veins in the body or by surgically creating a high pressure system (arteriovenous fistula and graft) close to the surface of the skin. Despite dialysis becoming more common, there are not many large-scale studies which guide clinicians on how to manage patients who live with vascular access. We wanted to establish what the key priorities for research were, according to patients, carers and access clinicians.
What we did: We conducted four online surveys targeting doctors, nurses, patients and carers and held a workshop to define the top10 priorities in vascular access research.
What we found: There was a high response rate to the survey. The patients’ and clinicians’ top 10 priority list included questions regarding optimising access function and preventing complications, and ensuring everybody is well educated in access matters.
What this means: This top 10 list will hopefully serve as a basis to direct future research. Researchers may wish to consider whether their research proposals fit with these agreed priorities. Research funding bodies may also use this list to decide whether future research is justified and eligible for funding.
Abstract
Introduction: There is increasing need for renal replacement therapy associated with the aging population and dramatic increases in diabetes prevalence. Despite an increasing clinical vascular access workload, there are significant unanswered research questions and a paucity of high quality trials to guide clinical practice. To address where future research in vascular access should be directed, we conducted a Priority Setting Partnership involving multiple disciplines, specialties, patients and carers.
Methods: In collaboration with the James Lind Alliance, four rounds of surveys were circulated to identify and score professional and patient priorities in vascular access research. Finally, in a consensus workshop attended by patients and professionals, priorities were discussed and a ranked top 10 list was produced using a nominal group technique.
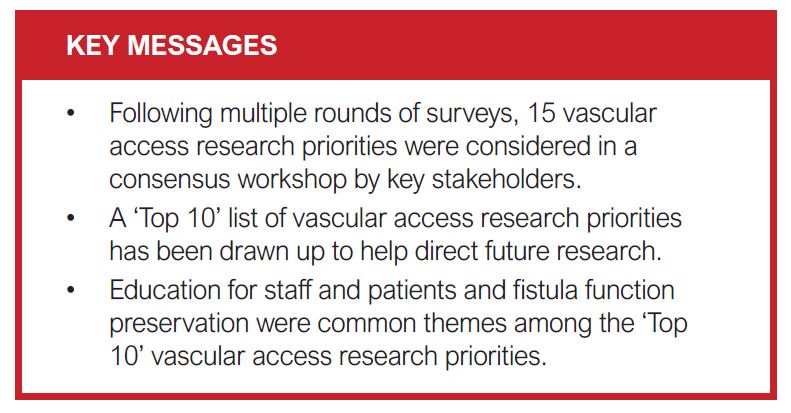
Results: A total of 1,813 research priorities were submitted within all areas of vascular surgery. Following removal of duplicates, consolidation and categorisation, 15 patient and professional priorities in vascular access research were taken forward to the consensus workshop. The workshop produced a ranked top 10 list of vascular access research priorities relating to: optimising access function, preventing access complications and education of patients and healthcare staff.
Conclusions: These research priorities should help to direct and contextualise future research in vascular access.
Introduction
The global prevalence of renal failure is rising, driven predominantly by diabetes.1 In the UK, 37.8% of the 68,111 patients on renal replacement therapy receive haemodialysis.2 Accordingly, there is a sustained increase in the need for vascular access and vascular access interventions. The Standardized Outcomes in Nephrology – Hemodialysis (SONG-HD) initiative is an international consensus process involving >1,300 patients, caregivers and health professionals from >70 countries; vascular access was identified as one of four areas in haemodialysis care considered critical to all stakeholders.3,4 Despite this, vascular access for haemodialysis remains a ‘Cinderella’ sub-specialty of vascular and transplant surgery. There are no landmark trials on the scale of those in aneurysm repair, carotid surgery, venous disease or peripheral arterial disease. Thus, clinical decision-making is based upon guidance that is not backed up by a robust evidence base and many significant questions remain in vascular access care.
Funding for vascular access research – and vascular surgery research more broadly – is lacking. There are no established large-scale funding charities for work in this field. As a consequence, funding applications must compete against many other clinical specialties in broad funding competition. Researcher-led funding applications in vascular access surgery have had low rates of success and are often developed in isolation. To combat this challenge, over the last three years the Vascular Society of Great Britain and Ireland (VSGBI) has partnered with the James Lind Alliance (JLA) in a Priority Setting Partnership (PSP). The aim of the PSP was to define the top 10 research priorities in vascular surgery through an international (UK and Ireland) prioritisation process involving patients, carers and professionals. This ‘Top 10’ would be the foundation of a clear strategy for research in vascular access over the coming years and be a demonstrable base on which to justify future proposals.5
Methods
The methodology was adapted from that used by other JLA PSPs,6 as previously reported.7
In the first stage, a national online Delphi survey was launched to members of VSGBI, the Society of Vascular Nursing (SVN), the Rouleaux Club (the UK and Ireland vascular surgery trainees society) and the Society of Vascular Technology (SVT). Members were contacted by email. Clinicians were asked to submit suggestions for what they perceived to be the key priorities in vascular surgery research through an online portal (Bristol Online Survey Tool). Respondents were free to suggest as many priorities as they wished. Duplicate and overlapping priorities were removed or consolidated by a sub-group of the PSP steering committee. Priorities were then grouped by clinical categories.
A second round of survey was launched asking prior contributors to score the importance of the rationalised and re-categorised priorities on a scale from 1 (least important) to 10 (most important). Sum scores were to be used to draw a preliminary rank of 30 priorities, as published previously.5
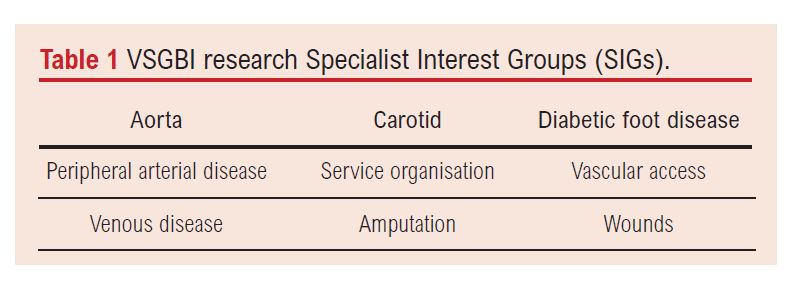
Following review of the priorities, the research committee of VSGBI and vascular patient representatives concluded that assessment of patient priorities would necessitate sub-speciality investigation. Separate Specialist Interest Groups (SIGs) (Table 1) were formed to address multiple sub-PSPs. The SIGs were to have relevant multispecialty and multidisciplinary representation. Chairs and deputy chairs were advertised nationally and appointed by the VSGBI research committee following competitive interview. Further stages in the overall PSP were coordinated centrally by the VSGBI and JLA, although each SIG took charge of its own sub-specialty PSP. The vascular access SIG at the time of the PSP was made up of a vascular surgeon, a vascular surgery trainee, a radiologist, a patient representative, a nephrologist, a dialysis nurse specialist and a vascular scientist.
 Following formation of the SIGs, a second survey was launched, this time targeting patients and carers. The survey could be completed online (Qualtrics™) or on paper and returned to the PSP coordinating centre. The survey was advertised to vascular surgery and nephrology charities and patient groups. Patients and carers were asked to state their experience of vascular surgery (access, aneurysm, etc) and submit their perceived research priorities. Patients and carers were also asked if they could be contacted to participate in further work in this process. Proposed research priorities were consolidated in the same manner as in the first survey, this time by the SIG. Priorities were re-worded by the SIG members with the assistance of the PSP coordinator for clarity and wording.
Following formation of the SIGs, a second survey was launched, this time targeting patients and carers. The survey could be completed online (Qualtrics™) or on paper and returned to the PSP coordinating centre. The survey was advertised to vascular surgery and nephrology charities and patient groups. Patients and carers were asked to state their experience of vascular surgery (access, aneurysm, etc) and submit their perceived research priorities. Patients and carers were also asked if they could be contacted to participate in further work in this process. Proposed research priorities were consolidated in the same manner as in the first survey, this time by the SIG. Priorities were re-worded by the SIG members with the assistance of the PSP coordinator for clarity and wording.
In the next step, patients and carers were canvassed again via a further survey and were asked to score the summarised priorities on a scale from 1 (least important) to 5 (most important). This resulted in the preliminary list of scored patient priorities to take forward to a consensus workshop.
The final step in the vascular access PSP process was to hold a consensus workshop which, due to the COVID-19 pandemic, was held by means of an online meeting. Six patient representatives and six healthcare professionals joined the workshop with the aim of ranking the priorities to identify a final top 10. The workshop was facilitated by two members of the JLA and led by the SIG chair. Participants were invited either through SIG contacts or drawn from survey respondents who had indicated that they were happy to be involved in future work. Full telephone technical support for accessing the online workshop was offered and a reserve ‘telephone in’ option was also made available for those without internet access. Participants were split into mixed groups of six. Participants in each group were asked to declare their top three and bottom three priorities to the group. This was followed by discussion, before agreeing a preliminary ‘Top 10’. The priority lists from each group were pooled by their geometric mean and presented as a preliminary list to the whole group of 12 for consideration. Participants were then redistributed into two new sub-groups of six and could adjust the ranking once more. The final ranking from the two sub-groups was again consolidated bygeometric mean and this was agreed as the final ranked top 10 list of research priorities for vascular access. Participants were asked to complete a feedback survey after they had participated in the workshop to evaluate its effectiveness.
Results
In total, 1,231 priorities were submitted by 481 health professionals during the first Delphi survey. These were rationalised into 83 priorities in nine clinical categories, of which two were related to vascular access. For the subsequent healthcare professional scoring survey, 323 responses were received. The full results of this survey have been published previously.5
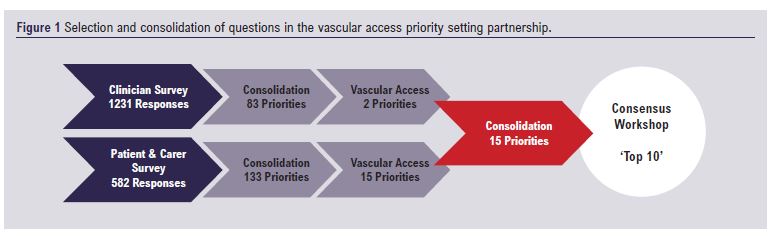
Among 373 patients and carers, 582 priorities were submitted, of which 61 related to vascular access. Consolidation and summarisation of priorities led to a list of 15 relating to vascular access. The patient and carer scoring survey received a total of 273 responses; 22 respondents chose to score vascular access priorities. These were consolidated with the two priorities from the healthcare professional survey into a final list of 15 priorities for the consensus workshop (Figure 1).
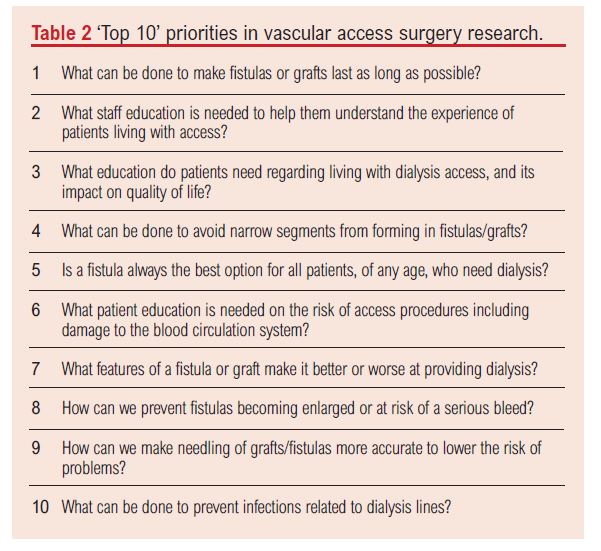
The workshop was attended by six patients, two carers, two vascular surgeons (one trainee), one vascular scientist, one nephrologist and two dialysis nurse specialists. The top 10 ranked vascular access research priorities agreed at the workshop are shown in Table 2. Patients and carers championed priorities on education, pain reduction and quality of life, whilst clinicians championed priorities relating to access longevity. Overall satisfaction with the workshop was high among participants who agreed that the final top 10 was a fair reflection of the aggregated view of the attendants.
Five research priorities did not rank sufficiently highly to be included in the top 10 priorities. Two of these related to the duties of non-medical staff: having a single nurse assigned to a patient for every needling was felt to be undeliverable and thus not worthy of research; the potential role for non-medical staff in performing central vein cannulation was received poorly by patients and carers. Although there was debate among patients regarding the utility of keeping a running fistula following successful transplantation, it was not felt to be of sufficiently high enough priority to justify its place in the top 10. Pain on needling was ranked high by some patients but dismissed by others following the use of topical agents and seen as unavoidable by healthcare professionals. Finally, reducing swelling in limbs after formation of vascular access was seen to be likely related to venous outflow problems, which overlapped with more highly ranked research priorities.
Discussion
This paper describes a process for establishing a top 10 list of priorities in vascular access research according to a broad set of stakeholders including patients, carers and the professionals responsible for their care. To do so, a modified JLA process was adopted to identify, score and rank priorities sourced from clinicians and patients. The final top 10 represents a balanced view of contrasting priorities among healthcare professionals and patients. While PSP top 10 lists are ranked, all priorities identified are important, regardless of position.
Of interest, a dialysis PSP was facilitated by the JLA in Canada in 2014.8 While none of the top 10 priorities in the Canadian process match those of the ones described here, there is notable overlap in themes, such as assessing differences in dialysis modalities or access types in different patient cohorts and enhancing patient and staff education and communication. A systematic review of priority setting in kidney disease was also undertaken in 2015.9 There was significant discrepancy in methodologies applied and little patient involvement across the studies included; however, improvements to vascular access were a recurring theme in the top priorities of these studies. While chronic kidney disease and dialysis as a whole are broader in scope than vascular access, the recurring themes add support to the potential international impact of this PSP.
Study limitations
This process has some limitations which warrant discussion. Firstly, the process was partly conducted during the COVID-19 pandemic, requiring virtual and remote working for the final workshop. Even with the technical support offered, there may be an element of selection bias towards participants who are more comfortable with online working. In the same vein, although a paper questionnaire was made freely available, the majority of survey results were received electronically, conferring the same potential bias. As the process was initially designed to address priorities in vascular surgery broadly, there was under-representation of transplant surgeons, nephrologists and vascular access nurses in the clinician survey. This was compensated for in later stages. Lastly, any survey is inherently susceptible to responder bias.10
Attempts were made to have a fair distribution of experience and geographical location among participants in the workshop. However, this had to be balanced against a ‘practical’ number of people who could participate in an open video forum and lost participants due to absence on the day. Thus, the sum of subjective experience in the workshop may not be sufficient for a fully objective prioritisation.
Finally, throughout the earlier parts of the process, engagement with patients and carers was challenging. Many respondents and participants perceive themselves as ‘dialysis’ or ‘kidney’ patients; communication from ‘the vascular society’ about ‘vascular disease’ priorities was anecdotally reported as potentially irrelevant to the targeted patients. Equally, the term ‘vascular access’ was somewhat esoteric to this cohort. Supporting information regarding the applicability of the survey to vascular access patients was communicated through relevant kidney charities to try to minimise this.
Conclusion
A ‘Top 10’ of research priorities in vascular access offers an opportunity for researchers and funders to consider future research applications in a different context and frame the perceived impact their questions and results may have on patients and care. It is hoped that this list will not only be of use to researchers in the UK and more widely, but will also help to ensure that limited research funding is targeted at the projects that are most likely to have the most impact on patients and in assisting with common day-to-day clinical decisions made by healthcare professionals. The Vascular Access SIG is now tasked with developing research projects which address the top 10 priorities through a wide collaboration with relevant organisations, multidisciplinary professionals, patients and carers.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(2):30-33
Publication date:
February 23, 2022
Author Affiliations:
1.Leeds Institute of Cardiovascular and Metabolic Medicine, University of Leeds, UK,
2.University Hospitals of Derby and Burton NHS Foundation Trust, UK
3.Department of Surgery, University of Cambridge, UK
4.School of Immunology & Microbial Sciences, King’s College London, UK
5.Division of Cardiovascular Sciences, University of Manchester, UK
6.East and North Hertfordshire NHS Trust, UK
7.Patient representative, Queen Elizabeth Hospital, UK
8.Hull University Teaching Hospitals NHS Trust, UK
9.James Lind Alliance, UK