ORIGINAL RESEARCH
Deprivation and supervised exercise for intermittent claudication
Gwilym BL,1 Chandy T,1 Edwards C,1 Hampton C,1 Lewis DR1
Plain English Summary
Why we undertook the work: Supervised exercise therapy can help improve the symptoms of persons who suffer from pain in the legs as a result of narrowing or blockages in the arteries. Previous studies have found that patients’ attendance with supervised exercise programmes is not as good as it could be, but the reasons for this are not clear. We wanted to find out how many patients with arterial leg pain attended a supervised exercise programme after being invited, and how many went on to finish the programme. We also wanted to find out if patients living in deprived areas were more or less likely to attend the supervised exercise programme. Additionally, we wanted to see if there were any factors that made it more likely that patients went on to attend or complete the programme, and whether patients reported feeling better after finishing the programme.
What we did: We looked at the medical records of patients who were invited to a supervised exercise programme to treat arterial leg pain between January 2017 and December 2018. We looked at data on deprivation in different areas of Wales produced by the government and analysed the data to answer our questions.
What we found: We found that 28 out of 164 patients (17.1%) attended the first appointment and 12 out of 164 (7.3%) completed the programme. There was no evidence that living in a deprived area made any difference to whether patients would attend or complete the programme, but the numbers are small.
What this means: The number of patients attending and completing the programme was low in this study. Our next aim is to find out why this is so that we can hopefully help more people with this treatment.
Abstract
Introduction: Supervised exercise is the first-line management for intermittent claudication and researchers must demonstrate that it is acceptable to patients and sustainable. Non-compliance with supervised exercise is an incompletely understood issue. It is unknown whether living in a more socioeconomically deprived area is associated with non-compliance with supervised exercise.
Methods: Consecutive patients referred to the National Exercise Referral Scheme (NERS) for intermittent claudication from a single centre from January 2017 to December 2018 were eligible for inclusion. The Welsh Index of Multiple Deprivation (WIMD) was used as a measure of deprivation for small areas in this study. The primary outcome was number of patients attending the NERS programme after referral. Secondary outcomes were number of patients completing the NERS programme, factors associated with attending and completing the NERS programme, and quality of life scores (EQ-5D-5L).
Results: Of the 164 patients in our cohort, 28 (17.1%) attended the exercise programme and 12 (7.3%) completed the full programme. Living in a more socioeconomically deprived area was not associated with attending the programme or completing the programme. There was insufficient quality of life score data for meaningful analysis.
Conclusions: The uptake and completion rate for supervised exercise in this cohort was low. There was no association between living in a more socioeconomic deprived area and either of these outcomes. Further qualitative research is needed to understand patients’ perspective of barriers to compliance with exercise programmes and how to overcome them.
Introduction
Intermittent claudication is ischaemic muscle pain resulting from impeded arterial blood flow that is precipitated by exercise and relieved by rest. It is thought to have a prevalence of up to 10%.1 National and international guidelines recommend supervised exercise, in conjunction with risk modification through lifestyle changes and best medical therapy, as first-line management for intermittent claudication.2,3 There is a well-supported consensus that exercise – specifically supervised walking exercise – is a cornerstone of intermittent claudication management.4-7 Supervised exercise often comes at a cost to the patient, and previous research has identified that uptake and compliance with exercise programmes could be improved.8,9 Identifying how compliance with supervised exercise can be maximised directly addresses the top two peripheral arterial disease research priorities from the perspective of patients/carers and clinicians/healthcare professionals.10 Factors associated with not engaging with supervised exercise are incompletely understood. Some of the potential barriers that have been identified include lack of education/understanding about intermittent claudication and the role of exercise, timing of the programme, cost of travel to the programme and other medical issues.11 However, previous studies have not explored whether socioeconomic depression could be a barrier to engaging with supervised exercise. It is unknown whether socioeconomic deprivation is associated with supervised exercise non-compliance. The primary objective of this study was to determine the proportion of patients referred to a national supervised exercise scheme from one health board in Southeast Wales that go on to attend the programme. Secondary objectives were to determine the proportion of patients that complete the exercise programme, to determine whether living in a more socioeconomically deprived area was associated with not attending and not completing the exercise programme, and to determine whether quality of life scores improved by completing the programme.
Methods
This study is reported in accordance with recommendations from the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).12 Local approval for service evaluation was obtained prior to starting data collection (reference number: SA/958/19). Funding required to access data from the supervised exercise programme was provided by the Gwent Vascular Institute, Aneurin Bevan University Hospital.
Patient identification and baseline demographic data collection
Consecutive patients referred to the National Exercise Referral Scheme (NERS) for the management of intermittent claudication from a single centre in South Wales over a two-year period (from January 2017 to December 2018) were eligible for inclusion. Patients were referred to the NERS from vascular outpatient clinics by consultants, registrars or vascular nurse practitioners. Referrals were made following a diagnosis of intermittent claudication if the patient indicated willingness to engage in supervised exercise and agreed to the referral after discussion with the healthcare professional. Contraindications to referrals included recent myocardial infarction, uncontrolled severe hypertension, uncontrolled arrhythmias and unstable acute heart failure. A copy of every referral is stored in the vascular department. Patients were retrospectively identified using copies of the NERS referrals from electronic records in the vascular surgery department. Baseline demographic data were collected from hospital electronic health records. The following baseline data were collected: age at time of referral, postcode data, diabetes mellitus, hypertension, chronic kidney disease, ischaemic heart disease, stroke, transient ischaemic attack, chronic obstructive pulmonary disease, smoking status (current, ex, never) and body mass index.
National Exercise Referral Scheme (NERS) and deprivation data
NERS provides tailored supervised exercise for patients referred by healthcare professionals in both primary and secondary care. The scheme is funded by the Welsh Government and managed by the Welsh Local Government Association and Public Health Wales. The scheme aims to provide supervised exercise for patients with varying chronic health issues including cardiovascular health issues. Patients presenting with intermittent claudication are eligible for referral to the scheme; tailored supervised exercise for this group includes walking exercise activities aiming to increase participants’ walking distance. Patients can attend twice a week for a total of 16 weeks. The activities are delivered as group sessions and last 1 hour each. Patients have a choice of available locations and times to attend and are required to pay £2.00 for each session. The cost is fixed regardless of location or reason for referral.
Data regarding NERS appointments are not immediately available to secondary care teams since they are not on hospital electronic health records. These data are stored by Secure Anonymised Information Linkage (SAIL), a databank funded by the Welsh Government and Care Research Wales. The application for access to data was approved by SAIL’s Information Governance Review Panel (project number: 0897). Data on patients identified on local hospital electronic health records were submitted for linkage with SAIL data. Additional data provided by SAIL in an anonymous format were: Welsh Index of Multiple Deprivation ranks, NERS attendance (first appointment, withdrawal/completion) and quality of life questionnaire EQ-5D-5L (at start and end of programme).13
The Welsh Index of Multiple Deprivation (WIMD) is the Welsh Government’s official measure of deprivation for small areas in Wales and was used in this study.14 The index is based on multiple measures of deprivation: income, employment, health, education, access to services, housing, community safety and physical environment. The index ranks all small areas in Wales from 1 (most deprived) to 1,909 (least deprived). WIMD was used in this study to represent the deprivation experienced in the small area (with an average population of 1,200 people) in which each patient resided.
Outcomes
The primary outcome was the number of patients attending the NERS programme after referral. Secondary outcomes were the number of patients completing the NERS programme (attending weekly sessions for 16 weeks total), quality of life and multivariate analysis results to identify factors associated with attending and completing the NERS programme.
Statistical analysis
Each patient was assigned a WIMD rank based on postcode data and the cohort was split into quartiles for describing demographic and comorbidity data. The WIMD rank was used as a continuous variable for regression analyses (as opposed to using the quartiles as categorical data). Categorical data were compared between the quartiles using the χ2 test and continuous data were analysed for normality and parametric or non-parametric tests used as appropriate.
Multiple imputation was performed to handle missing data using the Markov chain Monte Carlo method with 25 imputation sets and 25 iterations prior to regression analyses. Binary regression analyses were used to identify predictors of attending the NERS programme, predictors of completing the NERS programme, and predictors of withdrawing from the NERS programme. Univariate analysis was performed, with variables reaching a statistical significance threshold of p<0.1 carried forward to multivariate analysis. Results were presented as odds ratios (ORs) with corresponding 95% confidence intervals (95% CI). Statistical significance was defined as p<0.05. Regression analyses were conducted on imputed data followed by analysis using case-wise deletion as sensitivity analyses. Data were analysed using SPSS version 26 (IBM, New York, USA).
Results
The total number of referrals to NERS between 1 January 2017 and 31 December 2018 was 268. All 268 referrals were for intermittent claudication. Following exclusions for no matches on the SAIL database and those patients still on the waiting list for their first NERS appointment, 164 patients were included in the analyses.
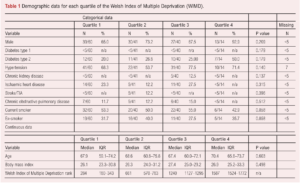
Demographic and comorbidity data
The median age at time of referral was 68.3 years (interquartile range (IQR) 60.4–73.5). Males accounted for 68.9% (113/164), 42/164 (25.6%) had type 2 diabetes, 111/164 (67.7%) had hypertension, 15/164 (9.1%) had chronic kidney disease, 36/164 (22.0%) had ischaemic heart disease, 12/164 (7.3%) had a previous stroke or transient ischaemic attack and 20/164 (12.2%) had chronic obstructive pulmonary disease. Most patients were current smokers (84/163; 51.5%) and 55/163 (33.7%) were ex-smokers. Median (IQR) body mass index was 26.7 (24.0–30.2) kg/m2.
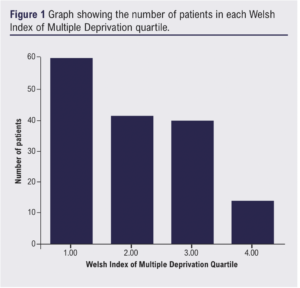
The median (IQR) WIMD rank was 644 (319–1183). WIMD rank was not available for nine patients. The cohort was split into quartiles based on the total range of WIMD ranks in Wales (1–1909). Quartile 1 (least deprived areas) had 60/155 (38.7%) patients, quartile 2 had 41/155 (26.5%) patients, quartile 3 had 40/155 (25.8%) patients and quartile 4 (most deprived areas) had 14/155 (9.0%) patients (Figure 1). The quartiles were equivalent in terms of demographics and comorbidities (Table 1).
Imputed data (multiple imputation) addressed the nine patients with missing WIMD data and the two patients with missing smoking status data.
NERS outcomes
Of the 164 patients in our cohort, 28 (17.1%) attended the exercise programme and 12 (7.3%) completed the 16-week programme.
The variables reaching the threshold of p<0.1 on univariate analysis to predict whether patients attended the NERS programme were type 2 diabetes (OR 0.304 (95% CI 0.087 to 1.070), p=0.064) and WIMD rank (OR 0.999 (95% CI 0.998 to 1.000), p=0.093). Sex, age at time of referral, body mass index, type 1 diabetes, hypertension, chronic kidney disease, ischaemic heart disease, stroke/transient ischaemic attack, chronic obstructive pulmonary disease and smoking status were not significant. Neither type 2 diabetes (OR 0.348 (95% CI 0.097 to 1.241), p=0.104) nor WIMD rank (OR 0.999 (95% CI 0.998 to 1.000), p=0.144) were significant on multivariate analysis (Table 2). Sensitivity analysis results using case-wise deletion were similar to results from analyses conducted on imputed data (Appendix 1).

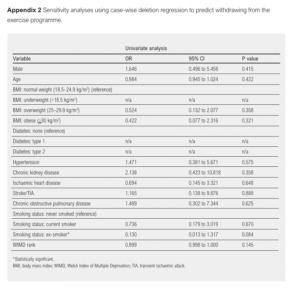
The only variable to reach the threshold of p<0.1 on univariate analysis to predict whether patients would not complete the NERS programme after starting was smoking status (ex-smoker): OR 0.130 (95% CI 0.013 to 1.317), p=0.084 (Table 3). WIMD rank did not meet the threshold (OR 0.999 (95% CI 0.998 to 1.000), p=0.156). Sensitivity analyses results using case-wise deletion were similar to results from analyses conducted on imputed data (Appendix 2).

The number of patients who completed the EQ-5D-5L questionnaire at the beginning and after completing the 16-week programme (n=12) was deemed too low to allow for meaningful statistical analysis due to the high risk of a type 2 error.
Discussion
The overall rate of supervised exercise uptake in our cohort was 17.1% (28/164) and the completion rate was 7.3% (12/164). Living in a more socioeconomically deprived area reached the threshold of p<0.1 on univariate analysis to predict taking up the programme. However, it was not an independent predictor of taking up the programme on multivariate analysis. Smoking status (ex-smoker) was the only variable to reach a threshold of p<0.1 on the secondary univariate analysis, and was associated with a lower likelihood of withdrawing from the programme. The mean scores for the mobility, usual activities, pain/discomfort and anxiety/depression domains of the EQ-5D-5L demonstrated a non-significant trend of improvement after completing the programme.
The rate of supervised exercise uptake, adherence and completion reported in the literature is variable,9,15-17 ranging from 24% to 78%. The uptake and completion rate in this cohort is lower than the majority of that reported in the literature.15-17 One possible reason for the discrepancy is that trial conditions may report over-optimistic rates,9,18,19 but other factors such as differences in prior education/expectations of supervised exercise for intermittent claudication,20 transport provision, cost of enrolment21,22 and lack of standardisation to supervised exercise are unknown variables that may account for the lower rates in our cohort.23 The NERS programme allows for patients to choose between different venues that provide the exercise sessions; however, we are not able to make conclusions about the patients’ perceived convenience of attending. It is possible that patients in this cohort have difficulty using suitable transport, especially if reliant on public transport that may require them to walk distances far greater than their claudication distance to reach stations. Similarly, the cost of attending the sessions is likely to be far greater than the £2.00 fee charged by NERS for patients that rely on public transport or taxis. Delays from referral to first session is another unknown variable that may have influenced the low uptake observed in this cohort.
Living in areas with more socioeconomic deprivation has been shown to be associated with lower levels of physical activity and utilisation of local facilities for exercise.24,26 This is not seemingly replicated when socioeconomic deprivation and supervised exercise for intermittent claudication are considered based on findings from this cohort. Other factors such as lack of understanding of the pathology of intermittent claudication, pain,27 motivation,28 other (non-PAD) health issues,9,27,28 cost29 and family/work/transportation issues may be more relevant barriers.28,29 Ex-smoking status was associated with a lower likelihood of withdrawing from the programme; it is possible that since these patients had a previously positive experience of lifestyle change, they were more likely to go on and complete the programme.
There were insufficient data to undertake meaningful statistical analyses using the EQ-5D-5L quality of life measure following completing the 16-week programme in this study. Findings from other studies have been in favour of improved quality of life following supervised exercise.19,30 However, it is worth noting that, despite there being a consistent finding of improved disease-specific quality of life measures (such as the walking impairment questionnaire) with supervised exercise,19,30,31 results are conflicting when generic quality of life measures are evaluated.7,19,30 Disease-specific quality of life measures should be considered by NERS in the future.
The results from this study highlight the poor uptake and compliance with supervised exercise for intermittent claudication in Southeast Wales and suggest that efforts to improve this should focus on known barriers, regardless of the socioeconomic deprivation in the area in which patients reside. The demographics of our cohort are as would be expected for a cohort with intermittent claudicants, increasing the generalisability of the results.
There are several questions that remain to be addressed by further research. Further studies should evaluate socioeconomic deprivation and supervised exercise uptake/compliance in other geographical areas. Despite having a strong evidence base demonstrating the short-term benefits of supervised exercise, longer-term outcomes require further evaluation,32 and evidence suggests that sustained engagement in physical activity is needed to maintain the improvements in outcomes.15 It is unknown whether the barriers to supervised exercise attendance/compliance in the short term will pose the same challenges following completing a supervised exercise programme. A recent systematic review identified that “lack of motivation”, “health reason not related to supervised exercise therapy”, and “patient choice” were the three most frequent reasons for incomplete adherence to an exercise programme for intermittent claudication.9 Further qualitative research is needed to understand these issues from the patients’ perspective and to identify whether they would also influence long-term engagement in physical exercise. Reducing key barriers by increasing provision and accessibility should also increase acceptability to patients.
There are limitations to this study. Firstly, some patients were excluded due to their records being unable to be linked with data on the SAIL platform, potentially introducing bias. There was potential confounding in our regression analyses from unknown variables such as patients’ depth of knowledge about the pathology and of supervised exercise, access to transport and psychological factors that may influence attendance. Similarly, there is a limitation to regression analyses since there were relatively low numbers of patients included. We used the WIMD in our analysis as we did not have patient level deprivation data available, therefore our results cannot be extrapolated to make assumptions about how individual socioeconomic deprivation influences uptake and completion of supervised exercise. Several patients could not be included in the analyses because the data could not be linked with SAIL records or they were still waiting to be invited for their first appointment. Long delays (unknown to us) could be a confounder when evaluating compliance. There were far fewer patients in the fourth quartile (most deprived areas) compared with the other quartiles. It is possible that patients living in the most deprived areas have unequal access to healthcare and may not have presented to the vascular service, introducing potential bias. There were insufficient data to allow for analyses of quality of life outcomes and no disease-specific quality of life measures were recorded. The NERS programme does not meet the National Institute for Health and Care Excellence (NICE) recommendations for supervised exercise for intermittent claudication,33 meaning our results may not be applicable to programmes that do meet the recommendations.
Conclusion
The uptake and completion rate for supervised exercise in this cohort was low. There was no association between living in a more socioeconomic deprived area and either of these outcomes. Further research is needed to understand the patients’ perspective of barriers to access, uptake and compliance with exercise programmes and how to overcome them.

Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;Vol1(4):130-136
Publication date:
July 21, 2022
Author Affiliations:
1. Gwent Vascular Institute, Royal Gwent Hospital, Newport, UK
Corresponding author:
Mr Brenig Llwyd Gwilym
Gwent Vascular Institute, Royal Gwent Hospital, Cardiff Road, Newport NP20 2UB, UK
Email: [email protected]











