ORIGINAL RESEARCH
Management of lower limb ischaemia using hybrid techniques: a single-centre experience
Chana MS,1 Leckey S,1 Paravastu SCV,1 Kulkarni SR1
Plain English Summary
Why we undertook the work: To provide outcomes of Hybrid procedures in a single vascular centre.
What we did: We undertook a retrospective review of the outcomes of patients undergoing hybrid procedures for lower limb ischaemia. This involves procedures combining traditional open surgery, in combination with an endovascular procedure.
What we found: Our results showed an acceptable rate of vessel patency and symptom resolution, and an acceptable rate of surgical complications.
What this means: The results of this study support the use of hybrid procedures in managing multilevel arterial disease causing lower limb ischaemia.
Abstract
Introduction: Modern vascular surgery combines procedures with both open and endovascular techniques, with these hybrid procedures becoming part of routine arterial surgery. Hybrid procedures have been established in this centre with access to a hybrid suite since 2014. The aim of this study was to characterise patients undergoing hybrid procedures including an open groin dissection plus an endovascular component.
Methods: A retrospective review of operation notes, electronic health records and radiology software for patients undergoing hybrid revascularisation for critical limb threatening ischaemia (CLTI) or intermittent claudication (IC) between January 2017 and December 2021 was performed. Any open groin surgical procedure including common femoral endarterectomy and/or lower limb bypass plus any endovascular procedure were recorded. Primary outcomes were recorded as stent patency, a composite of tissue healing or symptom resolution, and wound complications including surgical site infections. Secondary outcomes were length of stay, rate of readmission and mortality at 30 days.
Results: A total of 98 patients (77 men) of median age 73 years (IQR 68–78) underwent a hybrid procedure during this period. Treatment was for CLTI in 66% of the patients and for IC in 34%. The median length of stay was 5 days. Overall graft and stent patency was 85%. The overall rate of tissue healing and symptom resolution was 92%. The surgical site infection rate was 14% (14/98) and mortality at 30 days was 2%.
Conclusion: Hybrid revascularisation is safe and effective in treating CLTI and IC with an acceptable risk of surgical site infections. Our short-term results suggest that hybrid revascularisation should be considered in patients with multilevel disease.
Introduction
Peripheral arterial disease (PAD) is recognised as an increasing global healthcare issue.1 Chronic limb-threatening ischaemia (CLTI) resulting from PAD is the term adopted in the 2019 Global Vascular Guidelines. It is defined as ‘a broader and more heterogeneous group of patients with varying degrees of ischemia that may delay wound healing and increase amputation risk’.2 CLTI has been identified as the leading cause of limb loss and a significant cause of premature mortality worldwide.3 Surgeons treating vascular disease must be skilled in both open and endovascular techniques, with hybrid surgery becoming a routine part of arterial surgery to treat CLTI.4 These strategies can be used to treat multiple levels of disease and have been shown to be feasible in patients with complex disease in whom less invasive procedures are beneficial.5-7 Access for these procedures is commonly gained at the femoral vessels in the groin. This is a common site for surgical site infection (SSI), which is associated with preventable morbidity and mortality as well as increased healthcare cost.8
Gloucestershire Hospitals NHS Foundation Trust provides Vascular Surgery services as an arterial hub for the regional Vascular network. Access to a hybrid suite in this centre was established in 2014. This has permitted the burgeoning development of hybrid revascularisation strategies to treat multilevel arterial disease. The patient population undergoing these procedures and the outcomes of this practice have not yet been described.
The aim of this retrospective cohort study was to characterise the population of patients undergoing hybrid procedures including an open groin dissection for common femoral endarterectomy plus an endovascular component; to describe the therapeutic effect; to describe the stent patency rate; to describe the rate of SSI; and to describe mortality rates.
Methods
A retrospective review of consecutive patients undergoing hybrid revascularisation of the lower limbs for either CLTI or disabling short distance intermittent claudication (IC) at our centre between January 2017 and December 2021 was performed. Data were collected by case notes review, electronic health records and radiology software on patient demographics, procedure performed, operative procedure time, length of stay, clinical outcomes, groin complications and mortality at 30 days.
Operative procedures performed
Open groin surgical procedure included common femoral endarterectomy and/or lower limb bypass. This was performed in conjunction with an endovascular procedure including either an iliac or femoropopliteal angioplasty and/or stent or both inflow and runoff procedures.
Follow-up and outcomes
Patients are usually followed up 6 weeks after discharge from the hospital. All patients undergoing a stent and/or a bypass procedure have a 6-week stent and/or graft surveillance duplex scan as a routine in out Trust. Further surveillance is organised based on the individual case. Primary outcomes were recorded as stent patency at follow-up, a composite of tissue healing or symptom resolution, and wound infection or complication. Secondary outcomes were length of stay, rate of readmission and mortality at 30 days.
Statistical analysis
Descriptive analysis was performed using Microsoft Excel (Microsoft, USA). Median + interquartile range (IQR) was used for continuous data (length of stay in days, procedure time in minutes, follow-up time in weeks). Percentage (%) was used for continuous data (index pathology, procedure performed, outcomes and complications).
Results
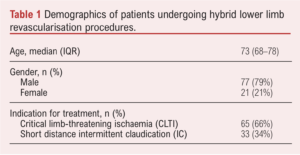
A total of 98 patients underwent a hybrid procedure during the study period, of which 79% were male (n=77) with a median age of 73 years (IQR 68–78). Treatment was indicated for CLTI in 66% (n=65) and short distance IC in 34% (n=33) of cases. These demographics are shown in Table 1.
Operative procedures
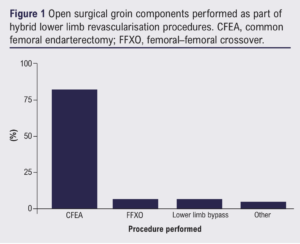
The most commonly performed groin procedure was common femoral endarterectomy (n= 79; 81%). Femoral–femoral crossover was performed in 7% (n=7) and lower limb bypass was performed in 7% (n=7). Femoral exposure for other reasons was recorded in 5% (n=5). These data are shown in Figure 1.
Endovascular procedures
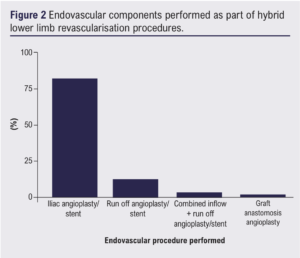
The most commonly performed endovascular procedure was iliac angioplasty/stent (83%, n=81). Run-off vessel angioplasty/stent was performed in 13% (n=13), combined inflow and run-off angioplasty/stent were performed in 3% (n=3) and angioplasty to proximal anastomosis of aortobifemoral graft in 1% (n=1). These data are shown in Figure 2.
Primary outcomes
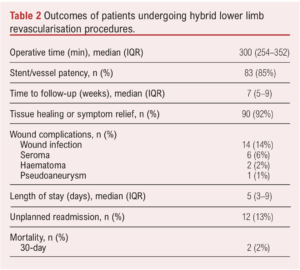
The median operative procedural time was 300 min (IQR 254–352). The median time to first outpatient follow-up was 7 weeks (IQR 5–9), at which point stent/vessel patency was present in 85% of patients (n=83). Tissue healing or symptom resolution was documented in 92% of patients (n=90). Wound infection was reported in 14% (n=14), seroma in 6% (n=6), haematoma in 2% (n=2) and pseudoaneurysm was reported in 1% (n=1). Seromas were managed conservatively and resolved on further follow-up. The patient with pseudoaneurysm was also managed conservatively with follow-up scans and it eventually occluded without intervention. All patients with documented wound infection (n=14) required antibiotic treatment and in 11 patients no further intervention was required. In the remaining three patients, one required negative pressure dressing therapy for dehiscence, one required wound washout and one required removal of an infected graft and subsequent above-knee amputation. Both patients with haematomas required washout and a sartorius flap.
Secondary outcomes
Median length of stay was 5 days (IQR 3–9). The rate of unplanned readmission for wound-related complications was 13% (n=12). Mortality at 30 days was 2% (n=2); these deaths were from unrelated causes. These data are shown in Table 2.
Discussion
PAD resulting in CLTI and short distance IC is prevalent in both elective and emergency vascular practice. It has a significant cost to patients in terms of quality of life, to healthcare systems and society.9 It is multifactorial, and by the time of presentation in increasingly comorbid patients its treatment may often be complex. Hybrid strategies to treat complex multilevel arterial disease are becoming more common and have been shown to be beneficial in high-risk patients.7 As such, the modern vascular surgeon is trained in the UK in both open surgical and endovascular techniques. These procedures often require open surgical access to the femoral vessels and are multistep, often requiring a multitude of equipment, resulting in a longer surgical time. The outcomes of hybrid procedures performed in this unit have not previously been described.
Based on the results of this single-centre retrospective cohort study, it appears that hybrid revascularisation in selected groups of patients with CLTI and IC is both safe and feasible. Vessel/stent patency was seen in the majority of patients at first outpatient follow-up. This correlated in favourable rates of tissue healing and symptom resolution, seen in 92% of patients. Although the procedure time was relatively long, length of stay was as expected at a median of 5 days with a low 30-day mortality in this high-risk group of patients undergoing complex procedures.
The implementation and continued use of hybrid strategies in this single UK centre is similar to that published internationally, with data from the Vascular Quality Initiative (USA) reporting up to one-third of lower extremity revascularisations being performed with a hybrid strategy.6 Its use has been shown to have favourable perioperative outcomes and should be considered in high-risk patients.6 Another large study examining perioperative outcomes in patients undergoing bypass surgery and hybrid procedures found higher rates of systemic complications, infection, postoperative transfusion and readmission in patients undergoing bypass procedures compared with hybrid procedures for femoropopliteal disease.10 A smaller study examining hybrid strategies for aorto-iliac segment disease reported shorter operative times, less blood loss and better surgical morbidity, with favourable primary patency rates at follow-up.11 The results of our study corroborate these findings and support the use of hybrid strategies as feasible and effective.
Surgical site infection was seen in 14% of the patients in this study. This is comparable to the recently published GIVE study, which is a multicentre study examining groin wound infections following femoral exposure for any non-infective cause.8 The authors reported a rate of surgical site infection of 8.6% in all patients. However, when looking specifically at procedures with ‘groin access (±groin intervention) for endovascular aorto-iliac/infra-inguinal occlusive disease’, the rate of surgical site infection was 12.1%. This is comparable, albeit lower, than the 14% rate of wound infection in our cohort. The development of surgical site infection in the GIVE study was reported to be frequent and carries significant sequelae. They recognised increased surgical time as a risk factor for developing surgical site infection. The group developing surgical site infection had a median operating time of 3.3 hours (198 min), which was significantly longer than the SSI group without surgical site infection (p=0.02). It is reasonable to suggest that hybrid strategies encounter more steps and can require more operative time. Our median operating time for hybrid procedures of 300 min is certainly in excess of the GIVE study and could be a contributing factor to the higher infection rate in our cohort. This increase in operative time is a result of combining two complex procedures together (open and endovascular), delaying the final completion.
All measures and efforts should be taken to reduce operative time and the risk of developing surgical site infection as far as possible. One possible strategy to reduce operative time would be to stage various levels of treatment, with an endovascular component happening separately from an open surgical procedure. Whilst this uncoupling of the hybrid procedure would reduce individual procedure time, it increases the number of intervention events and their associated risk for the patient, and has logistic and clinical service capacity implications. Furthermore, if a staged strategy were used to treat multilevel disease, there is a potential delay in achieving adequate treatment and clinical outcomes, with potential increased risk of limb loss. Therefore, we would advocate that, rather than stage treatment, modern practice should aim to optimise efficiency and theatre governance to reduce the time taken to complete hybrid procedures, ideally within a bespoke hybrid suite.
We acknowledge the methodological limitations of this study as a retrospective review, the small sample size and that cases may have been missed. Similarly, the outcome period studied was short and we cannot comment on longer term graft/stent patency or mortality. However, we have examined a common pathology seen in UK Vascular surgery practice, making our findings generalisable. Corollary work should include prospective evaluation and include more long-term follow-up, data regarding limb salvage and amputation rate, and could take the form of a registry-based collaborative study.
Conclusion
This study aimed to describe a cohort of patients undergoing hybrid lower limb revascularisation for CLTI and short distance IC, and to examine the outcomes following these strategies. The results show that patients with complex multilevel arterial disease can be safely and effectively managed using these strategies, with an acceptable rate of complications.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(2):65-68
Publication date:
January 24, 2023
Author Affiliations:
1. Gloucestershire Hospitals NHS Foundation Trust
Corresponding author:
Sachin R Kulkarni
Consultant Vascular and Endovascular Surgeon,
Dept of Vascular Surgery Gloucester Royal Hospital Great Western Road Gloucester, GL1 3NN, UK
Email: [email protected]











