ORIGINAL RESEARCH
Nurse-delivered endothermal venous ablation: 12 years’ experience at a single UK centre
Cooper B
Plain English Summary
Why we undertook the work: Varicose veins and venous disease (veins in the legs that do not return blood properly) affect many people through a range of symptoms including complications such as bleeding, clotting and the development of wounds that are difficult to heal (venous leg ulcers). Early assessment and early access to surgical treatment can improve people’s lives and help to heal venous leg ulcers more quickly. Early access to this type of surgery can be difficult in the UK due to a lack of resources within the NHS. The aim of this report is to describe innovative delivery of a venous service through advanced nursing practice.
What we did: A specialist nurse was trained to deliver this type of surgical procedure to overcome difficulties in accessing care at one UK hospital. A range of data around this practice and the patients treated was collected for a period of 12 years.
What we found: It was found that this type of surgical procedure can be safely delivered by a trained specialist nurse. Patients experienced shorter waiting times (average 53 weeks reduced to 17 weeks) and positive outcomes that were comparable to surgeon-delivered procedures.
What this means: Access to care and patient waiting times can be improved through specialist nurse care. Services for this patient group may become more sustainable by embracing specialist nurse-delivered procedures.
Abstract
Background: Despite new evidence supporting early assessment and intervention for patients with venous disease, there remain significant barriers to service delivery in the UK. The aim of this report is to describe the innovative delivery of a venous service through advanced nursing practice. Single-centre data are presented from 12 years of nurse-delivered venous interventions.
Methods: An existing nurse specialist was trained to (1) receive and vet referrals, (2) assess patients and (3) perform endovenous laser ablation (EVLA) and foam sclerotherapy. Consultant surgeons provided mentoring and assessment over a 10-month period, with ongoing team support thereafter. Qualifications were obtained in medical ultrasound and prescribing. Procedures were performed under local anaesthesia in a clinical treatment room setting. Audit data were maintained throughout. Complications were reported via risk management systems.
Results: Between 2012 and 2023, 6655 referrals were vetted and, of these, 3710 (56%) were seen and assessed. Of the 3710 assessed, 2148 (58%) patients (median (IQR) age 51 (40–53) years, 55% female) underwent nurse-delivered EVLA of the great (84%) or small (16%) saphenous vein. Complications were recorded for 25 cases (1.2%). Median waiting time before the nurse-delivered service was 53 weeks (2011). Across the reported period of nurse-delivered service, this reduced to a median of 17 weeks. In 2023, median (IQR) waiting time for the venous leg ulcer cohort was 7 (3–11) weeks. Early follow-up showed vein closure rates of 95%. High levels of patient satisfaction were recorded: where a score of 10 was most satisfied, the median (IQR) satisfaction score for clinical outcome was 8 (6–8) and satisfaction with a nurse-delivered service was also 8 (7–8).
Conclusions: The venous service within this single UK centre is being delivered through advanced nursing practice, improving waiting times and access to intervention. A significant efficiency in consultant surgeon time is being realised, increasing the capacity of the vascular unit. A low complication rate and positive patient satisfaction suggests that nurse-delivered EVLA is a safe innovation in service delivery.
Introduction
Attention is currently being directed towards the care of patients with venous disease in the UK. Contemporary research supports early intervention of incompetent superficial truncal veins, especially beneficial to patients suffering from venous leg ulceration (VLU). However, there are significant difficulties in the delivery of venous services impeding the implementation of best practice.
In 2012 a group of consultant vascular surgeons at a single UK centre aspired to improve the delivery of their venous service. Unable to increase their medical workforce and faced with expanding workloads of increasing complexity, the capacity to deliver timely venous interventions was failing; median (IQR) referral to treatment time (RTT) in 2011 had risen to 53 (45–59) weeks.
This report aims to describe innovative practice designed to address barriers to service delivery through the development of advanced nursing practice at a single UK vascular surgery unit. Data are presented from 12 years’ experience of nurse-delivered venous interventions.
Background
Assessment and treatment
The assessment and treatment of patients presenting to vascular services with symptomatic varicose veins and the consequences of chronic venous insufficiency represents a high-volume workload; more than 30,000 procedures per year are carried out in England alone.1 Varicose veins affect 10–40% of the adult population in the UK and are associated with a wide range of symptoms including significant complications such as bleeding, superficial thrombophlebitis and VLU.2 VLU is the most severe manifestation of chronic venous insufficiency and is associated with a significant impact on quality of life through pain, impaired mobility, foul smelling exudate, depression, loss of self-esteem, social isolation, employment difficulties and the need for long-term clinical support.3 It is no surprise that the management of this chronic recurring condition carries a significant financial burden to the National Health Service (NHS) in the UK, thought to consume over £2.7 billion of funding per year.4
The traditional paradigm in the treatment of this condition has consisted of high ligation and stripping of the superficial truncal veins, often combined with phlebectomies of truncal tributaries.5 In the case of VLU, the classic narrative has been to treat with compression therapy until wound healing is achieved, only addressing underlying aetiology surgically at this late stage. Referral and treatment pathways have been shown to be poorly established and poorly understood; often patients with VLU are never considered for surgical management of their underlying venous insufficiency.6
The advent of endovenous approaches, in particular endothermal ablation of the superficial truncal veins, has led to a phasing out of traditional high ligation and stripping in all but the most complex of cases.7 Current National Institute for Health and Care Excellence (NICE) guidance recommends endothermal ablation as the first choice for intervention, where clinically and technically appropriate.8 The advantages over open surgery are numerous and include short recovery time, fewer complications, treatment under local anaesthesia and shorter hospital stay.9
Evidence and barriers to best practice
The potential for surgical treatment of incompetent superficial truncal veins to benefit and improve VLU treatment are best summarised in the results of several studies challenging traditional rationale. The ESCHAR trial, published in 2007, concluded that most patients with VLU would benefit from superficial venous surgery as an adjunct to compression through significantly improved ulcer-free time post wound healing.10 More recently, the EVRA trial has demonstrated accelerated healing times of venous leg ulcers alongside increased ulcer-free time through early ablation of underlying incompetent superficial truncal veins.11 It was concluded that an early intervention strategy was highly likely to be cost-effective and associated with long-term improvements to patients’ quality of life.12 By its own merit, the results of the EVRA trial alone ask for a change in behaviour to facilitate early venous assessment and intervention.13
Actual and anticipated barriers to early assessment and intervention were identified in a post EVRA trial study. These included lack of operating space or time, theatre capacity, lack of trained staff, duplex scanning capacity, primary/secondary care integration/referral, financial reimbursement, resistance from colleagues, cost of change, local and national guidelines.14 Vascular surgery services in the UK do not appear to have the capacity, workforce or financial ability to implement the evidenced changes required to improve access to venous interventions for this patient group. This has been demonstrated through sequential Vascular Society of Great Britain and Ireland (VSGBI) reports showing an ever-increasing burden of vascular disease upon the population, resultant year on year rises in service demand and consistent deficits in the number of both vascular consultants and trainees to meet current and future requirements.15,16
An inability to surpass these barriers will result in a missed opportunity to improve access to treatment and patient outcomes; success, as the title of one post EVRA study suggested, could provide a “new hope for people with venous ulcers”.17
A 2023 All-Party Parliamentary Group on Vascular and Venous Disease report, addressing the future of venous disease, recognised the condition as a growing problem being addressed by a shrinking workforce.18 The same document realises that there exists a workforce shortage of vascular surgeons and of trainee posts in the UK, resulting in the prioritisation of some vascular conditions over others, potentially impacting negatively upon the wellbeing of those suffering from venous disease.18
Both the All-Party Parliamentary Group and VSGBI reports recommend innovation at service level and change in how clinicians practice to better use limited resources.15,16,18
Nurse-delivered surgical procedures
A recent series of papers published between 2022 and 2024 examined the worldwide phenomenon of nurse-delivered surgical procedures. They found a near 70-year modern history of nurses performing surgeries across 26 countries, spanning most surgical specialties including urology, oncology, cardiothoracic, orthopaedic and vascular surgery.19-21 The reasons for development of nurses to deliver surgical procedures varies; however, one common theme, recognised by the World Health Organisation (WHO), is task shifting in response to supply and demand deficits.22
This report presents data from 12 years of innovative venous service delivery through nurse-delivered surgical procedures at a single UK centre, conceived by vascular consultant surgeons and developed as a solution to vascular service delivery supply and demand deficits.
Methods
Patient pathway
The reporting vascular unit is a tertiary referral centre and university teaching hospital serving a population of more than 500,000 across a large geographical area. Primary care referrals are received from a network of 70 GP practices across this area.23
In 2018, NHS Scotland issued a protocol for access to varicose vein surgery where indications for treatment equated to CEAP C4–C6 symptoms.24 In accordance, patients referred with uncomplicated varicose veins (CEAP C0–C3) are not offered treatment at this centre. Referrals are returned to primary care at the vetting stage where referral criteria are not met; similarly, patients who do not meet referral criteria when assessed in outpatient clinic are not offered treatment. Prior to nurse delivery of the venous service, there was no accelerated pathway for patients suffering C6 symptoms (active VLU).
Development
An existing vascular nurse specialist (VNS) was trained to deliver the unit’s venous service, accounting for approximately 20% of the VNS job plan. This comprised receiving direct referrals, delivery of ‘one-stop’ assessment clinics and venous interventions (endovenous laser ablation (EVLA) and foam sclerotherapy). This initiative was conceived and driven by consultant surgeons to improve patient access to venous interventions, release medical workforce capacity and ensure continued delivery of a venous service at this centre.
The VNS was mentored by two vascular consultant surgeons. Nurse practice education facilitators (PEFs) were employed in the production of a locally agreed capability and competency framework, informed by mentors, using best available evidence and developed alongside hospital and nursing management teams.
At first, the VNS shadowed venous assessment clinics, building the experience and competence to deliver this part of the service with autonomy. In assessment, all patients were physically examined, verbally discussed their condition and underwent duplex ultrasound imaging performed by the VNS. Ultrasound skills were taught locally by resident vascular sonographers before undertaking a formal postgraduate qualification in medical ultrasound with a vascular focus. A record was maintained of all assessments and ultrasound investigations completed in the compiling of evidence towards competency.
EVLA was taught by one mentor. The procedure and skills required were broken down into component parts and progressively taught over a six-month period. An additional four months of supervised practice was completed where the VNS was observed and assessed as competent in delivering the procedure in its entirety. A prospective audit was maintained of all patients treated. Patient group directions were originally used in the prescribing of procedural medications; over time this was superseded by a qualification in non-medical prescribing and entry onto the Nursing and Midwifery Council registry of nurse prescribers.
EVLA was initially performed by the VNS in a day case operating suite under local anaesthesia, with intraoperative ultrasound performed by the VNS. In 2014 the transition was made to EVLA delivered in a clinical treatment room. Local anaesthesia (1% lidocaine) and tumescent saline were used in every case. Ultrasound-guided foam sclerotherapy (UGFS) of varicose saphenous tributaries was considered and performed in selected EVLA cases either concomitantly or within 8 weeks post EVLA.25 The decision to treat tributaries, either concomitantly or staged, was made on a case-by-case basis, considering the ability to treat the saphenous vein beyond the origin of the tributary, the size of the tributary and the potential impact on symptomatic relief.26,27
Compression stockings (Class II) were fitted immediately after the procedure with instructions to remain in situ for 7 days; additional compression bandaging was applied over the treated area with instructions to remove after 48 hours. In the delivery of EVLA, a 1470 nm diode laser was employed, operated in continuous mode between 5W and 7W power, delivering 30–50 Joules of energy per cm, dependent upon the vein being treated and vein diameter, in accordance with manufacturer guidance. In the delivery of UGFS, foam sclerosant was produced using either 1% or 3% sodium tetradecyl sulfate liquid converted to foam sclerosant via the Tessari technique.
In the first 24 months of practice (2012–2013), procedures were listed under the mentoring consultant vascular surgeon’s name alone and clinical correspondence signed by both mentor and VNS, constituting 2 years of close supervision. From 2014 onwards, following continued audit, review and discussion with the wider clinical and management teams, procedures were listed under the name of the VNS and clinical correspondence conveyed independently. Similarly, consent to treatment was observed and co-signed throughout the development period; a standard operating procedure for VNS obtained consent was developed by the PEF team alongside the capability and competency framework.
Although the VNS delivered EVLA independently once competent, support from consultant vascular surgeon colleagues was always available if required; this supportive team approach was integral to the clinical governance of this service development. Where complications occurred, they were reported via the DATIX risk management system, discussed at service level clinical governance meetings and escalated as appropriate.
Post-procedure evaluation
Within this centre, post-EVLA follow-up is not routine practice. However, in the evaluation of nurse-delivered treatment efficacy, a selection of patients received post-procedure ultrasound imaging in year 1 (2012) and year 2 (2013), performed by a vascular sonographer independent of venous service delivery 6 months post-procedure. Sonographer capacity restricted post-procedure ultrasound evaluation to 40 patients in 2012 and a further 40 in 2013; these were selected at random by the sonographer. Successful vein closure was defined as non-compressibility and absence of flow signal/colour filling along the full length of the treated saphenous vein on duplex ultrasound; proximal occlusion of the saphenous vein was expected to be within 5 cm of the saphenofemoral/popliteal junctions.
Evaluation of patient satisfaction was performed by questionnaire across the 2014/2015 period and again during 2016/2017. Main questions consisted of Likert scale responses, with 10 representing most satisfied; visual analogue pain scores ranked 10 as highest level of pain experienced. Full recovery was reported as time to return to work and/or return to normal daily activities. The questionnaire was of local design and did not use a validated assessment tool.
Identification of complications
Intraoperative complications were identified and recorded at the time of procedure delivery. Postoperative complications were identified following re-referral to the service from primary care or by direct contact with the service, instigated by the patient. It is likely that the incidence of minor to moderate postoperative complications, such as superficial thrombophlebitis of saphenous tributaries, has been under-reported in the absence of routine follow-up.
Data collection
Quantitative data were collected prospectively by the VNS for the purpose of audit, professional development and local clinical governance. VNS logbook entries were cross-checked against local health intelligence data for completeness.
Results
Referral and cases delivered
Over a 12-year period (2012–2023) 6655 referrals were received and vetted by the VNS. Of these, 3710 (56%) were seen and assessed; the remainder did not meet referral criteria. Of the 3710 assessed, 2148 patients (58%) underwent EVLA performed by the VNS. Of the remaining patients assessed, 441 (12%) underwent UGFS alone, 26 (0.7%) were listed for high ligation with or without phlebectomies under a vascular surgeon and 1095 (29%) were not offered treatment as symptoms were either below treatment criteria or was contraindicated.
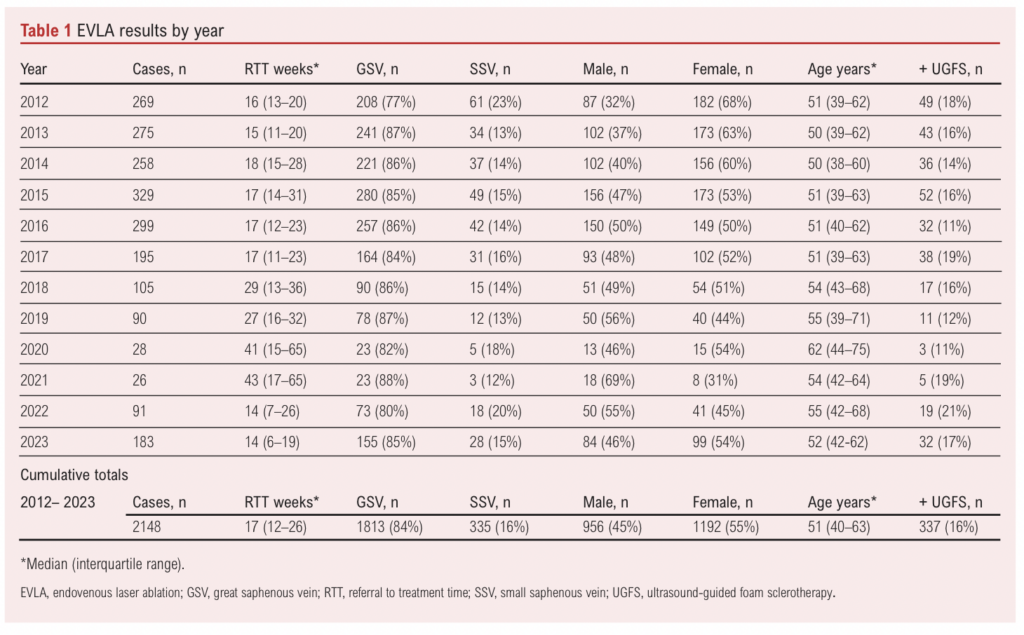
EVLA of the great saphenous vein was performed in 1813 cases (84%) and of the small saphenous vein in 335 cases (16%). EVLA cases included 956 men (45%) and 1192 women (55%) with a median (IQR) age of 51 (40–53) years. UGFS was administered either concomitantly or within 8 weeks of EVLA to saphenous tributaries in 337 cases (16%). EVLA results by year are shown in Table 1.
Median (IQR) time spent per year delivering EVLA was 189 (91–105) hours and delivering outpatient assessment clinics was 108 (105–113) hours, a combined average of 297 hours per year.
Waiting times (RTT)
In 2011, prior to the service being nurse delivered, median (IQR) RTT for this patient group was 53 (45–59) weeks. Median (IQR) RTT across the reported 12-year period of nurse-delivered service was 17 (12–26) weeks, a 68% reduction. Of the 183 EVLA cases performed in 2023, 40 (22%) had active venous leg ulcers; the median (IQR) RTT for this subgroup in 2023 was 7 (3–11) weeks.
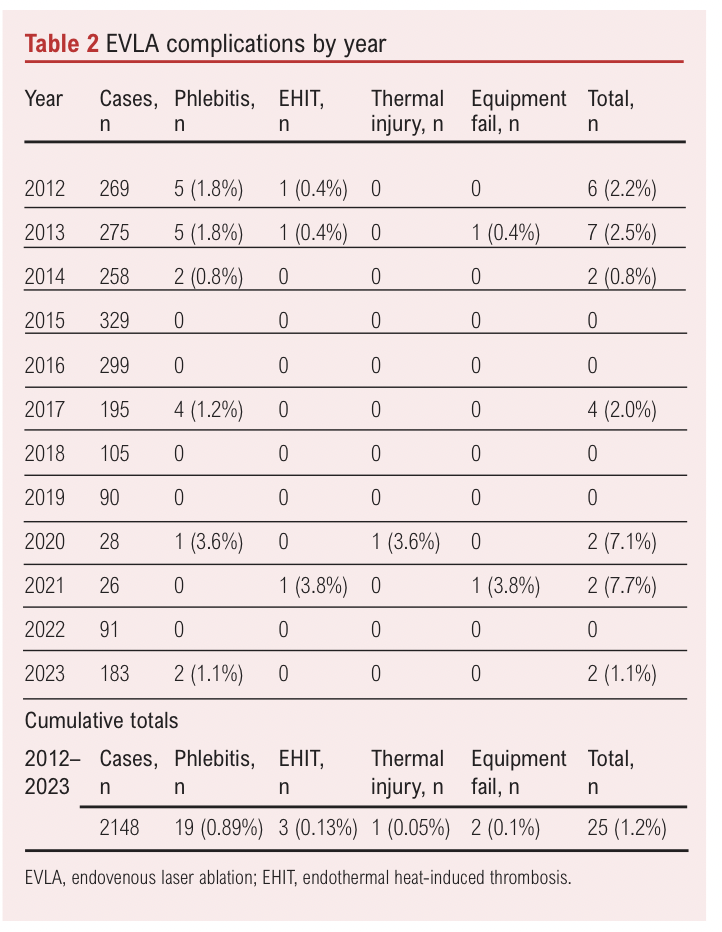
Complications
Complications were recorded for 25 cases (1.2%); these comprised three cases of endothermal heat-induced thrombosis, two intraoperative complications arising from equipment failure, one case of thermal injury and 19 presentations of postoperative superficial thrombophlebitis (see Table 2).
Follow-up and patient satisfaction
In 2012, 40 patients received duplex ultrasound follow-up at 6 months post EVLA and 36 patients were found to have successful vein closure (90%). A further 40 patients were followed up in the same way in 2013, all of whom were found to have successful vein closure (100%).
Patient satisfaction questionnaires were assessed in 2014/2015 and again in 2017/2018; of the 300 questionnaires distributed, 217 responses (72%) were received. Median (IQR) visual analogue pain score for the intraoperative period was 2 (2–3), with median time to full recovery 3 (2–4) days. Median satisfaction score for clinical outcome was 8 (6–8) and with a nurse-delivered service it was also 8 (7–8).
Discussion
The cases described represent a significant workload across the 12-year period. Time spent per year delivering EVLA combined with time spent delivering outpatient assessment clinics released a compelling amount of consultant surgeon time. This is a significant efficiency in a surgical speciality where lack of medical workforce capacity is recognised to be negatively impacting the clinical outcomes of this patient group.16
The types of complications encountered were not unexpected and mirrored those described by other authors outlining EVLA experience.28 Of the complications reported, six were procedural complications occurring during treatment; this is conservatively comparable to the surgeon-delivered EVLA reported in studies such as the CLASS trial (1%).29 However, lack of routine clinical follow-up has almost certainly resulted in under-reporting of postoperative complications, which were far more commonplace at 6 months within the CLASS trial (48.6%).29
Efficacy of vein closure during the initial years of practice was also reassuring and was comparable to several studies reporting closure rates of 93–96% in surgeon-delivered EVLA.30,31 The safety of nurse-delivered EVLA is further demonstrated by patient-reported low intraoperative pain scores alongside high overall satisfaction described in patient feedback.
Early access to both venous assessment and intervention is clearly beneficial to the patient group and is desired by those delivering venous services. RTT data for NHS England has previously been reported over a comparable 12-year period (2006/7 to 2017/18). Average waiting times ranged from 64 to 125 weeks, illustrating the extent of difficulty vascular services are experiencing in the delivery of timely venous assessment and intervention across the largest parts of the UK.1
Waiting times at this single UK centre were positively affected by nurse delivery. Across the reported period, RTT was consistently lower than the peak 53-week RTT recorded prior to this innovation; a 68% reduction in waiting time is a considerable improvement. Predictably, RTT rose significantly during the period of COVID-19 restrictions; however, data show that recovery post restriction was swift. The ability to recover waiting times rapidly post COVID-19 restriction is largely attributable to a nurse-delivered service not having to compete for resources. The VNS has a focused well-defined scope of practice that does not encroach upon other surgeon-delivered activity nor the resources allocated to that activity such as theatre space, time or workforce – barriers to early access identified in post EVRA trial studies.13 Designing a venous service in this way would appear to be a more sustainable method of delivering assessment and intervention to this patient group.
In the time since the EVRA trial was published, the Royal Society of Medicine Venous Forum has published recommendations for the treatment of patients with venous leg ulcers. Their guidance includes the goal of venous intervention delivered within 2 weeks of assessment.21 Through active promotion of early intervention, this nurse-delivered venous service made significant steps toward this goal, managing the VLU subgroup with priority and achieving RTT of 7 weeks in 2023.
Limitations
These data and the narrative describe the development of a venous service in a previously untested and innovative direction. There was no preconception of analysis beyond local audit; as such, this report lacks the rigour of formal research design and methodology.
Clinical follow-up was limited to a small percentage of reported cases (15% in 2012/2013, only 4% of total cases reported). The implication of incomplete follow-up could be overestimation of treatment efficacy and under-reporting of post-procedure complications. Prospective studies should aim to integrate comprehensive clinical follow-up within the study design to avoid the potential risk of study bias and ensure complete reporting of post-treatment complications as a patient-related outcome measure (PROM).
This report would be greatly enhanced by the inclusion of data derived from validated outcome measures of quality of life, PROMs and patient satisfaction/feedback. Evaluation of patients perceived (venous) health before and after treatment would help in the evaluation of VNS-delivered treatment efficacy. Validated tools such as the Aberdeen Varicose Vein Questionnaire and the Venous Clinical Severity Score would be ideally placed to achieve this.32
Impact upon surgical trainees
In 2024 the Association of Surgeons in Training released a joint statement raising concern following the publication of a case series of laparoscopic cholecystectomy performed by a surgical care practitioner.33 Of the three concerns raised, one is pertinent to this report of nurse-delivered venous practice – a worry raised in various forms and forums that nurse-delivered surgeries deprive surgical trainees of training opportunities.
Evidence reporting the impact of nurse-delivered activity upon the development of surgical trainees is lacking. However, factors detrimentally impacting their training in general are well reported. The Rouleaux Club (Vascular Trainees’ Association for Great Britain and Ireland) published a report in 2021 examining stressors resulting in vascular trainees resigning a National Training Number (15% attrition 2013–2019). Of the contributors cited, loss of training opportunities due to nurse-delivered activity or interprofessional task shifting does not feature. Key detrimental factors included impact of geographical relocation, poor work/life balance, unpredictable working hours, fatigue and lack of rest post on-call. Trainees expressed that they did not believe these factors would improve as their careers progressed.34
Within the reporting vascular centre, maintaining the ability to deliver a venous service for the benefit of the patient group was a core service priority; this was severely threatened, predominantly by woefully diminished workforce capacity. Prior to the service being nurse-delivered, surgical trainees rarely had the opportunity to experience EVLA/UGFS due to irregularity of lists and prioritisation of other vascular surgical procedures from the arterial workload. The question that should be asked is: If there is an impact on surgical trainees, does that impact outweigh the detrimental blow to patients who are unable to access venous services and benefit from best practice?
Scarcity of vascular curriculum surgical trainees and subsequent rota pressures contribute heavily to the issue. At the reporting centre there are periods where the vascular unit is without a vascular trainee and the accepted norm is to host but one trainee from the vascular programme per rotation. The VSGBI Vascular Surgery Workforce and Wellbeing Survey 2021 confirms that vascular services in the UK have experienced increases in activity, admissions and waiting lists year-on-year from 2012, with projected increases beyond 2030. The same report shows a UK-wide deficit of both established consultant vascular surgeons and of vascular specialty trainees (29% increase required), consistently increasing activity and consistently too few surgeons and trainees.15 This is not conducive to maintaining the full spectrum of vascular services needed to care for patients. The goal of ‘best practice’ becomes even less attainable when patient ‘demand’ continues to outstrip our ability to ‘supply’ services.
As recruitment to interventional radiology declined and emphasis on endovascular approaches to vascular surgery increased, trainees sought greater access to endovascular training.35 It has been the experience of this reporting centre and VNS that varicose veins and chronic venous disease are rarely a training priority for incumbent vascular surgical trainees. The exception was found to be in the learning of percutaneous access skills to augment arterial endovascular training. These were more easily taught in venous cases, where procedures are of shorter duration, use smaller access devices conducive of early-stage learning and were performed in a more relaxed environment. For this reason, nurse-delivered EVLA had a positive effect on the training opportunities of vascular surgical trainees within the reporting centre. The VNS and regular EVLA list became a fixture in trainees’ educational regimen. The quality and value of this experience should be studied further, as should the overall impact on training opportunities and the real-world experiences of vascular surgical trainees and specialist nurses alike.
Conclusion
A new gold standard of care is emerging in the UK for patients with venous leg ulcers and symptomatic chronic venous disease, delivering improved clinical outcomes through early assessment and early intervention. The potential exists to heal wounds faster and reduce recurrence, improving quality of life and easing the burden placed upon healthcare systems. However, current vascular services have self-identified barriers preventing optimum delivery of this care, including workforce shortage, overall capacity and financial restriction. A greatly increased number of clinicians must be found to deliver venous services if the gold standard is to be achieved and sustained.
Nurse-delivered surgical procedures are far from novel and are well reported across the globe for multiple surgical specialties.19 The data reported suggest that endovenous interventions can be safely performed in the outpatient clinical setting by a suitably trained and mentored VNS and that the patient group can be satisfied and accepting of this innovation.
Given the barriers to service provision described, the increasing UK venous caseload and diminishing medical workforce, there should be ample opportunity for trainee exposure to venous cases regardless of which experienced professional delivers the education.
Multiple UK centres have since developed similar nurse-delivered venous practice. Prospective audit and multicentre research should be undertaken as the evolution of modern sustainable venous services continues. Fostering a culture of inclusivity and cooperation across professions could help to achieve a new higher standard of care for this in-need patient group.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;4(1):33-40
Publication date:
October 30, 2024
Author Affiliations:
Department of Vascular Surgery, Aberdeen Royal Infirmary, Aberdeen, UK
Corresponding author:
Ben Cooper
Vascular Nurse Consultant, Department of Vascular Surgery, Aberdeen Royal Infirmary, NHS Grampian, Foresterhill Health Campus, Cornhill Road, Aberdeen, AB25 2ZN, UK
Email: [email protected]











