ORIGINAL RESEARCH
Open aortic surgical training with trainees as primary operator: a retrospective single-centre analysis
Nortley MC,1 Dixon F,1 Sharma I,1 Lawson JA,2 Rodriguez DU,1 Perkins JMT,1 Wilton E1
Plain English Summary
Why we undertook the work: The UK National Institute for Health and Care Excellence published guidance for unruptured abdominal aortic aneurysms (AAA) recommending vascular specialists “offer open surgical repair unless it is contraindicated because of their abdominal co-pathology and/or medical comorbidities”. Uptake of open AAA repair has since increased in the UK. This has been preceded by over a decade of worldwide endovascular enthusiasm.
What we did: This study reviewed safety outcomes of open aortic surgeries with vascular surgical trainees as the primary operator using retrospective analysis of prospectively accrued data.
What we found: We demonstrate that open aortic surgical training can be provided safely with trainees as primary operator.
What this means: This is paramount for preserving open aortic surgical skills for the vascular surgeons of the future.
Abstract
Objective: To review safety outcomes of open aortic surgeries with vascular surgical trainees as the primary operator.
Methods: A retrospective analysis of prospectively accrued data was performed using our departmental database, electronic patient records and the National Vascular Registry for all elective open abdominal aortic aneurysms (AAA) (juxtarenal and infrarenal) repairs over 2 years between 1 January 2017 and 31 December 2018. Data on primary operator, training level, number of surgeons, assistant training level, operation time, duration of ITU and hospital stay, 30-day mortality, 1-year mortality and complications were obtained.
Results: During the study period 83 elective open AAA repairs were carried out. The primary operator was a trainee in 46% (n=38) and a consultant in 54% (n=45). For trainees and consultants, median operation time was 178 min vs 215 min (p=0.036), duration of ITU stay was 1.5 days vs 2 days (p=0.270), duration of hospital stay was 5.6 days vs 6.8 days (p=0.037), 30-day mortality was 0.0% vs 2.2% (p=0.932) and 1-year mortality was 0.0% vs 2.2% (p=0.932), respectively.
Conclusions: Safe surgical outcomes for open AAA repair can be achieved with vascular surgical trainees as primary operators.
Introduction
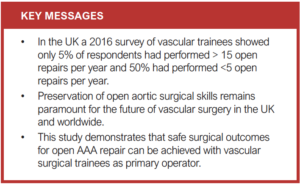
Over the last two decades the popularity of endovascular abdominal aortic aneurysm (AAA) repair (EVAR) has meant that vascular units have begun to express concerns regarding the ability of vascular trainees to acquire open aortic surgical skills. In the USA, EVAR usage has been reported to be >80% in some units.1,2 Trainees’ exposure to open AAA repair has fallen and providing training for open repair is a particular challenge.1-4 UK, US and European data show a worryingly low level of exposure to open repair – in some instances rates of open repair have dropped by 80% during the last decade.5 In the UK, a 2016 survey of vascular trainees showed only 5% of respondents had performed >15 open repairs per year and 50% had done <5 open repairs per year.3 This is echoed by predictive modelling using US national databases which demonstrate a dramatic decline in exposure to open repair amongst vascular trainees.2
In the last few years the vascular community has been presented with compelling evidence regarding the failure of Endovascular Aneurysm Sealing System and the inferior long-term durability of EVAR versus open repair. In the UK, the publication of the National Institute for Health and Care Excellence (NICE) guidance on unruptured AAA is strongly weighted towards open repair.
In the UK, National Vascular Registry (NVR) annual reports show that concerns over the durability of EVAR may be coming to fruition; percentages of EVAR and open surgery for elective AAA repair were 68% and 32% in 2017 but changed to 63% and 37% in 2018 respectively. This indicates a potential increasing need for surgeons with open aortic skills.
Regardless of local practices, acquisition and future retention of open aortic skills is paramount for the vascular community worldwide. Simulation training for EVAR is widely available and effective, but realistic simulation for open repair is more difficult to provide with any proven transference of skills to the operating theatre. Exposure to live cases likely remains the best training available and each opportunity should be maximised with safety as a priority. This is perhaps best achieved in specialist centres, since a recent international observational study of open repairs showed that an annual centre volume of 13–16 open repairs is associated with the most significant mortality risk reduction.6
We present data which examines whether vascular trainees can safely perform supervised open AAA repair as the primary operator. Outcomes are compared against cases where consultant surgeons were the primary operator.
Methods
All elective open juxtarenal and infrarenal AAA repairs performed at Oxford University Hospitals NHS Foundation Trust between 1 January 2017 and 31 December 2018 were identified from three prospective databases. These were a local departmental database, a hospital-wide electronic patient record database and the NVR – a national clinic audit commissioned by the Health Quality Improvement Partnership. All patients gave prospective consent to be included in the local departmental database and the NVR.
Research ethics committee approval was not required for this study as per the UK Health Research Authority Decision tool.7 The local Clinical Research and Trials Governance study classification meeting panel additionally classified this study under service review activity.
Case identification and data analysis was performed retrospectively. For each case the following data points were collected: primary operator (consultant surgeon vs vascular trainee), 30-day mortality, 1-year mortality, major complications, operation time, duration of ITU and hospital stay, number of consultant surgeons present, additional non-consultant assistant present, American Society of Anaesthesiology (ASA) grade and baseline co-morbidities.
The surgeon, consultant or trainee was labelled ‘primary operator’ if they performed a minimum of the exposure of the aorta and the proximal aortic anastomosis. This information was recorded prospectively on the local departmental database according to a locally agreed protocol. Cases with a consultant surgeon as the primary operator were compared with cases where a trainee surgeon was the primary operator. Primary outcome measures were taken as 30-day mortality and 1-year mortality. Secondary outcome measures were duration of ITU stay, duration of hospital stay, major complication rate and operation time.
For categorical data (30-day mortality, 1-year mortality, major complications), a χ2 test was used to perform statistical analysis. For non-categorical data (duration of ITU stay, duration of hospital stay, operation time), a Shapiro–Wilk test was used to assess if data were normally distributed. All non-categorical data were non-normally distributed so a Mann–Whitney U test was used for analysis. A statistical significance level of p<0.05 was used. The statistical software used was OriginPro (OriginLab, 2016).
Using the Clavien–Dindo classification, any complication between grade II (complication requiring pharmacological treatment e.g. pneumonia) and grade V (life-threatening complications) was included as a ‘major complication’.
Baseline co-morbidities were recorded as per NVR categories: none, diabetes, hypertension, ischaemic heart disease (IHD), chronic lung disease, chronic heart failure (CHF), stroke, cancer, chronic renal disease and lower limb arterial disease. These were then subclassified into cardio-respiratory disease (IHD, lung disease or CHF) and hypertension, and the presence or absence of these were compared. Additionally, ASA grade was recorded and compared for each group.
Results
Baseline characteristics
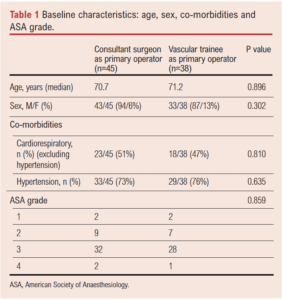
There was no significant difference in age, gender, baseline co-morbidities or ASA grade between patients operated on by a consultant surgeon and those with a vascular trainee as primary operator (Table 1).
Study results
Of 83 elective open AAA repairs, the primary operator was a consultant in 54% (n=45) and a trainee in 46% (n=38). The study centre had an adjusted in-hospital mortality rate for elective AAA repair of 1.4% for the year 2017 and of 1.3% for 2018. This was lower than the national average published rates of in-hospital mortality, which was 3.2% in 2017 and 2018 according to the NVR Annual Report 2018/2019.8,9
Primary outcome measures
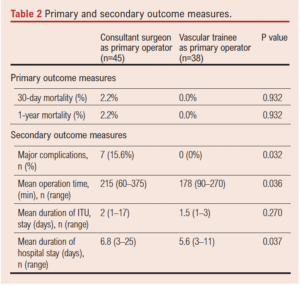
There was no statistical difference in 30-day mortality or 1-year mortality for patients operated on by a consultant surgeon or a trainee surgeon (2.2% and 0.0%, respectively, p=0.9), as shown in Table 2.
 Secondary outcome measures
Secondary outcome measures
Mean operation time was shorter for cases performed by a trainee surgeon (178 min) than for those performed by a consultant surgeon (215 min) (p=0.036). The rate of major complications was higher in patients who had a consultant as primary operator than in those who had a trainee as primary operator (15.6% vs 0.0%, p=0.03). There was no difference in the duration of ITU stay but overall hospital stay was longer in patients who had a consultant surgeon perform their surgery (6.8 days vs 5.6 days, p=0.002), as shown in Table 2.
Further characteristics and complexity
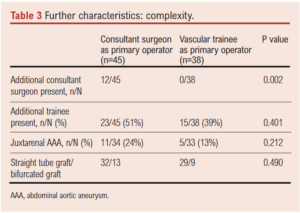
Out of a total of 83 elective open repairs, 12 (14%) had two consultant surgeons present with a consultant surgeon as primary operator. Where a trainee surgeon was the primary operator (46%), they were uniformly supervised by a single consultant surgeon. As shown in Table 3, there was no difference in the frequency at which an additional trainee was present for either group. There was no apparent difference in the frequency of juxtarenal repairs or bifurcated graft repairs in the consultant group compared with the trainee group.
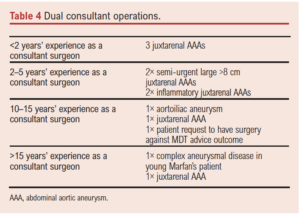
Of the 12 open repairs with two consultant surgeons present, these were examined in more detail regarding case complexity and attending seniority. Further details are outlined in Table 4.
Discussion
All trainees operating within this study would have completed a minimum of two ‘foundation years’ of training followed by two ‘core surgical training’ years. In the UK, surgical trainees then progress to a 6-year specialist surgical training programme. Trainees within this study would have been within years 1–6 of specialist vascular surgical training. A consultant surgeon was always present – either scrubbed into the operation or in the same theatre room. The level of independence was tailored to the seniority and experience of the trainee and at the discretion of the supervising consultant surgeon. All operative planning and intraoperative decision making were discussed with the supervising consultant surgeon.
Our results suggest that open repair can safely be performed by trainees as primary operator when cases are selected carefully and appropriately. Primary outcome measures of 30-day and 1-year mortality were comparable. All complications occurred within the consultant group. This and a shorter operation time and duration of hospital stay in the trainee group may reflect selection of the easier cases assigned to the trainees. However, it is likely that trainees also had the advantage of an experienced consultant surgeon assisting them throughout the open repair, which likely reduces operative time. Whilst the results did not reach statistical significance, consultants performed more juxtarenal open repairs than the trainees (24% vs 13%).
It is acknowledged that this study primarily examines the technical safety of trainees being primary operator. The degree of operative planning and intraoperative decision making by the trainee is difficult to define and measure within the realms of this study, and will have varied with the seniority of the trainee.
There was a second consultant present in theatre in significantly more consultant cases (27%) than trainee cases (0%), which again reflects increased case complexity (see Table 4). All trainee cases were supervised by a single consultant surgeon.
Underlying co-morbidity does not seem to have played a part in case selection as there were no significant differences in baseline co-morbidities or ASA between the two groups. The number of tube versus bifurcated graft repairs was the same between the trainee and consultant groups.
A recent US study analysed data from a major US vascular centre which indicated that, whilst numbers of EVAR and fenestrated EVAR (FEVAR) had remained stable, the numbers of open repair in this major centre had increased over recent years – presumably through quaternary referrals.9 Regardless, the same study reported that “on average, graduating vascular surgery trainees performed 23.1 open repairs before graduation (range 19–26)’’ – more than the reported US national average of 1–3.2 The UK vascular training guidelines have recently changed. It was previously stipulated a minimum number of 10 open repairs performed at level 4 is required to obtain the certificate for completion of training. Level 4 was defined as “able to perform the procedure fluently and without guidance or intervention’’ and “able to anticipate, avoid and/or deal with any common problems/complications”. This changed in August 2021 with an outcomes-based “multi-consultant report” system for set training domains. A total of 10 open repairs are now required showing progression to a minimum of four open repairs at level 4. Level 4 has a new definition: “that expected of a new consultant” with the previous level 4 definition now defined as level 5. To achieve this, each training opportunity for open repair must be maximised.
The authors of the US study suggested centralisation of open repair to centres of excellence in open repair, with trainees completing specialist placements as a strategy to preserve open repair training nationally.10 In the UK, vascular services are currently modelled on a ‘hub and spoke’ regional service system. The current centre is in the top third nationally in terms of volume of AAA repairs.8,9
An alternative approach is a training strategy where single cases are shared between trainees.10 Indeed, in the current study centre, open repair is considered in ‘training stages’ whereby a trainee can incrementally progress from closure, exposure, distal anastomoses, proximal anastomosis and whole procedure. The final training stage allows the trainee to perform the whole procedure with the assistance of a more junior trainee with the attending trainer unscrubbed but within theatre. Towards the end of their training, more senior trainees are also assisted by their consultant trainers in performing open repair in stable patients with ruptured AAAs. Whilst this is not necessarily a new or unique approach to training, in recent years trainees have had increasingly limited exposure to open repair, particularly as the primary operator.3 This strategy may help to maximise training opportunities, particularly if open training becomes centralised.
Overall, the current study demonstrates that safe surgical outcomes for open AAA repair can be achieved with vascular trainees as primary operators when cases are selected appropriately. Preservation of open aortic surgical skills remains paramount for the future of vascular surgery in the UK and worldwide. We propose trainees as primary operators for open repair as a training model, within the context of an incremental training plan, as a strategy for preserving open aortic surgical skills for the vascular surgeons of the future.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(3):84-88
Publication date:
May 10, 2022
Author Affiliations:
1 Thames Valley Vascular Network, Vascular Surgery Department, Oxford University Hospitals NHS Foundation Trust, John Radcliffe Hospital, Headley Way, Oxfordshire, UK
2 St Mary’s Hospital Paddington London, Imperial College NHS Trust London, Vascular Surgery Department, London, UK
Corresponding author:
Ms Mei Nortley
Thames Valley Vascular Network. Vascular Surgery Department, Oxford University Hospitals NHS Foundation Trust, John Radcliffe Hospital, Headley Way, Oxfordshire OX3 9DU, UK
Email: [email protected]











