ORIGINAL RESEARCH
Standards of radiation protection amongst UK vascular surgeons: a clinician’s perspective
Sritharan K,1 Sheikh Z,2 Saratzis A,3 Lakshminarayan R,4 Garnham A,5 Bowbrick G,6 Morgan RA,7 Carradice D8
Plain English Summary
Why we undertook the work: With increasing numbers of procedures in vascular surgery being performed by ‘keyhole’ techniques which require the use of ionising radiation (x-rays), vascular surgeons are being exposed to more radiation throughout their careers compared with 30 years ago. Excessive exposure to radiation can cause cancer and is related to other health problems such as cataracts and skin conditions. This survey looks at the awareness amongst vascular surgeons regarding radiation protection measures, the availability of personal equipment which would help minimise their radiation exposure and whether their employer effectively measures their exposure to radiation, as required by law.
What we did: To address the above questions, we conducted a survey of trainees in vascular surgery and consultant vascular surgeons in the UK. The survey contained 37 questions and was sent out online over a 6-week period, with the responses collected using the survey server SurveyMonkey and analysed.
What we found: This survey highlights a concerning lack of knowledge regarding radiation protection amongst the vascular surgical workforce, poor access to personal radiation protection and failures in monitoring an individual’s exposure to ionising radiation.
What this means: The survey supports the urgent need to address training in radiation protection, improve access to personal equipment such as lead gowns and lead glasses, and for employers to better monitor an individual’s exposure to radiation. This is necessary to protect the workforce against the potentially life-threatening effects of radiation.
Abstract
Objective: To evaluate training in radiation protection, knowledge of local policies and current practices regarding safe working with ionising radiation in vascular surgery units across the UK. Methods: A validated 37 question online survey was distributed to vascular surgery trainees (VTs) and consultants (VCs) by the Vascular Society of Great Britain and Ireland (VSGBI), British Society of Endovascular Therapy (BSET) and Rouleaux Club through their national mailing lists between March and May 2024. Responses were collated using the survey server SurveyMonkey. Results were summarised using descriptive statistics and appropriate tests.
Results: Ninety-one VCs and 87 VTs, representing approximately 15% and 44% of the UK VC and VT workforce, respectively, responded. In total, 94% of VCs and 97% of VTs expressed concerns over the effects of ionising radiation on their health; 91% of VCs and only 74% of VTs had undergone formal radiation safety training. Of these, only 18% of VCs and 43% of VTs had undergone training within the last two years. Overall, 34% of VCs and most VTs (75%) did not know who their local radiation safety officer was; 4% of VCs and 32% of VTs (p<0.001) were completely unaware of local radiation safety policies. A total of 13% of both were not aware of ‘As Low As Reasonably Achievable’ (ALARA) principles, with 20% of VCs and 35% of VTs failing to consistently employ them. Custom-made or retrofitted lead gowns were accessible to 55% of VCs but only 2.4% of VTs (p<0.001). Radiation protection glasses were worn by 52% of VCs compared with 16% of VTs (p<0.001). 84% of VCs were allocated a dosimeter versus only 44% of VTs (p<0.001). Most VCs (76%) and VTs (86%) believed that their employer should prospectively record their annual radiation exposure into a National Registry. A total of 86% of VCs and 96% of VTs agreed that employers should record their cumulative radiation exposure during their entire working life. One in four VCs and VTs experienced a health condition potentially related to their work with ionising radiation. Musculoskeletal pain was the most common, prevalent in 17% and 18% of VCs and VTs, respectively. Overall, 2% of VCs had a malignancy and 5% cataracts. Almost all VCs (94%) and VTs (96%) agreed that these illnesses should be recorded in a national registry.
Conclusion: This survey highlights significant and concerning deficiencies in knowledge, access to personal radiation protection and failures in monitoring individual exposure to ionising radiation amongst the UK vascular surgical workforce.
Background
The rapid evolution of endovascular technologies over the past 30 years has driven an exponential rise in the number of x-ray guided minimally invasive procedures undertaken by clinicians, including vascular surgeons, interventional radiologists, angiologists and cardiologists. In the UK approximately 60% of all aortic cases are performed endovascularly1 compared with just 1% in 2001; and from 2000–2005 to 2015–2019 there was a 46% rise in peripheral endovascular procedures performed in the NHS.2 As a result, clinicians are exposed to ionising radiation earlier in their training and far more frequently throughout their careers. Occupational exposure to ionising radiation is associated with an increased risk of malignancy, predominantly left-sided brain tumours,3 breast cancer,4 skin cancers, leukaemia5 and thyroid cancer.6,7 Regular exposure has also been linked to an increased risk of benign conditions such as cataracts,8 musculoskeletal pain due to ill-fitting lead gowns, dermatitis and hair loss.9
Personal protective equipment (PPE), which includes well-fitted lead gowns with axillary shields, eye protection, thyroid and leg shields, can greatly reduce the radiation exposure to operators. Monitoring radiation doses and maintaining accurate records will ensure that annual recommended levels of exposure to ionising radiation are not exceeded. Additionally, access to a modern hybrid operating theatre and adherence to ‘As Low as Reasonably Achievable’ (ALARA) principles further reduces the radiation exposure to operators.
This survey aimed to evaluate training in radiation protection and knowledge of local policies. It also seeks to review current practices regarding safe working with ionising radiation and understand concerns regarding ionising radiation-linked health conditions amongst the UK vascular surgical workforce.
Methods
This online cross-sectional survey was aimed at vascular surgeons in the UK. The questionnaire was designed by a group of consultant vascular surgeons with input from interventional radiology and orthopaedic surgery colleagues. The questionnaire was pre-tested and validated for content and construct by three vascular surgeons, one interventional radiologist and three orthopaedic surgeons (see Appendix 1, online at www.jvsgbi.com, for the complete survey).
The survey was divided into eight parts – namely, specialty, ionising procedures performed, demographic data, beliefs and values, training in radiation protection, strategies employed to reduce ionising radiation exposure, access to personal protection and injuries potentially associated with working with ionising radiation – comprising 37 questions. There was a mixture of open and closed questions and all closed questions were mandatory. All responses were anonymised.
There are an estimated 600 consultant vascular surgeons and 200 trainees in vascular surgery in the UK. Invitations to complete the survey were sent via email by the Vascular Society of Great Britain and Ireland (VSGBI), British Society of Endovascular Therapy (BSET) and the Rouleaux Club through their national mailing lists.
The survey was administered, and the responses collated by the survey server SurveyMonkey over a 6-week period from March 2024 to May 2024. There were no set exclusion criteria, but only the responses of trainees, fellows and consultants working in vascular surgery were considered for analysis. The results were fully anonymised and analysed using Stata 18.0 and Pearson’s χ2 test was used to evaluate differences in categorical data between groups.
Results
Demographics
The survey was completed by 91 vascular consultants and 87 vascular surgery trainees, representing approximately 15% and 44% of the UK consultant and trainee workforce, respectively. Of all consultant respondents, 82% reported biological sex, the majority (83%) identified as male. Whilst fewer trainees reported biological sex (60%), a greater proportion of those who responded were female (42%) (p<0.05).
Procedures performed
Endovascular aneurysm repair was the most performed procedure by consultant (99%) and trainee (100%) vascular surgeons. Trainees were more likely to be involved in complex aortic cases than consultants: thoracic endovascular aneurysm repair (68% versus 62%), fenestrated endovascular aneurysm repair (72% versus 55%) and branched endovascular aneurysm repair (53% versus 39%).
Most consultants performed iliac (87%) and lower limb endovascular revascularisation (82%) procedures. A greater proportion of trainees undertook iliac (94%) and lower limb (97%) angioplasty; more trainees (31%) were involved in deep venous interventions compared with consultants (19%).
Attitudes towards risk and training
Most consultants (94%) expressed concern over the effects of ionising radiation on their health, with 63% either very concerned or extremely concerned. The majority (91%) had undergone formal radiation safety training in the form of a face-to face (72%) or e-learning (66%) course. However, more than a third (35%) had received their training over five years ago and 9% had undergone training over 10 years ago. Only 18% had undergone training within the last two years.
Almost all trainees (97%) expressed concern about the effects of ionising radiation on their health; 67% were either very concerned or extremely concerned. However, only 74% of trainees had undergone formal radiation safety training and, of these, only 43% had undergone training within the last two years. Most training was in the form of an e-learning course (87%).
Awareness of local policies
Questions regarding awareness of local radiation policy were answered by 99% and 97% of consultants and trainees, respectively. Just over a third (34%) of consultants did not know who their local radiation safety officer was and half (50%) had never met them. Most trainees (75%) did not know who their local radiation safety officer was and the same number had never met them. Trainees (32%) were far more likely to be completely unaware of their local radiation safety policy compared with consultants (4%) (p<0.001). Moreover, 56% of consultant respondents and 83% of trainee respondents were either not aware or only somewhat aware of local policy regarding working with radiation during pregnancy.
Methods to reduce radiation exposure
Of those who answered (97%), 88% of consultant respondents were aware of ALARA principles. The majority (80%) either always or almost always employed ALARA strategies to minimise radiation exposure during endovascular cases. The most common practice employed by consultant operators to reduce exposure was shielding (91%) and keeping detectors close to the patient (90%). Minimising the use of digital subtraction angiography (DSA) (81%), reducing the frame rate of DSA acquisition (70%) and increasing the distance between the operator and C-arm during DSA (88%) were also frequently employed practices. Other strategies included awareness of C-arm angulation (83%) and, to a lesser extent, minimising the use of magnification (69%). Single use radiation protection shields (RADPAD®) were routinely employed by only 32% of consultant operators.
Of those trainees who responded (93%), 87% were aware of ALARA principles and 65% either always or almost always implemented them. Shielding (78%) and keeping the detector close to the patient (75%) remained the most frequently used strategy to reduce exposure but was overall less frequently used amongst trainee operators than consultant operators. Minimising the use of DSA (73%) and stepping away during DSA acquisition (79%) were also common; however, reducing the use of magnification (41%) and reducing the frame rate of DSA acquisition (54%) were less common.
Personal protective equipment (PPE)
Lead gowns
Custom-made or retrofitted lead gowns appropriate for build and gender were accessed by just over half (55%) of consultant respondents. Trainees were significantly less likely to have access to custom-made or retrofitted lead aprons (2.4%) (p<0.001) than consultants and only 3.8% of trainees versus 15% of consultants (p<0.05) had been measured or advised which lead gown available from the rack they should wear.
Over half (58%) of consultant respondents reported that their personal or departmental lead gowns were inspected annually for cracks. However, over a third (36%) were unsure. Only 10% of trainees reported that that their personal or departmental lead gowns were inspected annually; the vast majority (83%) were unsure.
Thyroid collars, eye protection, leg shields and lead caps
Thyroid collars were used by the majority of consultants (93%) and trainees (95%). However, radiation protection glasses were used less frequently (52%) by consultant operators. Of those who did not always wear radiation protection glasses, 41% reported not being provided with them. The use of radiation protection glasses was significantly less (16%) (p<0.001) amongst trainees. For those who did not wear protective glasses at all times, 39% did not have access to them.
Questions on the use of leg shields and lead caps were answered by 93% of consultants and 92% of trainees. Leg shields were used by only a small number of consultants (18%) and trainees (13%). Of the remaining consultants and trainees, 41% and 63%, respectively, had not been provided with them. Similarly, only a small number of consultants used a lead cap (4.7%); of those who did not, 36% had not been provided with them. Only one trainee reported using a lead cap, 50% of the time; 65% of all trainees reported not being provided with them.
Difficulties in accessing PPE
Trainees (38%) were more likely to be denied access to eye protection than consultants (32%). Moreover, trainees were more likely to have not asked for eye protection (56%) than consultants (25%) (p<0.001).
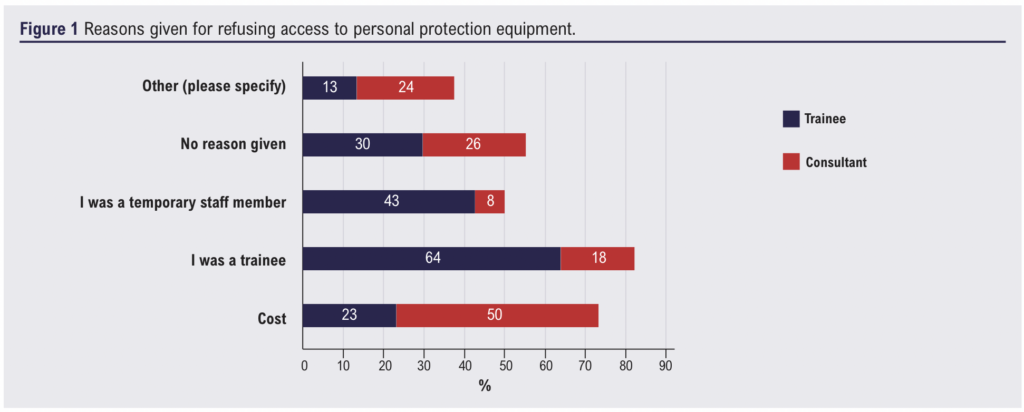
Trainees were also more likely to be denied access to custom-made or retrofitted lead gowns (63%) than consultants (27%) (p<0.05). Additionally, trainees were more likely (63%) to have not asked for this PPE compared to consultants (33%) (p<0.001). The most common reasons given to trainees for refusal (n=61) was that they were a trainee (64%) or temporary staff (43%). Of those consultants who reported reasons for refusal (n=66), cost was the most common reason given (50%) (see Figure 1).
Monitoring dose exposure
Questions regarding dose monitoring were answered by 95% and 92% of consultant and trainee respondents, respectively. The majority of consultants (84%) had been allocated a personal dosimeter and 72% wore these at all times. However, of those who also worked at remote sites, only 36% had a dosimeter allocated at these sites. Trainees were significantly less likely to have a personal dosimeter allocated (44%) (p<0.001) and only 28% wore these at all times. Of those trainees who travelled to remote sites, only 5.6% had a personal dosimeter allocated at this site. Furthermore, trainees were significantly less likely (3.8%) than consultants (41%) to have ever been given feedback on their dose exposure (p<0.001).
Real-time dosimetry has been shown to be effective in reducing overall operator dose exposure. However, only 7.0% of consultants consistently employed this. Of those consultants who did not, 48% did not have access to this. Only 3.8% of trainees reported consistent use of real-time dosimetry and, of those remaining, 68% did not have access.
Access to a hybrid operating room (OR)
Of all consultants (97%) and trainees (94%) who answered the questions regarding availability of a hybrid operating room (OR), the majority (68% and 73%, respectively) used a hybrid OR for both elective and emergency cases. 88% of all consultants had at some point requested a modern hybrid OR; 41% of these consultants reported having this request denied.
Monitoring compliance
Of all consultants (92%) who answered the question surrounding compliance, less than half (40%) agreed that their Trust accurately monitored their compliance to nationally legislated dose exposures; of these, 8% strongly agreed. Although fewer trainees responded to this question (84%), trainees were significantly less likely to agree than consultants that their Trust accurately monitored their dose exposures (only 8.2%) (p<0.001). Trainees were far more likely to strongly disagree (48%) that Trusts accurately monitor their compliance compared with consultants (13%) (p<0.001).
Most consultants (86%) agreed or strongly agreed that employers should record cumulative radiation exposure during an operator’s entire working career compared with almost all trainees (96%). Additionally, the majority of consultants (76%) and trainees (86%) agreed that employers should prospectively record and centrally upload annual radiation exposure to a national registry. Only 23% and 12% of consultant and trainee respondents, respectively, felt that the radiation protection afforded to healthcare professionals was adequate.
Incidence of workplace radiation exposure-related health problems
Around one in four consultants (25%) and trainees (23%) who responded had experienced a health condition potentially associated with their work with radiation. Musculoskeletal pain was the most common, prevalent in 17% and 18% of consultants and trainees, respectively. Of consultant respondents participating in this survey, 2% had experienced a malignancy (one basal cell carcinoma and one parathyroid adenoma), 5% reported radiation-induced eye disease and 7% reported skin conditions such as hair loss and dermatitis. Of the trainee respondents, one trainee reported a malignancy and 8% skin conditions. Notably, 37% of trainees and 60% of consultants knew of someone with a potentially radiation-associated condition. Almost all consultants (94%) and trainees (96%) agreed or strongly agreed that all potentially radiation-associated illnesses amongst radiation workers should be captured within a national registry.
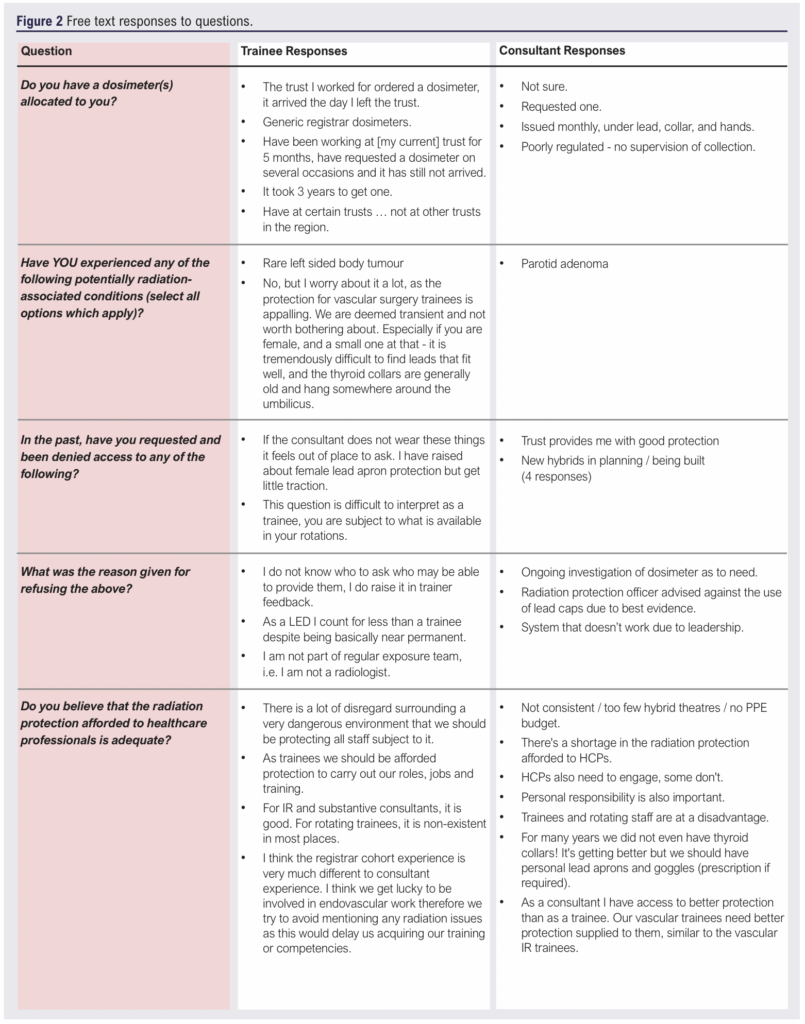
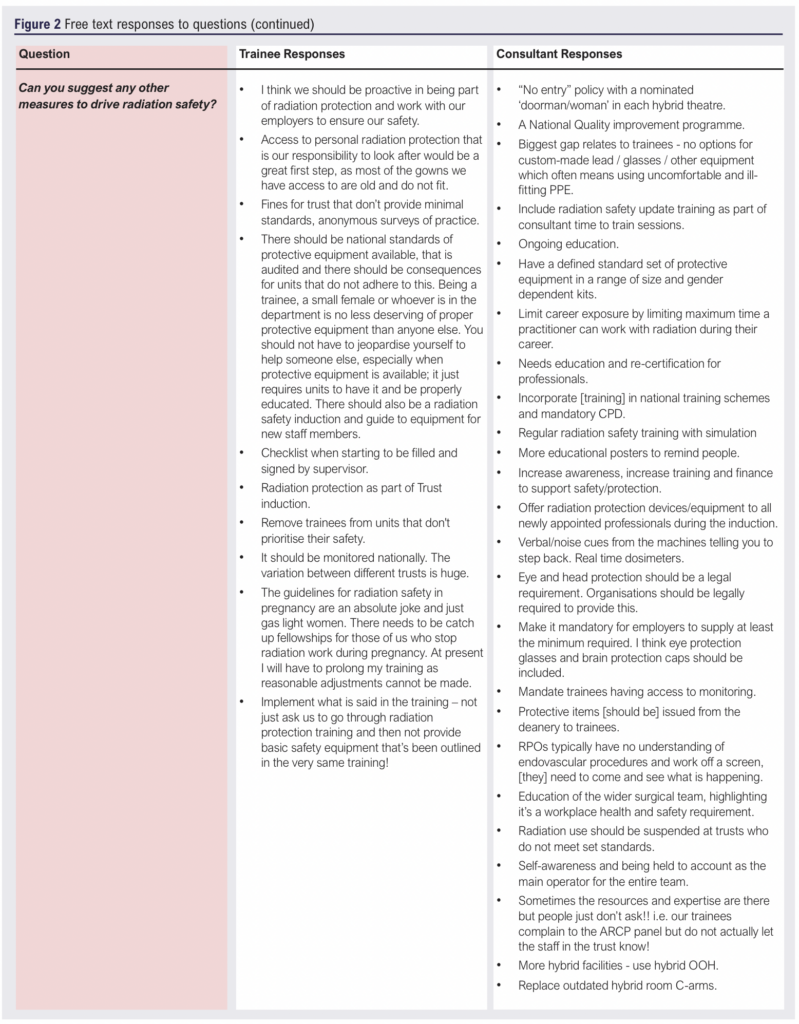
The free text comments from this survey are collated in Figure 2.
Discussion
The employer has a legal obligation to minimise the extent to which employees are exposed to ionising radiation by providing systems of work which restrict exposure to ionising radiation and through the provision of adequate and suitable PPE. Employers are also legally compelled to ensure that all practitioners are adequately trained for their role and undertake continuous education and training; and monitor, record and maintain records relating to an individual’s radiation exposure.10
Surgeon education has been shown to decrease the overall radiation dose in complex endovascular procedures11 and trainees who feel their consultants consistently practise ALARA strategies are more likely to do so themselves.12 In this study 26% of trainees and 9% of consultants either did not or did not recall having training in radiation safety. Moreover, nearly half of all consultants (44%) and 57% of trainees undertook their training more than five years ago and two years ago, respectively. This would partly explain why 13% of trainees and consultants were not aware of ALARA principles with approximately 6% of trainees and consultants never or almost never employing this in their endovascular practice. The International Commission on Radiological Protection (ICRP) makes specific recommendations that training should be initiated at the start of a career (ie, during medical school) and that specialty- and role-specific training should continue during training.13 Once training is completed, it should be updated at least every 36 months. Training in radiation protection in the UK clearly falls far short of these standards.
Whilst the majority of the vascular workforce did have access to a hybrid OR in this survey, 32% of vascular consultants and 27% of vascular trainees did not, and this is despite evidence of lower patient radiation doses, shorter screening times, and less contrast use with a hybrid OR compared to a conventional OR with a mobile C-arm.14 Those units without access to a hybrid OR are in the minority and fall outside the Provision of Vascular Services 2021 recommendation that all arterial centres should provide, as a minimum, a 24/7 hybrid OR.15
This survey also highlights the poor access to personal radiation protection experienced by the vascular workforce and shows a significant difference between the personal protection afforded to vascular surgery trainees compared with consultants, with only 2.4% of trainees having access to custom-made or retrofitted lead gowns compared with 55% of consultants. Poor access to PPE and a lack of dose monitoring has also been reported amongst interventional radiology trainees.16 As endovascular techniques advance, trainees are more likely to be exposed to ionising radiation earlier and for longer in their careers. Moreover, the trainee cohort in this survey comprised of significantly more female operators than the consultant cohort. Ill-fitting lead gowns can leave large amounts of the body unprotected, specifically radiosensitive areas such as breast tissue,4 hence the updated recommendation by the European Society of Vascular and Endovascular Surgery (ESVS)9 that all female operators should have lead gowns with axillary supplements and sleeves to reduce the risk of breast cancer. This study demonstrates that the UK is a long way from achieving this goal.
ESVS radiation protection guidelines also recommend that operators always wear appropriately fitted lead glasses during radiation-guided procedures.9 However, only 16% of trainees and 52% of consultants consistently used lead glasses in this survey, with one in five consultants and approximately one in three trainees not having access to them. The survey highlights both a gross failing by the employer to provide the workforce with adequate radiation protection as well as poor compliance in utilising certain PPE, and this should be urgently addressed.
Whilst exposure to high doses of ionising radiation has long been known to be harmful, it is increasingly apparent that long-term exposure to low-dose ionising radiation is also harmful.9 However, over half of the vascular surgery trainees in this survey and almost one in five consultants did not have access to a personal dosimeter, meaning that neither the annual safe level nor the cumulative lifetime radiation exposure was being recorded in these clinicians. A study of vascular surgery trainees in the United States demonstrated that excess radiation exposure in trainees was more prevalent than anticipated, with multiple trainees exceeding annual radiation dose limits.17 Moreover, less than half of all consultants and only 4% of trainees received feedback regarding their dosimeter readings, again representing a missed opportunity to engage the workforce and potentially improve radiation safety.17
One in four vascular consultants and trainees experienced a health condition potentially related to their work with ionising radiation, but this can only be inferred as dose data and worker classification information was not collected in this survey but, more importantly, would not have been available for the majority of respondents. Musculoskeletal pain was the most common, prevalent in 17% and 18% of vascular consultants and trainees, respectively. The prevalence of back pain amongst the trainee cohort is more than four times higher than the age-matched background population.18 However, the prevalence of back pain in consultant operators, who are more likely to have custom-made leads, was similar in prevalence to the background population. Well-fitted lead aprons in trainees may therefore help mitigate against the development of back pain.
Of concern, 2% of vascular consultants had experienced a malignancy, 5% reported radiation-induced eye disease and 7% of consultants and 8% of trainees had developed skin conditions. A national database of the incidence of potential radiation-linked health conditions across all groups working with ionising radiation in healthcare would help identify areas where radiation safety could be enhanced, noting that our understanding of the impact of ionising radiation on healthcare professionals and patients is continually growing. There was strong support for this approach from respondents in this survey.
Across both consultant and trainee groups there was also strong support for a national registry to monitor annual and lifetime occupational radiation exposure. This would potentially help strengthen the governance surrounding the monitoring, documentation and feedback of annual and lifetime dosimeter readings. In order for a registry of this nature to be effective, compliance with monitoring and the use of PPE is essential. This survey reports poor compliance as well as the lack of provision of PPE and monitoring. The former is interesting given the level of concern expressed by clinicians, and perhaps is a reflection of poor education and awareness.
The main limitation of this study was the small sample size, particularly in the vascular consultant cohort where 15% of the workforce was represented compared with 44% of the vascular trainee workforce. Responder bias could also not be excluded and those more concerned about radiation protection may have been more likely to respond. If this is the case, then the problems highlighted may be far greater than reported in this survey. In addition, there was a greater proportion of female respondents in the vascular trainee group compared with the consultant group. This may be due to apprehension amongst female trainees regarding the higher incidence of breast cancer reported in US orthopaedic surgeons compared with the general US female population,4 or fears surrounding radiation protection during pregnancy.
Conclusion
This survey highlights significant deficiencies in knowledge, access to personal radiation protection and failures in monitoring individual exposure to ionising radiation amongst the vascular surgical workforce in the UK. Moreover, trainees are more likely to struggle to access radiation protection equipment compared with their consultant colleagues. The data emphasise the failings by the employer to meet its legal obligations and the urgent need in the UK to improve standards for healthcare professionals working with ionising radiation by improving access to personal radiation protection, developing more robust training pathways and improving the governance surrounding the monitoring of exposure to ionising radiation.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;4(1):25-32
Publication date:
November 25, 2024











