ORIGINAL RESEARCH
Tenotomy for diabetic foot ulcers: a scoping survey of current practice
Hitchman L, Nandhra S, Gooday C, Cowan A, Bowling F, Nixon J, Pickard J, Cohen J, Atkin L, Rudarakanchana N, Collings R, Kavarthapu V, Shalhoub J, Games F, Russell D*
Plain English Summary
Why we undertook the work: Diabetes is very common and one of the major problems is foot ulcers. Many foot ulcers fail to heal. Tenotomy describes cutting tight foot tendons to redistribute pressure in the foot. This may help ulcers heal faster and stop them coming back. This study aims to see who uses tenotomy and how it is performed.
What we did: The study was an online survey of doctors, nurses, podiatrists and any other person involved in treating patients with diabetic foot ulcers. The study collected information on how they treat patients and if they were interested in taking part in further research.
What we found: One hundred and sixty-eight healthcare professionals completed the survey: 111 were surgeons, 48 were podiatrists and 9 were diabetes specialist doctors. There were three scenarios in which tenotomy was offered: to reverse toe deformity, to aid ulcer healing and to prevent recurrence. Tenotomy was often performed by orthopaedic surgeons (76%). The frequency with which tenotomy was performed varied from monthly (48%) to yearly (21%). The method of undertaking tenotomy varied. Some centres perform tenotomy under local anaesthetic (51%) whereas others perform it under a general anaesthetic (6%). Surgical tenotomy was the most preferred method (68%). Prior to tenotomy there was variable assessment of blood supply to the foot and 7% of centres did not assess blood supply at all. Eighty-three responders would like to take part in further research to further investigate tenotomy and other pressure relieving treatments in the diabetic foot.
What this means: There is variation in the reason that tenotomy is performed, pre-procedure assessment prior to tenotomy and the way tenotomy is performed. Clinicians responding to this survey are willing to take part in more research in tenotomy. The Vascular Society Specialist Interest Group in the Diabetic Foot will lead further research in this area.
Abstract
Background: Diabetes mellitus is one of the fastest growing health crises of our time. One of the major complications is diabetic foot ulcers, many of which fail to heal. Tenotomy – transection of tendon fibres – may help to redistribute pressure in the foot and therefore help ulcer healing and prevent recurrence. The aim of this survey was to explore the availability of pressure relieving adjuncts, including tenotomy, in diabetic foot services and interest in collaborating in further research studies.
Methods: An online survey was performed of healthcare professionals involved in the management of diabetic foot ulcers to explore the multidisciplinary composition of diabetic foot services, offloading therapies available and interest in collaborating in further research.
Results: The survey gained 168 responses from 10 countries. Most responders were orthopaedic surgeons (61.3%, 103/168). Of those who responded, 70.8% (119/168) had a dedicated diabetic foot clinic and 99 (58.9%) reported having an active tenotomy service. 73.8% (124/168) of responders wished to further collaborate and 82.1% (138/168) were willing to help involve their patients in a future trial.
Conclusions: The results of this survey showed the variation in tenotomy practice and an appetite for collaborative research in this area. The Vascular Society of Great Britain and Ireland Diabetic Foot Specialist Interest Group will address these uncertainties through targeted collaborative research to investigate tenotomy as a potential clinical and cost-effective treatment in diabetic foot care.
Introduction
Diabetes mellitus is one of the fastest growing health crises of our time. The disease is endemic in the UK, currently affecting more than 4.9 million people.1 Diabetic foot ulcers (DFU) are a common and difficult-to-treat complication of the disease. Over a quarter of patients with diabetes will develop a DFU. Even with current best ulcer care implemented by a multidisciplinary team (MDT) following evidence-based guidelines, less than 50% of patients heal within the expected time frame.2 Delayed healing leads to hospitalisations, life threatening infections, limb loss and mortality. This has a huge impact on patient quality of life and healthcare resources.
To tackle this health crisis, the Vascular Society of Great Britain and Ireland set up the Diabetic Foot Specialist Interest Group (DF-SIG), consisting of expert healthcare professions in DFU, vascular trainees and – importantly – patients, to address specific challenges facing patients, clinicians and healthcare systems through focused research. Foot complications of diabetes including infections, ulceration and amputation were identified in five of the top 10 clinician research priorities,3 and a collaboration with the James Lind Alliance exercise has identified joint patient-reported research priorities.4 The DF-SIG analysed key themes identified by patients and found new treatments to help DFU healing and prevent ulceration were the most frequently recurring themes.
DFUs occur due to a combination of factors, including peripheral neuropathy. Peripheral neuropathy is particularly problematic as it results in typical cavoid foot deformities such as claw and hammer toes. When combined with the loss of protective sensory feedback, this malposition causes increasing pressure on weight-bearing areas, predisposing patients to ulcer formation.
Conservative measures to treat these ulcers include offloading casts and below knee walker boots. However, these do not correct the biomechanical deformity in the long term, predisposing to ulcer recurrence, and are poorly tolerated by patients. Tenotomy describes the transection of the tendon fibres and, in this context, relates to the flexor or extensor tendons of the toes. It is a minimally invasive procedure that can correct toe deformities to improve DFU healing and prevent recurrence.5
The aim of this survey was to explore the availability of toe pressure-relieving adjuncts, including tenotomy, in diabetic foot services.
Methods
The survey focus was on tenotomy of toe tendons and pressure- relieving adjuncts to standard care to inform a prospective research study.
An online survey using Google Forms was developed, reviewed and piloted by the DF-SIG in line with designing and reporting survey guidelines.6 The questions explored the composition of the diabetic foot MDT at each centre, defined offloading therapies offered for DFU by the MDT and determined interest in collaborating in DFU research led by the DF-SIG (see Appendix 1 online at www.jvsgbi.com).
The survey was aimed at healthcare professionals involved in diabetic foot care. It was promoted through advertisement on social media platforms such as Twitter, distributed to mailing lists by the British Orthopaedic Foot and Ankle Society, College of Podiatry members and targeted invitation to lead clinicians in diabetic foot units.
Formal ethical approval was not sought as this is a survey of healthcare professionals and therefore formal informed consent was not required.
The survey ran between 13 January 2021 and 1 March 2021.
Data analysis
Raw survey data were extracted onto Microsoft Excel, cleaned and duplicate responses removed. Counts and percentages were reported for each survey item.
Results
Reach
The scoping survey had 168 responses from 10 countries. The majority of respondents were from the United Kingdom (94.6%, 159/168).
Orthopaedic specialists made up the majority of responses (61.3%, 103/168) with other specialties including podiatry (28.6%, 48/168), diabetology (5.4%, 9/168) and vascular surgery (4.8%, 8/168).
Surgeons were the most frequent responders (56%, 94/168), followed by podiatrists (19.6%, 33/168) and physicians (12.5%, 21/168). Other healthcare professionals included nurse specialists, nurses, interventional radiologists, orthotists, physiotherapists and dieticians.
Diabetic foot services
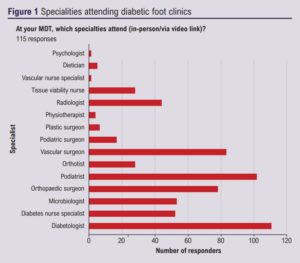
One hundred and nineteen of the 168 responders (70.8%) had a dedicated diabetic foot clinic at their centre. The clinic commonly consisted of a podiatrist (93.2%), diabetologist (81.4%), orthopaedic surgeon (62.7%) and diabetes specialist nurse (55.1%). 42.4% of clinics had an orthotist. Other specialties in attendance are shown in Figure 1.
Of those who responded, 64.1% (107/167) reported having a diabetic foot MDT either at their hospital or the regional centre and 30% (50/167) did not. Other responders stated the MDT was integrated during diabetic foot clinics or they had irregular and ad hoc MDTs.
Tenotomy practice
Ninety-nine (58.9%) responders reported having an active tenotomy service. Indications for tenotomy included: as an ulcer prevention strategy but with appropriate reversible toe deformity (66%, 68/103), following onset of ulceration (52.4%, 54/103) and following healed ulceration to prevent recurrence (55.3%, 57/103).
Orthopaedic surgeons most commonly perform tenotomy (75.7%, 78/103), followed by podiatric surgeons (24.3%, 25/103), vascular surgeons (5.8%, 6/103), podiatrists (3.9%, 4/103) and diabetologists (2.9%, 3/103). Other operators included vascular nurses and surgical care practitioners.
Of the centres offering tenotomy, 47.6% (49/103) perform tenotomy monthly and 21.4% (22/103) of centres perform tenotomies yearly. Only 4.9% (5/103) perform tenotomies weekly. Other respondents reported only doing them as part of another procedure or frequency depending on patient suitability.
Most tenotomies are undertaken in theatres in full asepsis (60.8%, 62/102). Other settings included outpatient clinic clean rooms and ward-based clean treatment rooms.
Tenotomy is performed under local anaesthetic (50.5%, 52/103), regional anaesthetic (15.5%, 16/103) or with no anaesthetic (13.6%, 14/103); 5.8% (6/103) routinely performed tenotomy under general anaesthetic. Other responders tailor the anaesthetic to the degree of neuropathy.
Surgical tenotomy was the preferred method (68%, 70/103). Needle tenotomy was used by 20.4% (21/103) of responders, and 11.7% of responders did not know the details of the technique as it was performed by a colleague.
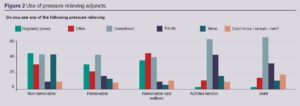
Over half of centres perform tenotomy in isolation (52.9%, 54/102). Others perform it with osteotomy/joint fusion (36.3%, 37/102), with Achilles tendon lengthening (29.4%, 30/102) or with casting (20.6%, 21/102). The frequency of use by each centre is shown in Figure 2.
Prior to tenotomy, most centres require patients to undergo an arterial assessment; 61.8% (63/102) of centres require patients to have palpable foot pulses, 42.2% (43/102) require multiphasic signals on hand- held Doppler, 21.6% (22/103) performed ankle-brachial pressure index and 8.8% (9/103) centres require a formal arterial duplex. 6.9% (7/103) of responders reported no arterial assessment was required prior to tenotomy. Other assessments included foot radiographs; 51% (52/102) of centres request a weight-bearing radiograph and 32.4% (33/103) require an anterior/posterior and lateral view foot radiographs. 57.8% (59/102) of centres assess patients for clinical evidence of a reducible foot deformity prior to tenotomy.
Future research
Of the responders, 49.4% (83/168) would be willing to take part in a trial to evaluate pressure-relieving adjuncts. 37.5% (63/168) would not want to take part as they felt tenotomy was an established treatment, they lacked research capacity or were not in equipoise. Other responders reported they would need to consult the local department or required more information about the proposed research before agreeing to engage further.
One hundred and twenty-four of the 168 responders (73.8%) wished to be further contacted about the project and 82.1% (138/168) of responders were willing to help involve their patients in designing a future trial.
Discussion
This predominantly UK-based tenotomy scoping survey had a good response rate, with an appropriate spread of specialists from the key relevant stakeholders. The results have demonstrated that there is clear variation in tenotomy practice. Tenotomy was not available in a third of centres who responded, and in those who did, there was little consensus on indications, preoperative assessment or how the procedure should be undertaken, with half of centres (54/102) offering it as a stand-alone procedure. In addition, despite the high prevalence of DFU, tenotomy was infrequently performed. The reason for this is unclear from this survey.
Another finding from this survey was the apparent lack of compliance with UK National Institute for Health and Care Excellence (NICE) guidance on the structure of diabetic foot services.7 Thirty percent of responders reported no dedicated diabetic foot clinic at their centre. In centres that operated a diabetic foot clinic there was a lack of representation in certain specialities advised to be part of diabetic foot services, in particular vascular surgery, microbiology and interventional radiology. A dedicated orthotist was available in less than 50% of diabetic foot clinics.
There is some evidence that tenotomy may reduce DFU healing times and prevent ulcer recurrence. To date, two systematic reviews have reported positive outcomes associated with tenotomy and low complication and recurrence rates; however, the absolute numbers are small with heterogeneous case mixes.5,8 The review by Bonanno and Gillies of retrospective case series reported 97% of ulcers healed postoperatively, with the postoperative ulcer healing time ranging from 21 to 40 days. The estimated ulcer recurrence rate was 6–17%.5 The literature reports DFU healing time to range from 1 month to over 1 year and is dependent on a number of factors.9–11 Armstrong et al estimates ulcer recurrence to be around 40% at 1 year.12
There is less evidence for tenotomy as a primary prevention intervention. A retrospective case series by Rasmussen et al reported no ulceration in 22 patients over 4 years.13 A further two small retrospective case series support this finding.14,15
The International Working Group on the Diabetic Foot (IWGDF) published guidance on DFU offloading methods in 2020. The guidance found weak evidence to support tenotomy to promote healing if non-surgical offloading options fail in patients with neuropathic plantar or apex digital ulceration, due to non- statistically significant findings of combined randomised trials.8,16,17 However, despite limited randomised controlled trial evidence, the IWGDF still supports offering tenotomy for non-healing digital ulcers associated with deformity as their expert opinion is that the benefit of tenotomy outweighs the harm. The cost effectiveness and patient-reported outcomes of this position are unknown.16 This therefore supports the rationale that a properly protocolled and delivered trial is required.
Most centres in this survey require patients to undergo arterial assessment to ensure adequate perfusion for healing and biomechanical assessment to screen for reducible foot deformity amenable to tenotomy. This approach was echoed in the literature where ankle pressure brachial index (ABPI) and clinical assessment of deformities amenable to tenotomy were commonly undertaken.18
Surgical tenotomies were preferred in this cohort of responders, with most procedures undertaken with full asepsis in an operating theatre setting. This is at odds with the literature where percutaneous tenotomy is in vogue, and is likely to be due to the high number of orthopaedic surgeons who responded to this survey. Small case series and cohort studies report percutaneous tenotomy to be safe and effective.18–20 There is limited high quality evidence to suggest whether surgical versus percutaneous tenotomy differ in healing rates, ulcer recurrence or adverse event profiles. Supporters of the percutaneous approach argue that it can be undertaken in the outpatient setting, therefore reducing healthcare costs, and is potentially more cost effective without compromising safety. One caveat to the survey responses reported is that foot and ankle surgeons made up the majority of respondents (61%). This is without doubt a potential bias to the survey responses as approaches, settings and the use of adjuncts might differ across specialties.
This scoping survey found that nearly three-quarters of responders were willing to engage in further research on this topic and over 80% would be willing to involve their patients. However, some responders felt there was an established tenotomy practice and therefore lacked equipoise. While the step-by-step technique of tenotomy may be established, there is no high-quality level 1 evidence to support the indication for tenotomy, timing of the procedure or benefits of the procedure in patients with diabetes. These questions need to be addressed in the form of a randomised controlled trial. The first step will be to undertake a feasibility trial to ensure the proposed trial is deliverable.21
The potential weaknesses of this study include not capturing all tenotomy practice and reporting bias by responders. Another weakness is the high number of orthopaedic responses and relatively low number of responses from endocrinologists and vascular surgeons, who typically manage patients with DFU. This may have skewed some results.
Conclusion
The results of this survey showed the variation in tenotomy practice and an appetite for collaborative research in this area. The Vascular Society of Great Britain and Ireland Diabetic Foot Specialist Interest Group will address these uncertainties through further collaborative research to investigate the role tenotomy may have in the treatment and prevention of DFU.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(2):54-58
Publication date:
February 11, 2022
Author Affiliations:
* Vascular Society Diabetic Foot Specialist Interest Group Collaborative











