PROTOCOL
The clinical effectiveness of waxing or epilation compared with other methods of hair removal in reducing the incidence of surgical site infections: a protocol for a systematic review
Cutteridge J,1,2 Garrido P,3 Staniland T,4 Lathan R,1,5 Smith G,1,5 Chetter I1,5
Plain English Summary
Why we are undertaking this work: When you have surgery such as vascular surgery, doctors often remove hair from the part of the body where they will operate. There are different ways to do this, but some methods might increase the risk of infections after surgery. In this research we want to study two methods of hair removal: waxing and epilation. Both involve pulling hair out by the roots. We will compare these methods with other ways of removing hair to see if they are better or worse at preventing infections after surgery. Infections after surgery can be serious. They can lead to other health problems, longer stays in hospital and higher costs for your healthcare. In some cases, like after surgery to restore blood flow to the legs, infections can be so severe that they lead to major amputation. Currently there is no widespread agreement among experts about the best way to remove hair before surgery. Some think waxing and epilation might be better because they might help wounds heal and make it easier to keep the area clean. Others worry that these methods might actually increase the risk of infection.
What we aim to do: We are going to look at all the research studies that have been done on this topic and find the ones that compare waxing and epilation to other hair removal methods or no hair removal at all. Then we will look at the results of these studies to see what they tell us about the risk of infections after surgery. Our plan includes several steps: (1) search medical databases and other sources for research studies; (2) select the studies that meet our criteria and exclude ones that don’t; (3) extract the details and results from the selected studies; and (4) analyse the data to see what it tells us about infections after surgery with different hair removal methods.
What this means: If you are going to have vascular surgery, this study could help you and your doctors decide the best way to prepare for your operation. If waxing or epilation is found to be better at preventing infections, it might become a common practice. If not, it might lead to other ways to reduce the risk of infections. One thing to keep in mind is that we might not find enough studies on this subject. If that happens, it will tell us that more research is needed in this area.
Abstract
Background: Surgical site infections (SSIs) represent a significant challenge in healthcare, contributing to morbidity, mortality as well as economic burden. Traditional preoperative methods of hair removal are under scrutiny, with some methods potentiality increasing the risk of SSIs. This systematic literature review (SLR) protocol outlines the assessment of the clinical effectiveness of waxing and epilation compared with other methods of hair removal in reducing SSIs.
Methods: Using PRISMA guidelines and the Joanna Briggs Institute Evidence Synthesis Checklist, this review aims to evaluate all interventional and observational studies that compare waxing or epilation against other methods or, indeed, no hair removal. The SLR has been prospectively registered with PROSPERO (ref: CRD42023423798). A comprehensive search strategy across Medline, Embase, CENTRAL, Clinicaltrials.Gov and CINAHL is planned, complemented by handsearching references of key articles. Important inclusion criteria include adult patient population, English language studies, and SSI reporting at 30 days. Both the Cochrane Risk of Bias (RoB2) tool and Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool will be employed. Data extraction will include study characteristics, participant characteristics, intervention and comparator details, and primary outcome data. The primary outcome is overall incidence of SSIs and, if feasible, a quantitative analysis including meta-analysis will be performed.
Discussion: This review has the potential to fill a knowledge gap around waxing and epilation as methods of preoperative hair removal, examining their impact on SSI incidence. These techniques offer theoretical advantages, such as extended hair-free periods and possible promotion of wound healing, but also have potential risks due to increased microtrauma. Due to the paucity of high-level evidence, there is a lack of consensus around their use. The outcomes of this review could reaffirm current guidelines or guide future practices. The high incidence of SSIs in areas like vascular surgery highlights the therapeutic potential of new evidence. One limitation of the study might be the small volume of literature on the subject, which could decrease statistical analysis power and make quantitative comparison challenging. If no high-quality evidence is found, this would indicate an unexplored area, potentially informing the design of primary research into waxing and epilation as SSI prevention methods.
Conclusion: This protocol lays the foundation for a comprehensive review of the clinical effectiveness of waxing and epilation in the prevention of SSIs. The insights gained could shape current clinical practice, influence guidelines or guide future research, ultimately contributing to the reduction of the substantial burden of SSIs.
Background
Hair has traditionally been removed from surgical sites preoperatively, but there is gathering evidence that some methods of hair removal can increase the risk of surgical site infections (SSIs).1,2 The most recent Cochrane review (2021) found that, while hair removal using clippers or depilatory cream does not significantly increase the risk of SSIs, razors may increase the chance of SSI development (moderate-certainty evidence).3 This is reflected in current NICE guidelines, which state that hair should be removed preoperatively only when its presence interferes with the operation.4 In this situation, it is recommended that hair is removed on the day of surgery with electronic clippers with a single-use head.4
Epilation involves the removal of hair by the root, commonly achieved through waxing or the use of a mechanical epilator. These techniques offer a theoretical advantage over other methods of hair removal because the removal of the hair by the root causes increased disruption within the dermal microenvironment, promoting greater influx of inflammatory cells, which may assist in healing of wounds and prevent possible infection evolving into a clinically overt SSI. These methods also provide an extended hair-free period, which simplifies wound cleaning, the application of dressings, and enables clinicians to identify the signs of SSI development with greater ease. However, the increased microtrauma seen with epilatory techniques may itself increase the risk of SSI development. Due to the paucity of high-level evidence, there is no consensus around the use of waxing or epilation as methods of preoperative hair removal and their effect on SSI incidence.
The prevention of SSIs is an area of increasing research interest due to their high disease burden. SSIs account for up to one in seven hospital acquired infections in the UK and are a cause of considerable morbidity and mortality.5 For instance, up to 30–40% of patients who develop a SSI following lower limb bypass surgery will require subsequent major amputation.6 SSIs also prolong hospital admissions and necessitate extended antibiotic treatment, increasing psychological distress for patients and inflating healthcare costs.1,7 Indeed, SSIs are estimated to cost the National Health Service (NHS) £700 million per year in the UK.8
This systematic literature review (SLR) aims to evaluate the current evidence in the preoperative removal of hair using waxing and epilating to reduce SSIs.
Methods
This systematic review will be conducted using the Joanna Briggs Institute Evidence Synthesis Checklist.9 Findings will be reported according to the extension for Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines.10 This SLR protocol has been constructed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) statement,11 which is shown in Supplementary Table S1 (see Appendix 1 within PDF). This review is prospectively registered with PROSPERO (ref: CRD42023423798).
Criteria for considering studies for review
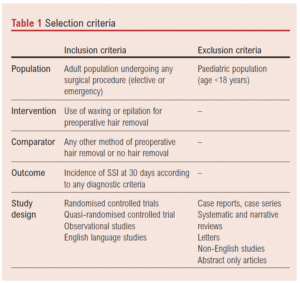
Studies will be included if they meet the following inclusion criteria: (1) randomised controlled trials, quasi-randomised controlled trials, observational studies; (2) comparing waxing or epilation against any other method of hair removal, or against no hair removal; (3) reporting the incidence of SSI at 30 days; (4) English language studies; (5) adult patient population. These selection criteria are summarised in the recommended PICOS format (Table 1). No limitations in sample sizes or quality of study will be applied to studies that meet these criteria, in order to comprehensively assess the literature. Systematic and narrative review articles will be excluded, although references will be hand searched. A subgroup analysis of randomised studies will be performed.
Search methods for identification of studies
Electronic searches
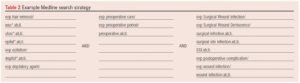
The search strategy will be designed in conjunction with an information specialist (TS) and will comprise a comprehensive search of Medline, Embase, CENTRAL, ClinicalTrials.gov and CINAHL. An example Medline search strategy is shown in Table 2.
Searching other sources
Additional searches will be conducted through handsearching the reference lists of included articles and excluded review articles.
Data collection and analysis
Selection of studies
Search results will be uploaded to Covidence systematic review software which automatically removes duplicated articles. Titles and abstracts will be initially screened independently by two researchers (JC and PG) to ensure they meet all selection criteria. Any disagreement that cannot lead to consensus after discussion will be discussed with a third senior researcher (RL) who will then adjudicate. All articles identified as relevant will undergo assessment of the full-length manuscript to confirm they meet all the selection criteria. As before, this will be performed independently by two researchers (JC and PG), with a third (RL) to manage disagreement on any points. The number of search hits, duplicates removed, full texts reviewed, articles excluded (with reasons), and the final number of studies included will be reported using the PRISMA flow diagram.10
Data extraction and management
Data will be independently extracted by two researchers (JC and PG) onto two separate Microsoft Excel spreadsheets using a bespoke data extraction form. Data to be extracted will include the following:
Study characteristics: year of publication, country, study design, sample size, length of follow-up, setting, inclusion and exclusion criteria.
Participant characteristics: age, gender, smoking status, patient comorbidities and medications, operation performed, perioperative use of antibiotics, type of dressing, postoperative complications, return to theatre rates and mortality.
Descriptions of intervention and comparators: waxing or epilation method, details of hair removal technique, timing of intervention, comparative method used.
Primary outcome data: SSI incidence at 30 days, method of SSI diagnosis (eg, CDC criteria ASPESIS, or Southampton scoring system, etc.
Details of methodology relevant to risk of bias assessment such as randomisation, blinding, etc will also be extracted at this stage.
Assessment of methodological quality
The Cochrane Risk of Bias (RoB2) tool12 will be used to assess the methodological quality of randomised controlled trials, whilst the Risk of Bias in Non-randomised Studies of Interventions (ROBINS-I) tool13 will be used to assess non-randomised studies. Each study will be assessed by the two independent reviewers with the respective tool and any disagreement resolved by consensus from a third. These tools provide an overall score of risk of bias (‘low’, ‘unclear’, ‘high’). Publication bias and selective outcome reporting will be explored with the use of funnel plots.
Statistical analysis and data synthesis
The primary outcome will be the overall incidence of SSIs by hair removal method (eg, comparison 1: waxing vs shaving; comparison 2: epilating vs clipping, etc). Secondary outcomes will include complication and reintervention rates. After data have been crosschecked, a narrative summary will be synthesised. If appropriate (depending on study heterogeneity), quantitative analysis will also be performed following the Cochrane guidelines for meta-analysis using the Review Manager (RevMan) V5.4 software program.14 Possible additional analysis includes subgroup analysis by intervention and comparator method, operation type, sex, diabetes status, smoking history, use of immunosuppressants or anticoagulants. For this study, due to the expected heterogeneity, a random effects model will be employed, providing there is no indication of funnel plot asymmetry. Absolute numbers of patients and events will be presented for each trial within the meta-analyses and any/all subgroups. The summary statistics will be presented as risk ratios and their corresponding 95% confidence intervals will be estimated for each trial. Forest plots will be displayed to illustrate the effect size for each trial and the combined effect size. For each analysis, τ2 will be presented as an estimate for the variance of true treatment effects between the trials, and the I2 used to display the estimated proportion of variability that can be attributed to trial heterogeneity. A two-tailed significance level of 5% will be used for all statistical analyses. The overall certainty of evidence for all outcomes will be assessed in accordance with the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.15
Discussion
This protocol outlines a systematic review to evaluate preoperative waxing or epilation in the reduction of SSIs. There is currently little evidence to support preoperative hair removal by any method, although waxing or epilation could reflect changes in this guidance. Should this review find evidence that waxing and epilation confer a greater risk of SSIs compared with clipping, it would reaffirm current guidelines and indicate that other methods of reducing the incidence of SSIs should be examined instead. Thus, any evidence produced from this study would provide valuable information, particularly to those areas of surgery that are at high risk of SSIs, such as vascular surgery where SSIs may complicate up to 40% of procedures.16
One key limitation of this study is the predicted small volume of literature surrounding waxing and epilation, which will decrease the power of any statistical analysis. Furthermore, given the lack of guidance around waxing and epilation, studies may diverge greatly in methodology, which would make any quantitative comparison unfeasible.
Should this review fail to find any studies that meet the inclusion criteria due to the lack of high-quality evidence, it would indicate that waxing and epilation encompass a relatively unexplored area of SSI prevention. The insight gained in this review could be used to inform the design of evidence-generating primary research into waxing and epilation, exploring both their feasibility and efficacy as methods of primary SSI prevention. The high incidence of SSIs in vascular surgery would stipulate that any primary evidence garnered here would have high therapeutic potential, which would make it an appealing site for further research.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023; 3(1): 52-55
Publication date:
November 20, 2023
Author Affiliations:
1. Academic Vascular Surgical Unit, Hull University Teaching Hospitals NHS Trust, Hull, UK
2. York and Scarborough NHS Foundation Trust, York, UK
3. Surrey and Sussex Healthcare NHS Trust, Redhill, UK
4. Hull University Teaching Hospitals NHS Trust Library Service, Hull, UK
5. Centre for Clinical Sciences, Hull York Medical School, Hull, UK
Corresponding author:
Joseph Cutteridge
Academic Vascular Surgical Unit, Hull Royal Infirmary, Hull, HU3 2JZ, UK
Email: joseph.cutteridge@ doctors.org.uk











