ORIGINAL RESEARCH
Thoracic outlet syndrome: a survey of operative practice amongst vascular surgeons
Al-Saadi N,1 Shalan A,1 Elbasty A,2 Popplewell M,1,3 Wall M,1,3 Pherwani AD,4,5 Smith F,6 Fligelstone L,7 Garnham A1,8
Plain English Summary
Why we undertook the work: Thoracic outlet syndrome (TOS) is a condition that occurs when the nerves or blood vessels in the space between the collarbone and your first rib are compressed. This can lead to pain in the neck, shoulders and arms, as well as numbness in the fingers. Although TOS is relatively rare, it can impact a person’s daily life. Identifying and treating TOS can be challenging, partly because there is no single definitive test for diagnosis, and treatment options can vary between surgeons. This study aims to better understand how vascular surgeons manage TOS.
What we did: A questionnaire made up of 12 questions covering various aspects of TOS operations was developed. This included assessment before surgery, surgical approaches and care following surgery. The survey was distributed online to vascular surgeons globally, allowing responses to be collected over eight months.
What we found: Eighty-one vascular surgeons responded, mainly from the UK. TOS operations were performed at multiple hospitals and the number of procedures differed amongst surgeons. Most operations addressed relieving the compression on the nerves or veins. While different surgical approaches were used, an incision above the collarbone was employed most frequently. The type and length of follow-up varied between the survey respondents. Most surgeons supported the idea of creating a database for TOS, where information about patient cases is collected and stored.
What this means: Our findings highlight how TOS is being managed by vascular surgeons. Creating a database for TOS operations could be valuable to better understand treatment options, patient outcomes and to help improve future care.
Abstract
Introduction: Thoracic outlet syndrome (TOS) poses a significant challenge in clinical management due to its varied presentation and impact on patients’ quality of life. Currently, there are no standardised guidelines used for the management of these patients and guide surgical intervention. This survey aimed to assess practices related to the pre-, peri-, and postoperative management of patients with TOS amongst vascular surgeons.
Methods: This online cross-sectional survey was designed and distributed to vascular surgeons at consultant or specialist registrar levels. The survey was designed by two vascular surgery trainees and validated by vascular surgery consultants with a specialist interest in TOS. Data collection occurred over eight months through an online survey platform, and responses were analysed using descriptive statistics and narrative analysis.
Results: The survey was completed by 81 vascular surgeons. This included 55 consultant-level and 26 speciality registrar-level surgeons, primarily from the UK. Most survey respondents (86%) reported that their centre performed surgical decompression for TOS. The median number of cases performed by each centre annually was eight. Venous and neurogenic TOS were the most reported indications for surgical intervention (78%) and the supraclavicular approach was the most frequently used operative approach (87%). There did not appear to be any standardisation in postoperative management or follow-up, including reporting of treatment outcomes.
Conclusions: This survey highlights the significant variability in pre- and postoperative practices related to TOS among vascular surgeons. Further research, including observational studies, is needed to better understand the relationship of assessment, surgical approaches and perioperative care with patient outcomes to help guide future practice.
Introduction
Surgical management for thoracic outlet syndrome (TOS) is undertaken in several surgical specialties including thoracic, plastic, vascular and neurosurgery.1 The reported incidence of TOS is approximately 1–3 per 100,000;2,3 however, despite the uncommon nature of this condition, it can have a significant impact on patients’ quality of life.4,5 Currently, there are no established guidelines for the surgical management of patients with TOS, although reporting standards published by the Society for Vascular Surgery in the USA have attempted to address this issue.6 As a result, surgical practices are largely dictated by individual surgeon preferences,7,8 which are likely to be influenced by training and experience.
More information is needed to better understand practices related to TOS and to explore the potential benefits of a registry to inform guidelines and clinical decisions. It is known that surgical registries offer numerous advantages including identifying practice trends, developing treatment protocols, directing research efforts and enhancing patient outcomes.9 Establishing a registry for TOS operations would enable the collection, monitoring and analysis of data related to patient operative workup and outcomes. This data could significantly influence the development of national guidelines for diagnosing and managing patients with TOS.
We designed a specific questionnaire to explore current practices related to TOS including preoperative, operative and postoperative practices among vascular surgeons. It also aimed to establish the willingness of vascular surgeons to take part in a formal registry of patients with this condition who undergo surgical intervention.
Methods
This study is reported in line with the Checklist for Reporting of Survey Studies (CROSS).10 A survey was designed by two vascular surgery trainees (AS and AE). The survey was validated after being piloted by four vascular surgery consultants (FS, LF, ADP and AG) who have a specialist interest in the management of TOS. Minor changes were then made to the survey including changing the formatting and wording of some of the questions to improve readability. The final version of the survey can be found in Appendix 1 online at www.jvsgbi.com.
An online cross-sectional survey assessing variability in practice related to the surgical management of patients with TOS was undertaken. The target population of the survey was vascular surgeons including those in specialist training programmes. The study was primarily designed to understand practices by vascular surgeons in the UK (there are approximately 400 consultant members of the Vascular Society of Great Britain and Ireland); however, it was also open to vascular surgeons internationally.
The survey consisted of 12 questions and comprised four main sections: identification of centres which carry out surgical decompression for TOS and estimated number of cases per annum; preoperative practice including assessment and indication for treatment; operative practice; and postoperative practice. The survey consisted of a combination of free-text responses and closed questions. It could be completed anonymously by the respondents, who also had the option of providing their email addresses to be involved in future studies on a voluntary basis.
Data collection and analysis
The survey was undertaken via the SurveyHero tool11 and distributed via the VSGBI mailing list, UK national education programmes for trainees and social media platforms. The survey was open for a period of eight months from 1st February to 1st September 2020.
At the end of the survey period all the responses were collated and entered into Microsoft Excel for data cleaning and analysis. This was password-protected and could only be accessed by the first author (NA-S). At the end of the survey, participants had the option of providing an email address so that contact could be made regarding any future study. This information was also used to screen for multiple participation. For any duplicates identified, only the most recent response was included in the results. Incomplete survey responses were also included in the analysis. Missing data are clearly identified in the Results section. Free-text responses were collated, analysed and themes were identified, when possible, by the first author (NA-S) and reviewed and independently verified by another author (AS). Descriptive statistics including percentages and frequencies were used in the analysis of the closed questions. Graphical illustrations were created using GraphPad Prism version 10.
Ethical considerations
The surveys were all completed optionally by persons meeting the inclusion criteria listed above and consent was indicated by survey completion. Formal ethical approval was not sought as this work did not meet criteria to be classed as research using the Health Research Authority (HRA) decision tool.12 Data were kept and managed in accordance with local governance policy with strict adherence to the Data Protection Act (1998) and the principles of Good Clinical Practice.13
Results
Survey respondents
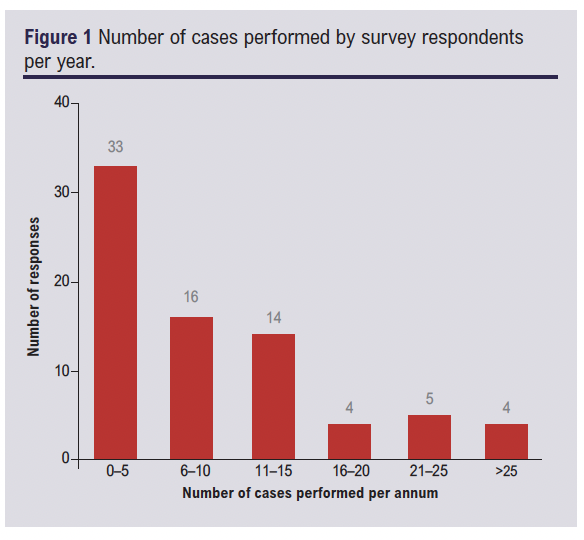
This survey received responses from 81 vascular surgeons including 55 (68%) consultant level surgeons and 26 (32%) vascular speciality, non-consultant level surgeons. Due to the online nature of the survey and it being shared on social media, it was not possible to calculate a total response rate. Most respondents (70/81; 86%) stated that surgical decompression for the management of TOS was carried out at their vascular centre. The number of cases performed annually between the respondents ranged from 0 to 40 (Figure 1).
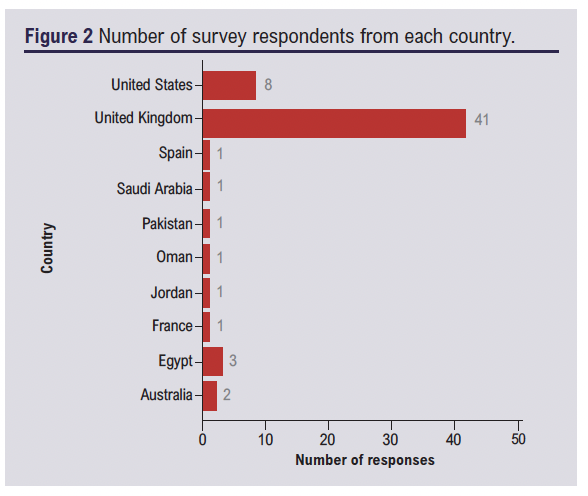
Of the respondents who provided their contact details (60/81), 41 (68%) worked at a vascular centre in the UK at the time of survey completion and 19 (32%) worked in other centres internationally (Figure 2).
Preoperative practice
The types of TOS most often referred for surgical decompression were venous TOS (VTOS) (25/65; 39%) or neurogenic TOS (NTOS) (25/65; 39%). Arterial TOS (ATOS) was reported as the most common indication for surgical intervention by 15 respondents (23%).
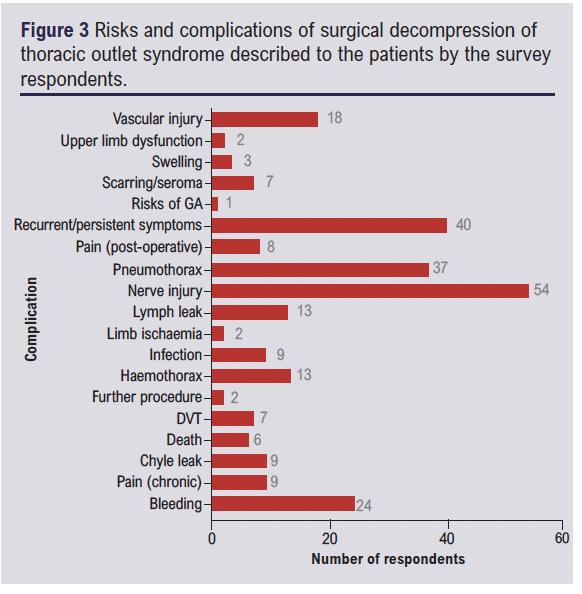
The most common operative risks explained to patients preoperatively were the risk of nerve injury (54/65, 83%), including mentioning injury to specific nerves (phrenic or long thoracic) and non-specific nerve injury, and recurrent or persistent symptoms (40/65, 62%). Other risks mentioned to patients included pneumothorax, haemothorax and bleeding (Figure 3).
Operative practice
There was varying practice in the surgical approach used to manage TOS between the respondents. The surgical approaches used included supraclavicular, infraclavicular, transaxillary, paraclavicular, transmanubrial or a combination of two or more of the approaches. The most common surgical approach used was the supraclavicular approach (54/62, 87%), followed by the transaxillary approach (21/62, 34%) and the infraclavicular approach (12/62, 19%). More than one-third of respondents used more than one surgical approach (23/62; 28%).
Postoperative practice
Most respondents (53/77; 69%) used routine clinical examination as their primary method of assessing patients’ symptoms postoperatively. Some respondents (24/77; 31%) used an objective assessment of postoperative outcome including the disabilities of the arm, shoulder and hand (DASH) questionnaire (6/24; 25%) and postoperative imaging investigations (18/24; 50%).
Reported duration of follow-up postoperatively ranged from 1.5 months to 72 months. Median length of follow-up was 6 months (IQR 3–12 months). In the free-text responses some participants (5/64; 6%) noted that length of follow-up depended on the patient and symptom relief and one respondent reported they would continue to follow patients with TOS life-long.
Scope and support for a national TOS registry
Support for a national registry of patients who undergo an operation for TOS was expressed by 78/81 (96%) respondents and 65/81 (80%) welcomed being part of a discussion group to develop this.
Discussion
This study is the first survey to examine the practices of vascular surgeons regarding TOS and is the first survey to assess this to the best of the authors’ knowledge. Survey respondents were primarily from various centres throughout the UK. The limited representation of centres internationally could be due to the survey being distributed via UK-based society mailing lists and social media platforms. Most responses were from consultant vascular surgeons who are directly responsible for patients under their care and therefore most likely to be able to describe their perioperative practices.
Differences in the experience of vascular surgeons in the management of patients with TOS was demonstrated by this survey. Whilst most survey respondents reported that surgical decompression for TOS was undertaken at their centre, the annual number of cases performed at each centre varied. Twenty-five or more cases were performed annually by 17% of centres, with respondents from the remaining centres reporting fewer numbers of cases performed per year. This highlights that, although surgical decompression for TOS is carried out by multiple units across the UK, the volume of cases remains comparatively low when compared with other vascular surgery procedures. Also, given that only a small number of centres and/or surgeons are performing surgery for TOS decompression, there could be a case for supra-regional centralisation. In other areas of vascular surgery in the UK (complex aortic work), we have already seen this trend over the last decade. Furthermore, with the relatively low volume of cases, a comprehensive registry used to collect and analyse outcomes from all surgeries performed for patients with TOS could provide valuable insights to guide future practice.
The most common indications for surgical intervention were distributed equally between VTOS and NTOS. NTOS has often been cited as the most common type of TOS, accounting for over 90% of cases.14 Although the incidence of VTOS is lower (8 per 100 0000),3 our findings may be explained by a higher proportion of patients with VTOS being likely to require surgical intervention compared with those with NTOS. This is supported by a systematic review which described the management of most patients with NTOS as conservative in the first instance.15 In contrast, the mainstay of interventional treatment for VTOS is thrombolysis before surgery, with anticoagulation alone associated with a high rate of vascular re-occlusion.16 Patients with ATOS often require immediate surgical intervention for upper limb ischaemia.17
There was some variation in the complications mentioned by survey respondents during the consent process for surgery. Whilst most respondents cited nerve injury and persistent or recurrent symptoms as a risk, pneumothorax was mentioned less frequently. In a study assessing postoperative complications following surgical decompression for TOS, it was found that nerve injury, pneumothorax and haemothorax were the most frequently reported complications.18 Despite this, over half of this survey’s respondents did not mention pneumothorax or haemothorax as a complication of the operation. This could be explained by the interpretation of the survey question by respondents, with some only commenting on the main risks they mention in their consenting process and others listing all possible risks in the free-text response. To better inform the consent process for surgical decompression of TOS in the future, larger-scale observational studies are required, which may help to determine the incidence of these complications based on surgical approach and type of TOS. This may be useful in helping to develop standardised consent information for patients undergoing TOS procedures.
The surgical approaches used included supraclavicular, infraclavicular, paraclavicular, transaxillary and transmanubrial. The supraclavicular approach was employed most frequently. This approach has previously been described to permit a greater exposure of the thoracic outlet and of the structures above the first rib.19 The use of more novel approaches, such as the video-assisted thoracoscopic and robot-assisted thoracoscopic approach20,21 for TOS decompression, was not selected by any of the participants. The latter approaches are more commonly undertaken by thoracic surgeons and, as our survey was directed at vascular surgeons, this could explain why experience of these procedures was limited in this study. A greater understanding of the reasons why different approaches are employed by clinicians and outcomes associated with the use of each is one of the benefits a national registry could offer. It is important to note, however, that establishing a national registry demands substantial financial resources, expertise and approval from advisory groups.22,23 With the creation of the national TOS dashboard, progress has already been made in this direction, which is promising.24
Most participants indicated they would rely on clinical evaluation for postoperative assessment, with objective tools being used less frequently. There was also considerable variation in the duration of postoperative follow-up among respondents. This variability in practice may be due to the lack of evidence regarding optimal methods and duration of postoperative follow-up for these patients. Clinician experience is likely to play a significant role in shaping individual surgeons’ practice.
The DASH questionnaire was designed for the assessment of quality of life and functional recovery following surgery for musculoskeletal conditions.25 There are no validated tools that measure similar outcomes specifically for patients with TOS. This is a potential reason why the use of DASH in the survey was low. However, specific reasons were not assessed in the scope of this study. A further understanding of this and the impact of longer follow-up periods on outcomes would be valuable for informing future practice.
The main limitation of this study is the random cross-sectional design. This may lead to some selection and reporting bias. However, we feel that this was the most appropriate way to increase participation in the study. Another limitation of our study included the small number of responses from participants outside the UK, suggesting that collaboration with other international societies could have enhanced the survey’s reach and generalisability. Additionally, the contact details were available for only 60 respondents, preventing us from assessing the affiliations of the other participants or identifying potential duplicates in these responses. As the survey specifically targeted vascular surgeons, insights into the practices of thoracic and plastic surgeons remain unknown. It may be beneficial to undertake an international pan-surgical speciality survey to determine the experiences of vascular, plastic, thoracic and neurosurgeons in the management of patients with TOS.
Conclusion
This study has revealed that, although surgical decompression for TOS is uncommonly performed, there is variability in the preoperative and postoperative practices amongst vascular surgeons. Indications for operative decompression are more commonly neurogenic or venous TOS and the supraclavicular approach is the one most often used. Our results support undertaking an observational study to understand the impact of different practices on patient outcomes and the establishment of a registry for patients who undergo a surgical operation for TOS. This could guide future patient management and inform national guidelines.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(4):226-230
Publication date:
August 17, 2024
Author Affiliations:
1. Black Country Vascular Network, West Midlands, UK
2. University Hospitals of Southampton NHS Foundation Trust, UK
3. Institute of Applied Health Research, University of Birmingham, UK
4. University Hospitals of North Midlands NHS Trust, UK
5. Keele University School of Medicine, UK
6. University of Bristol & North Bristol NHS Trust, Bristol, UK
7. Department of Vascular Surgery, Swansea Bay University Health Board, UK
8. Vascular Society of Great Britain and Ireland, UK
Corresponding author:
Nina Al-Saadi
Vascular Speciality Registrar, Black Country Vascular Network, Pensnett Road, Dudley,
DY1 2HQ, UK
Email: [email protected]











