SHORT REPORT
Transfusion requirements in elective open abdominal aortic aneurysm repair: a network review of practice
Leatherby RJ,1 Godfrey AD,1 on behalf of the Dorset and Wiltshire Vascular Network
Plain English Summary
Why we undertook this work: When there is a shortage of blood for transfusion the NHS recommends that surgery likely to require blood transfusion should be postponed. Open surgery for a dilated artery (aortic aneurysm) in the abdomen is traditionally considered likely to require blood transfusion and thus affected by these recommendations.
What we did: We reviewed 3 years of data from patients undergoing open surgery to repair aortic aneurysms in order to assess how many required blood transfusion.
What we found: Only seven of 90 patients (7.8%) undergoing open aortic aneurysm surgery needed a transfusion.
What this means: The transfusion rate following open aortic aneurysm surgery is much lower than the 15% risk limit suggested for postponing surgery in the current NHS guidelines when blood stocks are low. Therefore, in such circumstances, open aortic aneurysm surgery should continue.
Abstract
Introduction: Patients undergoing elective open abdominal aortic aneurysm (AAA) repair are considered a high-risk group for transfusion, with transfusion rates quoted around 15%. In the context of an NHS blood transfusion (NHSBT) Amber Alert, it is suggested that surgeries with a high risk of transfusion (>15%) are postponed unless otherwise clinically indicated. This review of network elective open AAA activity aimed to improve our understanding of transfusion requirements and risk profile.
Methods: National Vascular Registry data for patients undergoing elective open AAA repair in the Dorset and Wiltshire Vascular Network (DWVN) between January 2019 and February 2022 inclusive were retrospectively reviewed and cross-referenced with electronic patient records, pathology results, transfusion database and theatre records.
Results: Ninety patients (seven women and 83 men) undergoing elective open AAA repair were identified. Seven (7.8%) patients required a postoperative transfusion.
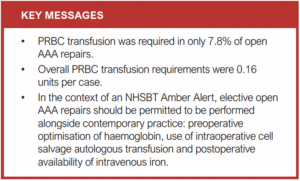
Conclusion: This contemporary review suggests elective open AAA repair should continue during an NHSBT amber alert as the risk of transfusion is lower than previously reported.
Background
During a recent NHS blood transfusion (NHSBT) Amber Alert1 for a shortage of Group O red cells available for transfusion, a recommendation to review higher risk surgeries which may require transfusion was implemented. Vascular surgery, and particularly open abdominal aortic aneurysm (AAA) repair, is often cited as being a particularly high-risk group (>15% transfusion requirement); however, specific data on transfusion requirements are largely lacking in contemporaneous UK practice. Previous studies have suggested a packed red blood cell (PRBC) transfusion requirement in 46-48.9% of patients undergoing open AAA repair.2,3 We undertook a retrospective review of our elective open AAA cases, with an aim to better understand transfusion requirements and risk profile.
Method
All elective open AAA repair cases from Dorset and Wiltshire Vascular Network (DWVN) between January 2019 and February 2022 inclusive submitted to the National Vascular Registry were retrospectively reviewed. Data were cross-referenced with electronic patient records, pathology results, transfusion database and theatre records.
Results
Ninety cases were identified, all with complete data sets available. All cases were performed as per the DWVN protocol within a designated vascular operating theatre with intraoperative cell salvage autologous transfusion in use for all cases. All cases were performed or supervised scrubbed by a Consultant Vascular Surgeon.
Seven female and 83 male patients were analysed with median (IQR) ages of 70.6 (65–74) years and 72.0 (68–76) years, respectively. The median AAA size was 59 and 56 mm for female and male patients respectively. The average length of stay following elective open repair during this period was 9 days (range 6–10) with a risk adjusted 30-day elective AAA repair survival of 99.4%.4
In total, seven patients received a PRBC transfusion (7.8%), all of which occurred in the postoperative phase of care. Table 1 outlines their characteristics.

A total of 14 PRBC units were transfused after appropriately triggering the local transfusion protocol of haemoglobin <80 g/L (mean 0.16 units/case). Three of these PRBC transfusions were single unit, one was two units and three were three units. Notably, all three patients receiving three units of transfusion required a return to theatre in the postoperative period for a complication. The median preoperative haemoglobin was 128.5 g/L (range 103–143 g/L) in this group (vs 130.1 g/L, NSD).
During the study period, the availability and use of intravenous iron in the postoperative care of vascular patients became more common with agreed standard operating procedures in place. This is considered likely to have positively impacted the transfusion requirements in this patient cohort and should also be considered alongside these data.
Conclusion
The requirement for PRBC transfusion following elective open infrarenal AAA in our network was 7.8%. This is well below the perceived and historic transfusion requirements in this group of patients. In the context of contemporary practice, our data would support such cases continue to be delivered during times of blood shortages.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(3):180-181
Publication date:
March 23, 2023
Author Affiliations:
1. Dorset and Wiltshire Vascular Network, Department of Vascular Surgery, Royal Bournemouth Hospital, Bournemouth, UK
Corresponding author:
Anthony Dean Godfrey
Clinical Lead Dorset and Wiltshire Vascular Network and Consultant Vascular Surgeon, Department of Vascular Surgery, Royal Bournemouth Hospital, Castle Lane East, Bournemouth BH7 7DW, UK
Email: [email protected]











