CASE REPORT
Traumatic thigh AV fistula leading to aneurysmal changes in aorta and iliac arteries
Zaki S,1 Hilles A,2 Chandrasekar R3
Abstract
Penetrating traumatic arteriovenous fistulas (AVFs) have the tendency to be clinically silent for many years and could be misdiagnosed as deep venous thrombosis (DVT) on initial presentation. A 52-year-old male underwent a duplex scan to evaluate swelling of the limb, which detected an AVF in the thigh. He was stabbed in the lateral aspect of the thigh 16 years previously. His left leg was larger with a palpable thrill in the thigh. A CT angiogram confirmed the AVF and aneurysmal changes in the common iliac artery (29 mm) and infrarenal aorta (32 mm). A moulding balloon was placed across the AVF by an antegrade puncture of the common femoral artery to control the arterial inflow and outflow. Following disconnection of the AVF, the defect in the side wall of the femoral vein was primarily repaired with Prolene. The defect in the superficial femoral artery was repaired by transection, spatulation and end-to-end anastomosis of the arteries. A Duplex scan performed six months postoperatively showed that the aorta (29 mm) and the common iliac artery (27 mm) had regressed. The authors suggest that, when faced with an AVF with a huge calibre mismatch between the arterial segment proximal and distal to the fistulous tract in a young patient, a hybrid approach should be considered for control and surgical disconnection of the fistula.
Introduction
Traumatic penetrating arteriovenous fistulas (AVFs) are very rare, with only 291 cases accounted for in the literature.1 The most common causes are stab wounds and gunshot wounds.1,2 AVFs of the extremities tend to present with pain, swelling or limb size discrepancy.3 If untreated, severe or chronic AVFs may lead to high output cardiac failure, functional impairment or steal, resulting in limb ischaemia and tissue loss.3
Case report
A 52-year-old male seen in the vascular clinic after an AVF was detected on a venous duplex scan. He complained of a swollen painful left leg for a number of years. After probing, he gave a history of a stab injury to the left thigh 16 years previously. On examination his left thigh was significantly larger than his right. He had a full complement of pulses, but a thrill could be felt on his inner thigh and a bruit could be heard.
A CT angiogram (Figure 1) showed dilatation of the common femoral artery (CFA) and the proximal two-thirds of the superficial femoral artery (SFA) and femoral vein (FV). Furthermore, due to the long-standing well developed AVF, the left common iliac artery (CIA) was tortuous and enlarged (29 mm), with mild aneurysmal dilatation (32 mm) of the infrarenal aorta.

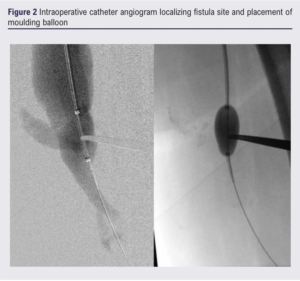
Intraoperatively, an antegrade catheter angiogram was performed to locate the exact site of the AVF and a moulding balloon (Figure 2) was used to control the arterial inflow and outflow. This aided the dissection of the SFA and the adjacent FV, both proximally and distally. Following dissection and sloop control of the vessels, the SFA and FV were clamped and the AVF disconnected. The defect in the side wall of the FV was primarily repaired with a 6/0 Prolene suture. The defect in the SFA was treated by transection, spatulation and end-to-end anastomosis of the arteries. A completion on-table angiogram confirmed restoration of the blood flow and a three-vessel run-off to the foot.
An aortic arterial duplex scan performed six months post-operatively showed that the aorta had regressed in size to 29 mm and the left CIA to 27 mm.
Discussion
Penetrating traumatic AVFs may be clinically silent in the acute setting, demonstrating minimal to no symptoms initially. This leads to a missed diagnosis, especially if there was no neurovascular compromise on examination.4,5 Even though some are self-limiting and would spontaneously heal,6 most would develop a significant fistulous tract size which renders them problematic.7,8
The consensus from the literature is that traumatic AVFs should be managed surgically rather than conservatively,9 and that an endovascular approach should be considered first as it is less invasive, more cost effective and has a lower rate of complications.2 In our case, given the patient’s young age and the calibre mismatch between the proximal and distal segments of the artery in relation to the fistulous tract, we opted for open surgery for a more durable outcome.
Conclusion
We suggest that, when faced with an AVF with a huge calibre mismatch between the arterial segment proximal and distal to the fistulous tract in a young patient, a hybrid approach should be considered for control and surgical disconnection of the fistula for a durable permanent solution.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(2):105-107
Publication date:
January 31, 2024
Author Affiliations:
1. Senior Clinical Fellow in Vascular Surgery, Countess of Chester NHS Trust, Chester, UK
2. Consultant in Interventional Radiology, Countess of Chester NHS Trust, Chester, UK
3. Consultant in Vascular Surgery, Countess of Chester NHS Trust, Chester, UK
Corresponding author:
Shady Zaki
Flat 410C, Winchester Road, Southampton SO16 7DH, UK
Email: shady_mikhael@ hotmail.com











