PROTOCOL
Use of rigid dressings versus soft dressings in the management of lower limb amputations: a systematic review protocol
Chua WY,1,3 Mohamed A,1,2 Smith G,1,2 Carradice D,1,2 Ravindhran B,1,2 Lim A,1 Aylward K,3 Chetter I1,2
Plain English Summary
Why we are undertaking this work: Amputations of the lower limb are occasionally a necessary treatment performed in such cases as severe diabetic foot infection, severely impaired blood supply to the legs or major trauma. After amputation, the remaining limb is usually bandaged to help with wound healing, pain control and swelling reduction. Several studies have investigated different types of dressings to assess if they have an impact on wound healing and mobility after surgery. This review will put together the findings of those studies to guide management of patients after amputation.
What we will do: We will review the results of published studies that compare rigid and soft dressings in patients who have undergone lower limb amputation. We will assess the benefits of each type of dressing and summarise the findings.
What this means: A review of the existing evidence will help us determine if rigid dressings have the potential to improve results after surgery compared with soft dressings. We will then be able to develop clinical guidance for the management of patients after lower limb amputation.
Abstract
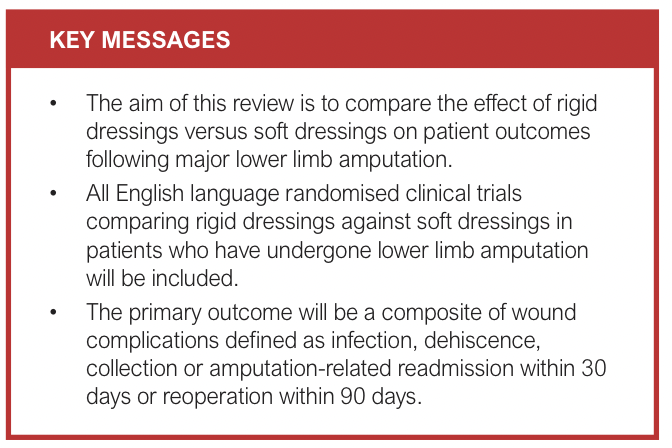
Background: Amputation of the lower limb is a procedure that is commonly performed, most notably in patients with diabetes, lower limb ischaemia and trauma. Wound dressings can impact patient outcomes such as wound healing, complication risk and time taken to prosthesis fitting. Recent studies have investigated the effect of rigid versus soft dressings with regard to these outcomes. The aim of this systematic review is to compare the effectiveness of rigid dressings against soft dressings among patients who have undergone lower limb amputation.
Methods: A literature search will be conducted in OVID Medline, EMBASE and the Cochrane CENTRAL databases, reference lists from included articles and previous reviews on the topic. The terms used in the search will include “above knee amputation”, “through knee amputation”, “below knee amputation”, “lower limb”, “rigid dressing”, “removable rigid dressing”, “plaster dressing”, “soft dressing”, “elastic dressing” and “elastic bandage”. Randomised clinical trials that look at both transfemoral and transtibial amputations for any indication will be included if they compared the impact of using rigid dressings versus soft dressings on patient outcomes. The primary study outcome is a composite of infection, dehiscence, collection or amputation-related readmission within 30 days or reoperation within 90 days. The Cochrane Risk of Bias (RoB 2) tool for randomised trials will be used for bias risk assessment and a meta-analysis of clinically homogenous studies will be performed using Review Manager (RevMan). A narrative systematic summary will be performed for data not amenable to meta-analysis.
Ethics and dissemination: This is a systematic review of published literature data and therefore ethics approval is not required.
Introduction
Amputation is often the most appropriate treatment for patients with a non-salvageable ischaemic limb, fulminant diabetic infection or after major trauma.1 The aim of the procedure is to relieve pain, preserve life and facilitate prosthetic reconstruction of the limb. In the UK, the annual lower limb amputation (LLA) rate is 11 per 100,000 in the population aged 25+ years.2 However, LLAs continue to be associated with high rates of postoperative complications, with additional surgical revisions and delayed wound healing being the most common.3
At the end of the amputation procedure a local wound dressing is applied, and this is usually followed by application of dressings that cover the residual limb, which helps protect the wound, reduce swelling and shaping of the residual limb. These measures aim to facilitate successful wound healing, reduce pain, maintain the range of motion and strength of the lower limb, and expedite prosthetic fitting.4 There are two main types of dressings that can be applied after a LLA – namely, soft and rigid dressings. The type of stump dressing used has an impact on these goals as inadequate shrinkage of the residual limb and swelling can impair circulation and wound healing.5
Soft dressings comprising elastic materials such as crepe bandages and compression socks are the most commonly used postoperative dressing owing to their low cost, availability and ease of application.6 Rigid dressings, on the other hand, employ hard exterior materials. These include removable rigid dressings such as vacuum-formed removable rigid dressings, and conventional rigid dressings such as plaster of Paris and plastic casts. They have grown in popularity as some specialists believe that they promote faster wound healing and reduce the time to prosthetic fitting.7 Additionally, rigid dressings have been proposed to provide the residual limb with better protection from trauma by reducing the incidence of injury following falls.5 However, they are more expensive than conventional dressings and, in many cases, require skilled personnel to safely apply them.8
Since the removable rigid dressing was first described by Wu et al in 1977,9 several studies have investigated its efficacy against soft dressings in LLA. Despite this, there has been no clinical consensus on which type of dressing leads to better patient outcomes. A 2018 Cochrane review concluded that there was insufficient evidence that either type of dressing is superior following amputation.10 The conclusions were made mainly due to the limitations in the design and execution of the studies included. However, two randomised clinical trials (RCTs) have since been published and their results may have a bearing on that conclusion.11,12 Despite a recent systematic review published by Koonalinthip et al in 2023 which incorporated the two published RCTs, the results remained inconclusive owing to the inclusion of several poor-quality non-randomised studies.13 This systematic review aims to determine the clinical effectiveness of rigid dressings compared with soft dressings in the management of the residual stump following LLA. We intend to measure wound complications as a composite primary outcome derived from the existing literature, as this is expected to serve as a robust measure of the clinical effectiveness of rigid dressings.
Methods
This systematic review is prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO) database (reference: CRD42024563421). The methods used in this review and its reporting are in line with the Preferred Reporting items for Systematic Reviews and Meta-analyses Protocols (PRISMA-P) guidelines and checklist.14
Search strategy
Sources that will be used to obtain studies for this review are EMBASE, OVID MedLine, Cochrane CENTRAL and CINAHL databases, and reference lists from previous reviews and included articles. No search date constraints will be applied.
A search with pre-defined search terms will be conducted in consultation with a qualified medical librarian. The databases will be searched for studies comparing the effects of rigid dressings versus soft dressings using keywords, equivalent terms and medical subject headings to maximise the search sensitivity. Search terms will include and are not limited to “lower limb amputation”, “above knee amputation”, “below knee amputation”, “rigid dressing”, “semi-rigid dressing” and “soft dressing”. A draft search strategy is shown in Appendix 1 (online at www.jvsgbi.com).
Inclusion criteria
All English language prospective RCTs of adult patients comparing the use of rigid dressings against soft dressings among patients who have undergone LLA at the transtibial, transfemoral or through-knee level will be eligible for inclusion in this systematic review. The types of rigid dressing include, but are not limited to, plaster cast socket, Unna semi-rigid dressings and vacuum-formed removable rigid dressings. Soft dressings include elastic bandages, cotton stockinette, compression socks and crepe bandages. The use of local wound dressings without a formal stump dressing is also permissible and will be included in the comparison as a type of soft dressing.
Study selection
The COVIDENCE web tool will be used for screening, study selection, data extraction and quality assessment. Search results will be uploaded to the web tool, followed by automatic duplicate identification and the manual removal of duplicates. These will then be screened independently by two authors. Eligibility of studies will be determined based on the title and abstract initially. After elimination of ineligible studies at this initial stage, full review of the manuscripts of the remaining articles will take place. Studies will be included by consensus and, if this is not reached, a third reviewer will provide arbitration. Where necessary, study authors will be contacted for further data or clarification.
Data extraction and management
Summary statistics of participant baseline characteristics, dressing type, study sample size, primary outcomes and amputation type will be collected and presented in a table. In addition, conflicts of interest, study funding and other sources of bias will be reported where available.
Raw data will be extracted from the manuscripts and entered into a dedicated Microsoft Excel (Microsoft, Redmond, Washington, USA) spreadsheet and Review Manager (RevMan) (Cochrane Collaboration, London, UK) prior to analysis.
Assessment of methodological quality
The risk of bias in selected RCTs will be assessed using the revised Cochrane Risk of Bias (RoB 2) tool for randomised trials.15 Two authors will independently assess each study, with any disagreements resolved by consensus or arbitrated by a third author. A narrative summary will be provided for studies deemed to have a critical risk of bias or no information and these will be excluded from data analysis and synthesis.
The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) system will be used to assess the certainty of the evidence for each outcome.16 Outcome certainty will be rated as “very low”, “low”, “moderate” or “high” per guidelines.
Outcomes
The primary outcome will be a composite of wound complications, defined as infection, dehiscence, collection or amputation-related readmission within 30 days or reoperation within 90 days.
The secondary outcomes include healing time, defined as time in days from amputation to wound closure; length of hospital stay following surgery; time to prosthetic fitting, defined as time in days from surgery to first prosthetic fitting; post-procedural pain; patient satisfaction; and adverse effects which include return to theatre post-amputation, joint contracture and death from any cause.
Statistical analysis
A forest plot summary will be provided for all meta-analyses. Continuous outcomes will be analysed and reported using mean or standardised mean difference (SMD) with a 95% confidence interval (CI). Dichotomous outcomes will be reported as risk ratios with 95% CI and, for time-to-event data, a hazard ratio with a 95% CI will be reported. Clinical homogeneity of selected RCTs will be assessed with respect to patient demographics, type of intervention and types of outcome assessment. If clinical homogeneity criteria are satisfied, statistical heterogeneity will be assessed using the χ2 and I² tests. A fixed effects model meta-analysis will be performed for studies where statistical heterogeneity is <60%, and for those >60% a random effects model will be used. Subgroup meta-analysis of studies included in any random effects model will be considered if the cause of statistical heterogeneity can be identified, such as a difference in amputation indication or presence of diabetes. A narrative review will be provided for outcomes that cannot be quantified or analysed in a meta-analysis.
Discussion
Amputation is a major life event for patients, their families and wider support network. All aspects of clinical care that is involved in such an event should be optimised in order to minimise complications and facilitate rehabilitation so that patients recover and take the next stage in their life journey. Professional bodies such as the British Association of Chartered Physiotherapists in Amputee Rehabilitation recommend rigid dressings,17 while others including Cochrane deemed that there was uncertain evidence in this area.10 A robust updated look at the evidence in this area will provide clarity in light of recent RCT evidence. This will inform future practice and help improve patient outcomes following LLA.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;4(1):48-51
Publication date:
November 22, 2024
Author Affiliations:
1. Academic Vascular Surgical Unit, Hull York Medical School, Hull, UK
2. Hull University Teaching Hospitals, Hull, UK
3. York and Scarborough Teaching Hospitals, UK
Corresponding author:
WeiYing Chua
Vascular Research Office,
Allam Diabetes Centre, 2nd Floor, Hull Royal Infirmary
Anlaby Road, Hull HU3 2JZ, UK
Email: [email protected]











