ABSTRACTS
VASGBI 2023 Brighton oral presentation abstracts
Authors of the top scoring abstract submitted are given the opportunity to give an oral presentation of their work during our free paper session. The first paper, by Suzanne Harrogate et al was awarded first prize.
A National Study of Peri-operative Smoking Cessation in Vascular Surgery
Suzanne Harrogate,1,2 Jonathan Barnes,3 Josie Watts,4 Ava Lorenc,4 Leila Rooshenas,4 Robert Hinchliffe,4,5 Ronelle Mouton2,4
1 Elizabeth Blackwell Institute, University of Bristol, Bristol, UK; 2 Department of Anaesthesia, North Bristol NHS Trust, Bristol, UK; 3 Department of Anaesthesia, University Hospitals Bristol and Weston NHS Foundation Trust, Bristol, UK; 4 Department of Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK; 5 Department of Vascular Services, North Bristol NHS Trust, Bristol, UK
Background
Smoking is the biggest cause of preventable illness worldwide1 and is associated with increased peri-operative morbidity.2 Over 30% of patients awaiting vascular surgery smoke, far higher than the general population.3
Aims
To explore smoking-cessation strategies currently offered to vascular surgery patients and to identify barriers and facilitators to the provision of peri-operative smoking-cessation practices.
Method
We designed a survey exploring anaesthetists’ knowledge, beliefs, and practice regarding smoking cessation in patients awaiting vascular surgery. The survey was piloted with 9 participants from 2 centres. After refinements, it was distributed to Vascular Anaesthesia Society of Great Britain and Ireland (VASGBI) members by email. Inductive thematic analysis of free text responses was used to identify codes, which were subsequently grouped into themes.
Results
We received 93 responses from anaesthetists representing 46 out of 67 vascular networks. Although most vascular anaesthetists (84%) ask patients about smoking, only 53% regularly recommend smoking-cessation, and only 12% regularly provide specific smoking-cessation interventions. Most anaesthetists (57%) have no formal training in smoking-cessation interventions while 77% are not familiar with the current NICE smoking-cessation guidance. Anaesthetists who had been formally trained had mostly undertaken self-directed learning in Very Brief Advice (34%).
In keeping with research evidence and institutional guidance, most anaesthetists surveyed believe that any degree of preoperative smoking-cessation is beneficial (82%). However, belief in the detrimental impact of smoking-cessation before surgery persists: 15% agreed with the statement that smoking cessation “too close” to surgery is harmful, while 7% felt that perioperative use of nicotine replacement therapy could cause harm.
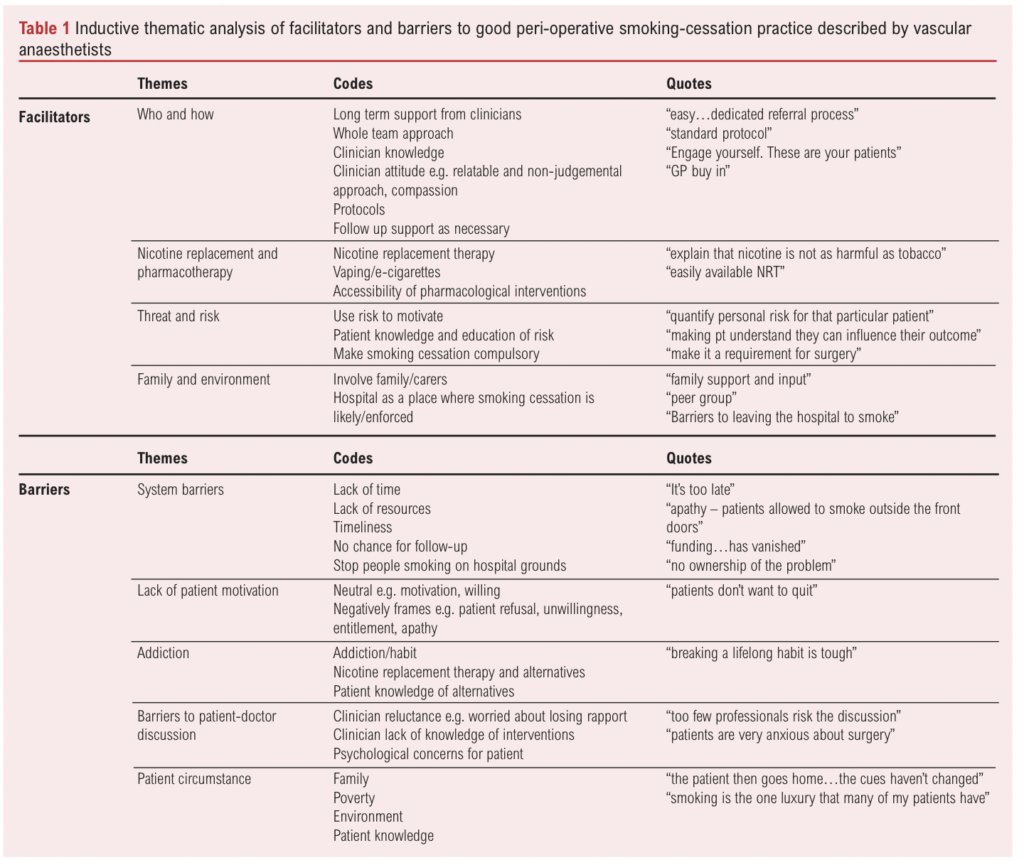
Respondents described barriers they felt prevented them from implementing smoking-cessation interventions periopertively, and facilitators of good smoking-cessation practice. Themes identified from these responses are listed in table 1, alongside exemplar codes. Themes for barriers were system barriers, lack of patient motivation, patient circumstances, addiction, and barriers to the patient-doctor discusson. System barriers, such as lack of time and resources, was the most commonly coded theme. Themes for facilitators were threat and risk, family and environment, nicotine replacement therapy (NRT), and “who and how”.
Conclusion
Despite a high smoking prevalence in patients awaiting vascular surgery, there is a variation in smoking-cessation practice between anaesthetists across the vascular networks. Only half of vascular anaesthetists regularly recommend smoking-cessation to their patients. Most are not familiar with NICE smoking-cessaiton guidance, and few have any formal training in the delivery of smoking-cessation interventions. Where it exists, training is predominantly self-directed. Organisational factors and lack of patient willingness are significant barriers to the provision of effective smoking cessation support, while access to NRT and a clear, protocolised approach (the “who and how”) were facilitators of good practice.
Funding: Funding from VASGBI and the Association for Cardiothoracic Anaesthesia & Critical Care (ACTACC) via the National Institute for Academic Anaesthesia (NIAA).
References
1. Khan J. The Khan review: making smoking obsolete. 2022, Office for Health Improvement and Disparities
2. Grønkjær M, et al. Preoperative Smoking Status and Postoperative Complications: A Systematic Review and Meta-analysis. Annals of Surgery 2014;259(1).
3. Waton SJ, et al.,https://www.vsqip.org.uk/content/uploads/2022/11/NVR-2022-Annual-Report.pdf
The development of a Vascular Post Anaesthesia Care Unit (PACU) in the Royal Victoria Hospital, Belfast – Our experiences and outcomes to date
Colin Munn,1 Sinead McGuirk2
1 ST7 Anaesthetist, RVH Belfast, Northern Ireland; 2 Consultant Anaesthetist, RVH Belfast, Northern Ireland
Background
High risk non-cardiac surgery represents 12.5% of all surgical procedures, however it accounts for a disproportionate rate of peri-operative morbidity and mortality.1,2 Vascular surgical patients in particular represent a complex patient cohort undergoing high risk surgery. Belfast is one of the busiest tertiary vascular units in the UK, performing over 50 elective open AAA repairs in 2021 despite the COVID pandemic. Our traditional model of care has been to admit these patients to our regional intensive care unit (RICU) post operatively which has ultimately led to patient cancellations and reduced theatre efficiency due to lack of elective capacity. Following on from the Bengoa Report, the Review of Surgery in Northern Ireland report was published in 2022. One key recommendation was the development of enhanced post anaesthesia care for our high risk patients in order to reduce complication and cancellation rates and to minimise the existing burden on services through improved theatre efficiency, reduced length of hospital stay and reduced burden on critical care, which currently operates at a greater than 95% bed occupancy rate.3
Aims
We set about establishing PACU by defining our key goals, which were to ensure the new unit provided time limited, enhanced, intermediate level care within our pre-existing recovery unit for elective patients.
Methods
A local steering group was formed including management, medical and nursing teams. We put in place governance structures and commenced a pilot scheme where one vascular surgical patient per week was identified for admission into PACU. Alongside our pilot we developed a standard operating procedure, drafted a successful business case for submission to the Department of Health NI, devised a user friendly booking system and data collection procedures. Following a hugely successful pilot scheme and release of funding we have now expanded to facilitate four PACU beds per day across all surgical specialties, with multidisciplinary input.
Results
Our results have demonstrated a positive impact across numerous quality indicators. Vascular theatre efficiency has improved, particularly for those undergoing open AAA repair or aorto-bifemoral bypass surgery where there has been a 66% reduction in delays prior to surgery commencing due to lack of ICU bed capacity, and a subsequent 50% reduction in vascular theatre session over-runs, thus increasing capacity for other vascular procedures. There has also been a 50% reduction in patient cancellations due to lack of ICU capacity for those undergoing open AAA or ABF repair. Our impact on critical care has also been noted with a significant reduction in planned vascular admissions, translating into reduced bed pressures through an estimated saving of 3 critical care beds per week. We have also demonstrated a reduction in high dependency outliers within our recovery ward which has further improved theatre and recovery flow. We are providing safe care to our PACU patients, with an escalation rate to critical care of only 2% and no reported adverse incidents to date. This has been achieved in a cost effective manner, with a PACU bed costing approximately 10% of a critical care bed per 24 hour period. Feedback from patients and staff alike has been very positive.
Conclusion
In summary, we have shown that our PACU service is delivering safe, quality care to a complex surgical cohort whilst improving theatre efficiency, reducing cancellations and the burden on our critical care department.
References
1. Pearse RM, Harrison DA, James P, Watson D, Hinds C, Rhodes A, Grounds RM, Bennett ED: Identification and characterisation of the high-risk surgical population in the United Kingdom. Crit Care 2006;10(3):R81-10.1186/cc4928.
2. Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, Vallet B, Vincent JL, Hoeft A, Rhodes A: Mortality after surgery in Europe: a 7 day cohort study. Lancet 2012;380(9847):1059-65. 10.1016/S0140-6736(12)61148-9.
3. Review of General Surgery in Northern Ireland, Standards and a way forward. www.health-ni.gov.uk.
Observational analysis of the affect of national lockdown on the cardiopulmonary fitness of patients being assessed for aortic surgery
Ian JB Young,1 Mysoon Alabdah,1 Anna Dickson,2 Euan McGregor1
1 Department of Anaesthesia, Critical Care and Pain Medicine, Royal Infirmary of Edinburgh, Edinburgh, UK. 2 The University of Edinburgh.
Background
Since 2010, all patients assessed for open or endovascular aortic surgery at the Royal Infirmary of Edinburgh undergo cardiopulmonary exercise testing (CPET) as part of their preoperative assessment. The role of CPET in preoperative assessment is built on three premises. First, that training improves cardiopulmonary fitness.1 Second, that improved cardiopulmonary fitness is reflected in better CPET performance. Third that better CPET performance is reflected in better operative outcome.2
That training improves cardiopulmonary fitness is well demonstrated in athletic training. Broadly however, the patients we see do not do a lot of regular training. They are reliant on activities of daily living for the majority of their daily exercise.
With this in mind, we thought the period of national lockdown associated with the SARS-CoV-2 pandemic might provide an interesting observational window into whether, if you legislate to curtail activities of daily living, do our patients perform less well in CPET.
Aims
We wished to observe the impact of national lockdown on the cardiopulmonary fitness of those assessed for aortic surgery at the Royal Infirmary of Edinburgh (RIE). We hypothesised that behavioural changes during this time might negatively affect cardiopulmonary exercise testing (CPET) results.
Method
We performed a retrospective observational analysis on 714 patients undertaking CPET in the vascular pre assessment clinic at the RIE. 486 patients assessed before lockdown between January 2010 and December 2015, 110 assessed closely following lockdown between July 2021 and August 2022, and 118 assessed after lockdown between August 2022 and May 2023. We compared maximal oxygen consumption ml/kg/min (VO2), oxygen consumption at anaerobic threshold ml/kg/min (AT), and ventilatory efficiency at anaerobic threshold (VE/VCO2). These values are all associated with postoperative survival after aortic surgery.3 Analysis was performed in R version 4.2.2. Values are mean (SD).
Results
Pre, affected by, and post lockdown groups were similar at baseline. Mean group age (68-70), BMI (27-28), Resting heart rate (77-81), Resting blood pressure (124/74-130/79). The group affected by lockdown showed evidence of a statistically significant reduction in VO2 (14.7(4.3) vs 16.3(4.2) p < 0.001), AT (10.4(2.3) vs 11.7(2.5) p < 0.001), and increase in VE/VCO2 (38.0(7.6) vs (34.0(5.6) p < 0.001) compared to the pre lockdown group (figure 1). When compared to average CPET results for patients attending vascular pre assessment at the RIE, these differences represented a 12 centile shift in VO2, 17 centile shift in AT, and 21 centile shift in VE/VCO2 (figure 2). These differences had dissipated in the group assessed at least one year post lockdown.
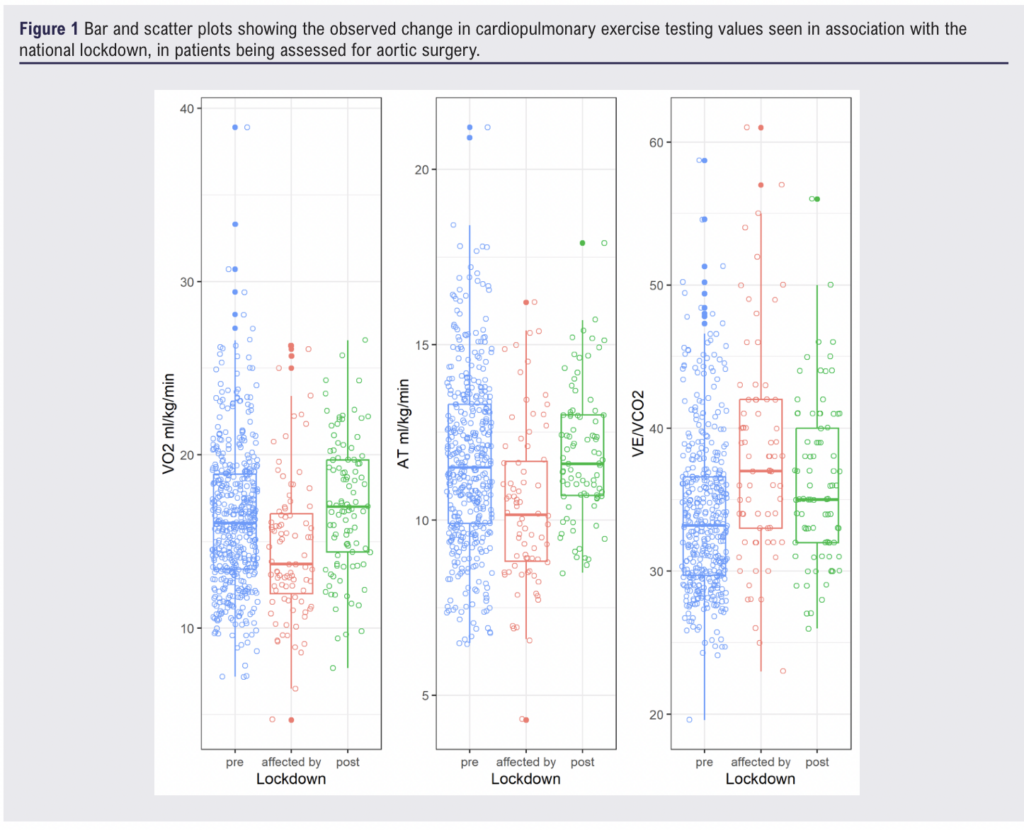
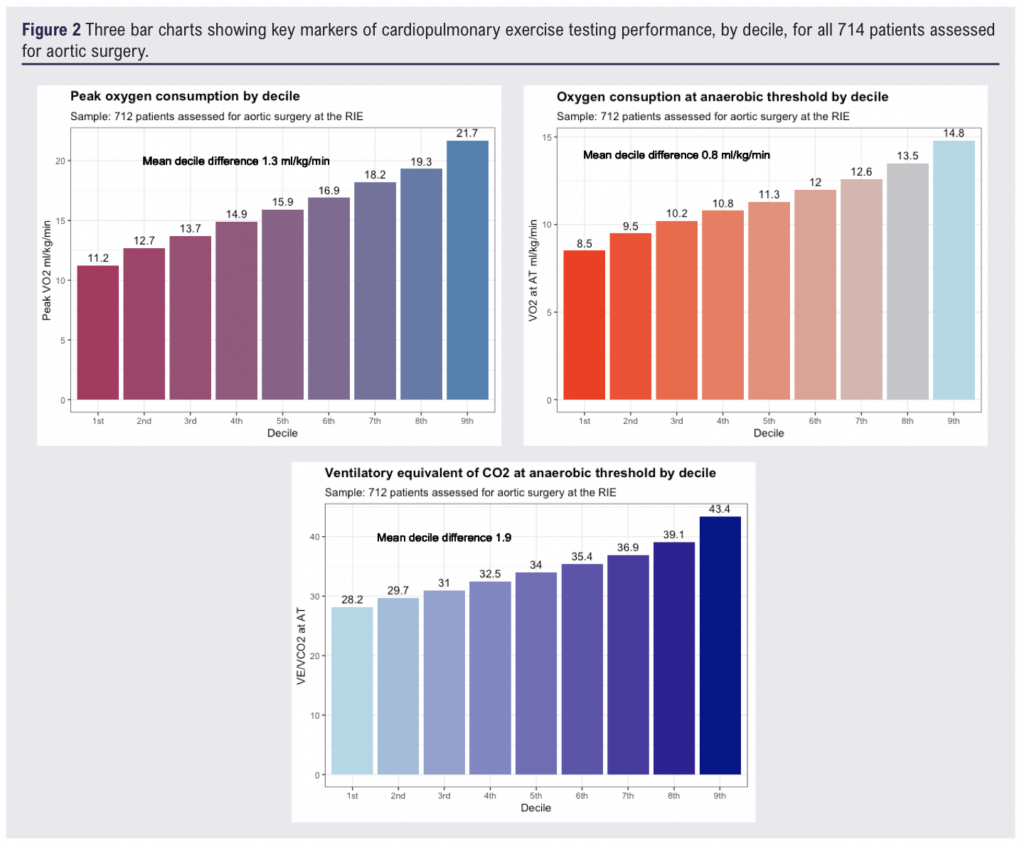
Conclusion
This retrospective observational cohort shows a significant reduction in key markers of cardiopulmonary fitness following the period of national lockdown. While absolute differences may appear small, they represent a 10-20 centile shift when compared to the population of patients who attend the RIE in the context of assessment for aortic surgery. In these data the observed difference did not persist more than one year after national lockdown. Fitness is maintained by activities of daily life. When these are constrained by public health measures, we should be cognisant of the impact on patients preparing for surgery and continue to encourage prehabilitation where possible.
References
1. Banugo, P, Amoako D. Prehabilitation. BJA Education 2017;17:401-05
2. Moran J, Wilson F, Guinan E, McCormick P, Hussey J, Moriarty J Role of cardiopulmonary exercise testing as a risk-assessment method in patients undergoing intra-abdominal surgery: a systematic review. British Journal of Anaesthesia 2016;116:177-191
3. Carlisle J, Swart M. Br J Surg 2007;94:966-9.
Preoperative thrombin generation is correlated to intraoperative blood loss in open aortic surgery
Neill S Aitken,1 Ian JB Young,1 Yesim Dargaud,2 Alastair F Nimmo1
1 Department of Anaesthesia, Critical Care and Pain Medicine, Royal Infirmary of Edinburgh, Edinburgh, UK 2 Haemophilia Treatment Centre, University Hospital of Lyon and French Reference Centre on Haemophilia, Lyon, France
Background
Thrombin generation analysis (TGA) is a measure of overall coagulation capacity and reflects the combined effects of pro and anticoagulant factor concentrations. In the setting of cardiac surgery, an inverse relationship between preoperative thrombin generation and operative blood loss has been demonstrated.1,2 In major vascular surgery, we observe three components of TGA in preoperative blood samples, and their correlation to total intraoperative blood loss. We report the maximum concentration of thrombin generated, or peak thrombin; the area under the curve of thrombin generated, or endogenous thrombin potential (ETP); and the time to initiation of thrombin generation, or lag time. In TGA, a reduced lag time and higher peak thrombin and ETP represent greater coagulation capacity.3
Aim
Does an association exist between preoperative capacity to generate thrombin and subsequent operative blood loss in open aortic surgery?
Methods
These observations are part of a prespecified secondary analysis of a randomised controlled trial comparing fibrinogen concentrate to fresh frozen plasma (FFP) for management for coagulopathy during extent IV thoraco-abdominal aortic aneurysm (TAAA) surgery.4 Twenty patients had blood samples in the anaesthetic room, before induction of anaesthesia. Thrombin generation was measured in citrated platelet poor plasma samples and triggered with 5pM tissue factor. Data was analysed using R version 4.2.2.
Results
We observe statistically significant correlations between preoperative TGA and intraoperative blood loss (figure 1). Peak thrombin (Pearson Correlation -0.53; 95% CI: -0.26 to -0.72. R2 0.28. p < 0.001), ETP (Pearson Correlation -0.35; 95% CI: -0.04 to -0.60. R2 0.12. p < 0.05), and Thrombin lag time (Pearson Correlation 0.53; 95% CI: 0.27 to 0.73. R2 0.30. p < 0.001). Total intraoperative blood loss ranged from 2650ml to 16500ml. Greater preoperative coagulation capacity was correlated with lower intraoperative blood loss.
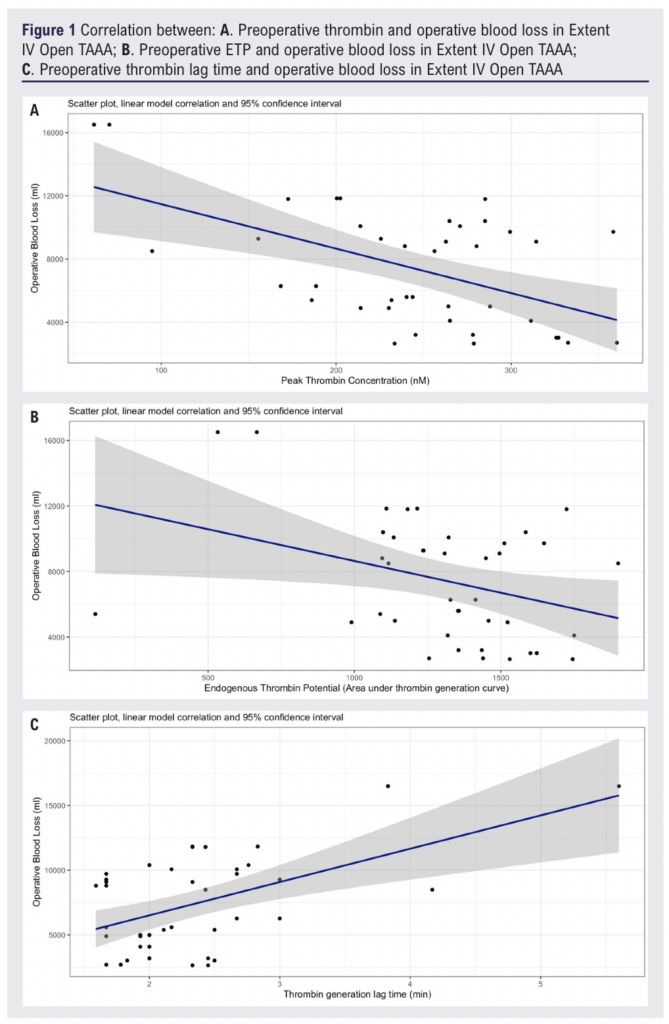
Conclusion
Coagulopathy in TAAA surgery is ubiquitous, reflecting the combined effects of blood loss, visceral ischaemia and reperfusion, hypothermia, and the administration of heparin. This observed correlation is hypothesis generating. High intraoperative blood loss, and associated blood product transfusion, is resource intensive and associated with its own morbidity. A preoperative blood test that could better predict intraoperative blood loss would be beneficial for service preparation and planning.
The original RCT on which this secondary analysis is based is registered at clinicaltrials.gov (NCT00994045). CSL Behring part funded this RCT.
References
1. Coakley M, Hall JE, Evans C, et al. J Thromb Haemost 2011;9:282-92.
2. Bosch Y, Al Dieri R, ten Cate H, et al. J Cardiothorac Surg 2013;8:154.
3. Berntorp E, Salvagno G.L. Semin Thromb Hemost. 2008;34:670–82.
4. Morrison GA, Koch J, Royds M et al. Anaesthesia 2019;74:180–9.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(3):173-178
Publication date:
May 22, 2024











