ABSTRACTS
VASGBI Annual Scientific Meeting 2024, Leeds, 9-10th September, oral presentation top abstracts
Authors of the top scoring abstracts submitted were given the opportunity to give an oral presentation of their work during our free paper session. The first paper, by Akshay Shah et al was awarded first prize.
Platelet function in patients undergoing major non-cardiac vascular surgery (PLUGS): A prospective cohort study
Akshay Shah,1 Grace Polley,2 Kasia Bera,3 Keith Maher,4 Stephen Von-Kier,4 Antonio Barbosa,4 Louis Corrigan,5 Sabeena Sharma,6 Michael Desborough,7 Stuart McKechnie2,6 on behalf of the PLUGS Investigators
1Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, UK; 2Oxford Critical Care, Oxford University Hospitals (OUH) NHS Foundation Trust, Oxford, UK; 3Department of Vascular Surgery, OUH NHS Foundation Trust, Oxford, UK; 4Haemostasis and Blood Conservation Service, Oxford University Hospitals NHS Foundation Trust, Oxford, UK; 5Wadham College, University of Oxford; 6Nuffield Department of Anaesthesia, OUH NHS Foundation Trust, Oxford, UK; 7Radcliffe Department of Medicine, University of Oxford, Oxford, UK
Background
P2Y12 inhibitors, such as clopidogrel, pose challenges to vascular anaesthetists particularly when regional/central neuraxial anaesthesia is being considered. Current guidelines recommend discontinuation of clopidogrel 5–7 days prior to major surgery to reduce the risk of bleeding, but also before attempting central neuraxial anaesthesia to mitigate the rare risk of developing a vertebral canal haematoma.1 However, guideline recommendations do not take into consideration the individual variability in pharmacodynamic responsiveness to clopidogrel. Approximately 32% of patients on clopidogrel may be non-responders.2 The leading question in a VASGBI research priority setting exercise was – “Can regional anaesthesia safely be performed on patients taking clopidogrel and similar antiplatelet agents?”.
Aims
The aim of this study was to characterise platelet function in patients undergoing vascular surgery using near-patient viscoelastic testing (Thromboelastography (TEG®) 6S).
Methods
PLUGS was a single-centre, prospective, non-interventional cohort study conducted at the John Radcliffe Hospital, Oxford, UK. The study was prospectively registered (ISRCTN11959105). Inclusion criteria were: (i) age >18 years; (ii) scheduled to undergo vascular surgery (carotid endarterectomy, abdominal aortic aneurysm (open or endovascular), lower limb arterial revascularisation and lower limb amputation); and (iii) established on antiplatelet therapy for at least 7 days before entering the study. Study-specific blood samples were collected at pre-operative assessment clinic (POAC) visit and on the day of surgery. Baseline demographic, laboratory procedure-related, and clinical outcome data were collected for each participant. The primary outcome of interest was the proportion of patients with antiplatelet drug resistance at (i) initial presentation to POAC and (ii) on the morning of the surgery.
Results
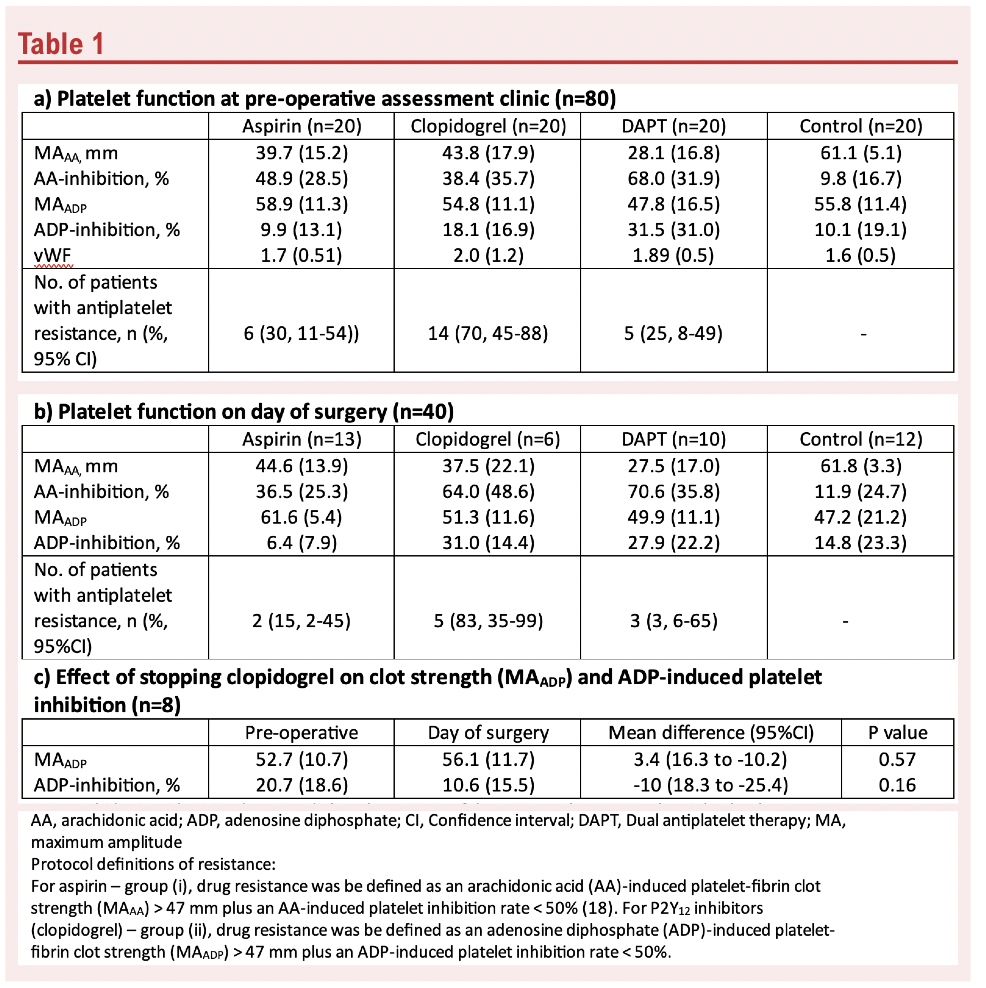
Between 9 June 2022 and 17 April 2023, 80 participants were enrolled of which 64 proceeded to have surgery. The mean (SD) age was 71.7 (12.1) years, and 69 participants were male. Fifty-two participants had >2 pre-exisiting comorbidities. The commonest operation was abdominal aortic aneurysm repair (n=25) followed by carotid endarterectomy (n=20). The proportion of patients with antiplatelet resistance at POAC ranged from 25% to 70% (Table 1a). Approximately three-quarters of patients taking clopidogrel displayed antiplatelet resistance. Medication compliance was generally good with only four patients forgetting to take their medications (on 1-2 days) in the preceding two weeks. On the day of surgery, the proportion of patients with antiplatelet resistance ranged from 15.3 to 83.3% (Table 1b). In an exploratory analysis, stopping clopidogrel 5-7 days before surgery demonstrated no statistically significant changes in platelet clot strength and ADP-induced platelet inhibition (Table 1c).
Conclusion
This study confirms a high prevalence of antiplatelet, particularly clopidogrel, resistance.3 This combined, with the introduction of CYP2C19 genotype testing, offers an opportunity for precision-based medicine in vascular surgery. Using our approach, a large, adequately powered, multicentre study is feasible to confirm our findings and to clarify the role of resistance testing on clinical outcomes.
Acknowledgements: This study was funded by a NIAA/VASGBI Trainee Research Development Grant awarded to A.S. (WKRO-2020-0017). We would like to thank the following PLUGS Investigators for assisting in the recruitment of study participants – Jean Wilson, Neil Davidson, Soyamol Matthews, Sally Beer, Jenny Buisan, Beatrice Vidotto, Ping Zhang, Pam Davies.
References
1. Horlocker TT, Vandermeuelen E, Kopp SL et al. RAPM 2018;43(3):263-309
2. Krishna V, Diamond GA, Kaul S. Circulation 2012;125(10):1288-303
3. Kim Y, Weissler EH, Pack N, et al. Ann Vasc Surg 2023;91:257-265
A single institute, 3-year, service evaluation of outcomes for carotid endarterectomy using general or regional anaesthesia techniques
Hew D Torrance, Eoin O’Rathallaigh, Holly-India Esam, Pawandeep Sarai, Sadie Syed
Department of Anaesthesia, St Mary’s Hopsital, Imperial College Healthcare NHS Trust.
Following the completion of the GALA study in 20081 controversies still exists among vascular units regarding the preferred anaesthetic technique for carotid endarterectomy (CEA).
As part of a service evaluation, patients undergoing CEA at St Mary’s Hospital, Imperial College Healthcare NHS Trust, were retrospectively analysed between December 2019 and December 2022. Aims were to compare these data to the National Vascular Registry (2021)2 and to explore if anaesthetic technique influenced duration in recovery, use of postoperative vasopressors or admission to critical care. Analysis was performed using R v.4.0.0.
One hundred and forty-seven patients were identified (Table 1), 72% male (n=106), median age 71 (IQR 64-78), 86% (n=126) suffered an acute stroke or transient ischaemic attack (TIA). Median duration from symptoms to surgery was 12 days (IQR 7-25), mirroring national data (13 days, IQR 8-22).2
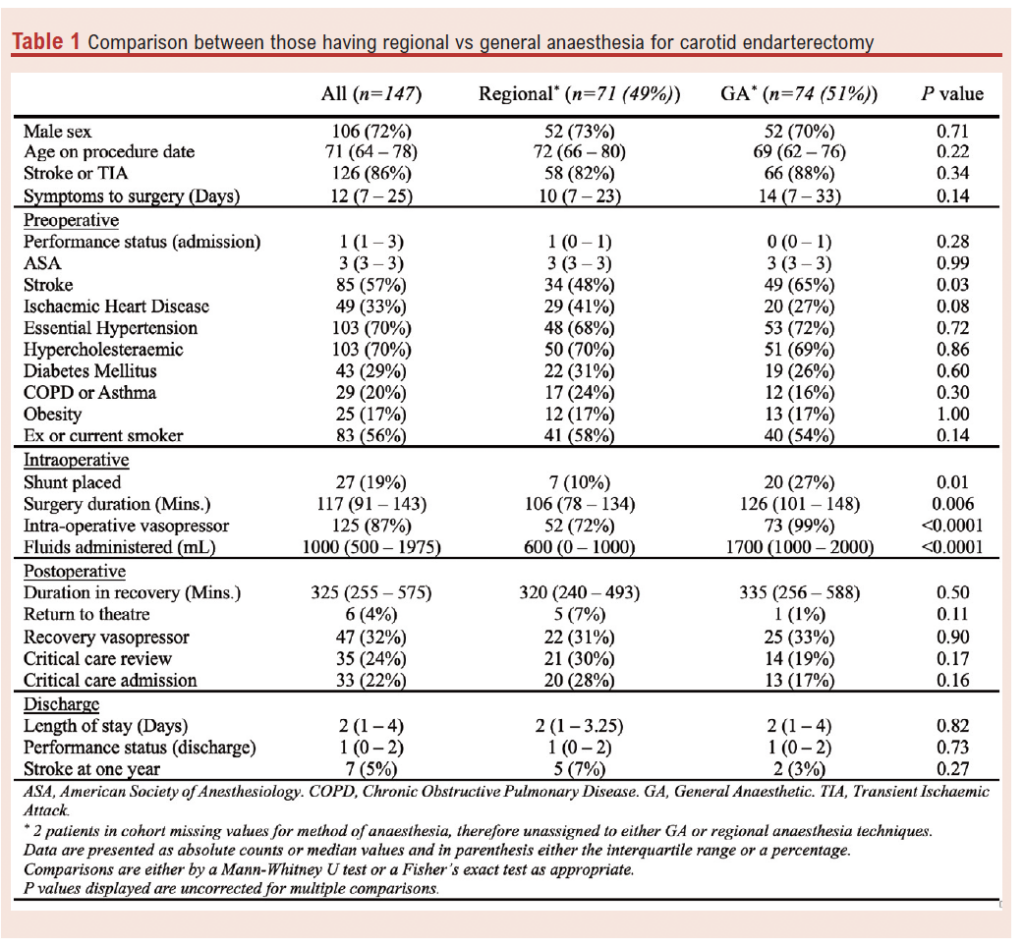
General anaesthesia (GA) accounted for 51% of cases with the remainder performed under regional anaesthesia (RA), (79%, intermediate and 21%, deep cervical plexus). 30% performed under GA also included a regional component. This was in stark contrast to national data with 64% of cases being performed under GA alone, 11% under GA with a block or local anaesthetic (LA) component and only 18% were performed under block alone.
No differences were identified in the incidence of preoperative hypertension, hypercholesterolaemia, diabetes mellitus, chronic lung disease, obesity or smoking status in RA or GA. However, GA patients trended towards a reduced incidence of preoperative ischaemic heart disease, 27% vs 41% (P=0.08), but an increased incidence of preoperative stroke, 65% vs. 48% (P=0.03). Our institution rarely utilised shunts (19%), compared to national data (64%). Shunt usage was reduced in RA, 10% vs 27% (P=0.01). In those patients undergoing GA, 67% had concomitant near infrared spectrophotometry monitoring documented.
Surgery duration was reduced in RA patients (P=0.006), they also received less intraoperative fluid (P<0.0001) and were less likely to require intraoperative vasopressors (P<0.0001). No differences were detected when comparing duration in recovery or postoperative vasopressor requirements. There were no statistical differences in return to theatre rate (7% vs. 1%, P=0.11), or critical care admission (28% vs. 17%, P=0.16) when comparing RA to GA.
The length of stay and discharge performance status was consistent between RA and GA; at one year there was no statistical differences in incidence of stroke (7% vs. 3%, P=0.27).
In this hypothesis generating service evaluation, despite our unit using differing anaesthetic strategies to published national data, we demonstrated similar outcomes. Anaesthetic choice did not appear to influence use of vasopressors in recovery, duration in recovery or admission to critical care, although this may be affected by study power. These data may reflect the conclusions from the pragmatic GALA trial illustrating that major perioperative outcomes after CEA are broadly similar between RA and GA and are reflective of unit experience and expertise.
References
1. GALA Trial Collaborative Group. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet. 2008;372:2132-42.
2. Waton S, Johal A, Birmpili P, et al. National Vascular Registry: 2022 Annual Report. London: The Royal College of Surgeons of England, November 2022.
Inter-test reliability of point of care platelet function tests: comparison of multiplate and TEG platelet mapping in patients with peripheral arterial disease taking clopidogrel
Dr Mark Parson, Dr Vanessa Fludder, Dr Jia Liu Stevens
Department of Anaesthesia, Royal Sussex County Hospital, University Hospital Sussex NHS Foundation Trust, Eastern Road, Brighton, BN2 5BE, UK
A high proportion of patients with peripheral arterial disease (PAD) take clopidogrel as a routine antiplatelet. For patients undergoing vascular surgery, neuraxial anaesthetic blockade (NAB) is typically preferred over a general anaesthetic due to concurrent patient illness. Current guidance suggests omission of clopidogrel for 5-7 days for NAB, which may not be feasible for emergency surgery. A proportion of the population have a genetic polymorphism in clopidogrel metabolism, resulting in a reduced antiplatelet effect, contributing to High on Treatment Platelet Reactivity (HTPR). These patients potentially could have NAB earlier than 7 days; however, this requires accurate and reproducible point of care (POC) testing of platelet function, this currently is an under investigated area, with no common consensus on a reliable POC cut-offs. Our study primarily aims to determine the degree of correlation between TEG-6S PlateletMapping (PM) and Rotem Multiplate (RM) POC analyser and the proportion of patient suitable for NAB using surrogate HTPR cut-offs from cardiac anaesthesia, with a secondary aim to determine any difference in platelet inhibition between a cohort of ward and clinic patients.
We conducted a single-centre, prospective cross-sectional study of vascular ward and claudication clinic patients at the Royal Sussex County Hospital (Brighton, UK). Venous blood was obtained and analysed by both RM and PM. Baseline demographic and clinical data was collected prospectively. The study gained ethical approval from London – Fulham Research Ethics Committee. Informed consent was obtained from participants.
Sixty patients were recruited, 68% were male; the median age was 68 years. We found a moderate correlation from the two analysers for paired samples (R=0.63, P<0.001)). Using published consensus cut-off values for HTPR of area-under-the-curve (AUC) 46U for RM and maximum amplitude (MA) 47mm. 67.7% of RM and 69.5% of PM measured patients were safe to proceed with NAB. No difference was found in in AUC or MA between ward and patients, however fibrin was higher in ward patients compared to clinic (17.0 versus 12.6, P=0.003), in addition AUC was found to be higher in females versus males (78 and 61U respectively, P=0.049). Statistical analyses was carried out using GraphPad Prism 8 software.
Guidelines regarding the role of platelet testing in peri-operative decision making exist in relation to cardiac surgery, but not yet for use of NAB in vascular surgery.1 Our finding suggests that there may be a high proportion patient suitable for safe NAB whilst taking clopidogrel, however variability in POC results remain which adds uncertainty in identification of these patients. Further work is required in this field. This maybe the first step in developing a personalised antiplatelet management for patients needing vascular surgery.
References
1. Kong R, Trimmings A, Hutchinson N, Gill R, Agarwal S, Davidson S, et al. Consensus recommendations for using the Multiplate ® for platelet function monitoring before cardiac surgery. Int J Lab Haematomolgy. 2015;37:143–7.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;4(1):52-54
Publication date:
November 27, 2024











