ORIGINAL RESEARCH
What’s the denominator? An 8-year audit of ruptured abdominal aortic aneurysm outcomes, including rates of conservative and palliative management
Sharma A,1 Bergman H,2 Lane TRA2
Plain English Summary
Why we undertook the work: A ruptured abdominal aortic aneurysm (rAAA) happens when the main blood vessel in the body bursts. It is a life-threatening emergency. Surgery is in almost all cases the only treatment. Not everyone is able to survive surgery. Doctors often need to make quick decisions with little time. There are two main types of repairs – open repair and a less invasive method called endovascular repair (EVAR). Many studies compare these treatments. However, there is less focus on those who are too unwell and instead receive comfort care (those who do not have surgery). We wanted to learn more about these patients and their outcomes.
What we did: We looked at hospital records for all cases of rAAA treated at Addenbrooke’s hospital between January 2015 and November 2022. We looked at how patients were treated (open repair, EVAR or no repair), their outcomes, and other factors like scans, blood transfusions, and how long they stayed in hospital.
What we found: We found 209 cases of rAAA. About 44% of patients had open surgery, 36% had EVAR, and 20% received no repair. Open repair had higher risks, with more deaths, longer hospital stays, and a greater need for blood transfusions compared to EVAR. Open repair was associated with more surgeries in the short term, while EVAR often required more surgeries in the long term. Some patients who were treated without repair survived for over a year, though this was rare, and most died.
What this means: The patients that underwent EVAR, based on suitability, had better results in the short term. Most studies focus on surgery, but our findings highlight that around 1 in 5 patients are treated without any repair. Including this group in reports can help to ensure that doctors make better decisions about treatment and set clearer standards for the rate of intervention.
Abstract
Background: A ruptured aortic aneurysm (rAAA) is a surgical emergency with rapid onset and poor survival. Expedited diagnosis and surgical repair are required to prevent exsanguination. Extensive literature compares outcomes of endovascular and open repair but there is little discussion of the denominator – the patients undergoing non-operative palliative management. Without this, all reported outcomes are confounded by case selection. We carried out this review to learn more about those operated on and to include the rate of palliation to learn more about overall outcomes.
Methods: A retrospective note review of the electronic patient record identified all rAAAs treated at Addenbrooke’s hospital between January 2015 and November 2022. Demographics, treatment strategy, mortality, pre-operative imaging, transfusion requirement and inpatient stay were interrogated.
Results: There were 209 rAAAs identified. Management was with open surgery (44%), endovascular surgery (36%) and palliation (20%). Open repair was associated with higher mortality, longer inpatient and ITU stay, and larger transfusion requirements than endovascular repair. Open repair was associated with a higher rate of return to theatre in the short term, while endovascular repair (EVAR) had a higher rate in the long term. 7% of palliative rAAAs remained alive at one year.
Conclusions: An EVAR-first approach results in lower mortality rates and better short-term outcomes. Although interventional outcomes are widely reported, approximately 20% of the caseload is palliated. This denominator should be reported alongside conventional outcomes to address the bias of case selection and resource allocation and to provide a more comprehensive picture of overall outcomes.
Introduction
In the UK, more than 4,900 deaths annually are attributed to aortic pathologies,1 with aneurysms and dissections being the leading causes, particularly in men over 65. Aneurysms, often undetectable until rupture, are at higher risk of rupturing if they exhibit pain, increase in size by more than 1 cm/year or have diameters larger than 5.5 cm, prompting elective surgical repair. Surgical intervention, either through open surgery or endovascular approaches, is the primary treatment for ruptured abdominal aortic aneurysms (rAAAs). The shift towards endovascular repair (EVAR), supported by the IMPROVE study, reflects its short-term benefits over open repair, such as fewer complications and shorter hospital stays, despite long-term risks like endoleaks and the necessity for revision surgery.2-4 Addenbrooke’s hospital follows an ‘EVAR first’ strategy, being able to provide EVAR 24 hours a day, seven days a week in a dedicated hybrid operating suite, with round-the-clock vascular and interventional radiology coverage, adequately supported by a high-power ITU.
Literature often focuses on the effectiveness of interventions, with the intervention decision being complex and reliant on consensus among the patient, surgeon and anaesthetist. The variance in intervention strategies among centres could lead to perceived outcome disparities, suggesting potential selection bias in reported outcomes.
This report presents an 8-year overview of rAAAs at a tertiary centre, providing data on both palliated and treated patients to provide a comprehensive evaluation of the unit’s outcomes.
Methods
Local service evaluation and audit approval were sought through the Cambridge University Hospitals NHS Foundation Trust Research and Development department (Registration number PRN10943). Cambridge Vascular Unit, based at Addenbrooke’s Hospital, Cambridge is a tertiary vascular referral centre serving an immediate population of approximately 1.8 million and regional complex services for 4 million. Hospitals included in this region are Peterborough Hospital, West Suffolk Hospital, Bedford Hospital and Hinchingbrooke Hospital. The distribution of the population in these spoke hospitals is shown in Figure S1 (see Appendix online at www.jvsgbi.com).
A retrospective case note review was performed via the EPIC – Hyperspace patient management platform (Epic Systems Corporation, Verona WI, US) to elicit all patients with ruptured aortic aneurysms at Addenbrooke’s hospital (according to the International Statistical Classification of Diseases, ICD-10), discharged between 01/01/2015 and 30/11/2022. Patients with a previous aortic aneurysm were excluded to analyse primary ruptured aortic aneurysms only. Data were collected from 01/03/2023 to 30/04/2023. Baseline patient demographics including postcode, date of birth (DoB), gender and age were recorded.
Mortality status was interrogated for all patients to determine the date of death (DoD), post-procedure days to death and the 30-day, 90-day and 1-year mortality status. Where mortality data were missing, the NHS inter-hospital data spine, connected to all local hospitals and GP practices, was interrogated to provide mortality data for non-hospital registered patients. When available, the cause of mortality was analysed from registered death certificates.
Pre-specified group analysis was done analysing individual outcomes for open and EVAR surgeries, including the amount of blood transfused intra-operatively and the recovery time and level of care required. The rate of and reason for return to theatre due to complications in the short and long term were inspected. Previous interventions, co-morbidities and average aneurysm size were examined.
All statistics and graphical representations were produced on Microsoft Excel (V16.79.1 Microsoft, Redmond, WA, USA), the SPSS platform (V29.0.1.0, Armonk, NY, USA), and GraphPad Prism (V10.1.2, Boston, MA, USA). Statistical methods involved normality assessment, Chi-squared test for comparison of all groups, unpaired t-test (if parametric data) and Welch’s unpaired t-test (if non-parametric data) to compare open vs EVAR, and one-way ANOVA to compare all groups. ArcGIS (V10.6.1 Redlands, CA, USA) was used to plot geographical spread.
Results
Study cohort
209 cases of ruptured AAAs were identified over the 8-year period (approximately 26 cases per year). There were 91 (44%) and 76 (36%) cases of open and EVAR surgery, respectively. 42 patients (20%) were palliated with no surgical intervention. 77 cases presented to Addenbrooke’s hospital first. Of these cases, 32 (41.6%) underwent open repair and 18 (23.4%) underwent EVAR. A total of 27 patients were palliated (35.1%). A total of 132 cases presented to a ‘spoke’ site first, of which 82 were from Peterborough and Hinchingbrooke Hospitals, 27 from West Suffolk Hospital, 8 from Colchester Hospital, and 14 from other areas.
Cohort analysis
Demographics
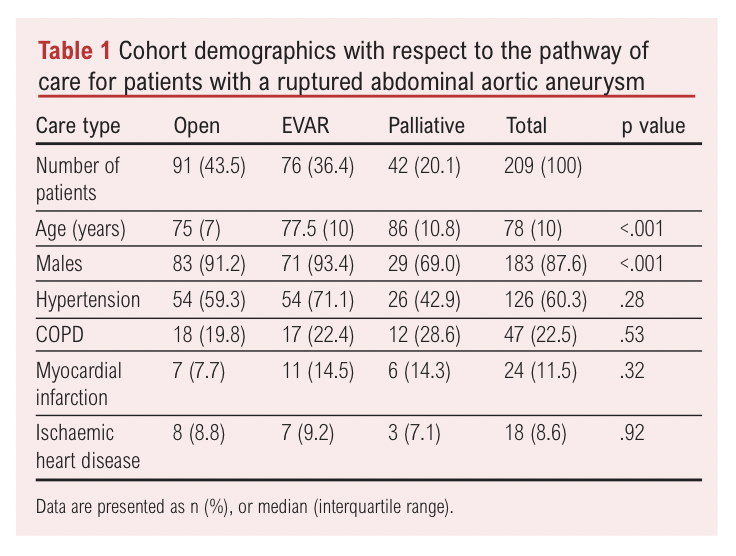
Gender and average age, given in Table 1, were both significantly different between the groups (gender p<.001, age p<.001). The median age was 75 years (7 [IQR]) and 77.5 years (10 [IQR]) for open surgery and EVAR, respectively. However, the average age of palliated individuals was 86 years (10.8 [IQR]). Of those undergoing open repair, 8.8% were female, while EVAR was 6.6%. 31.0% of palliated patients were female. The geographical spread of referrals within the East of England is demonstrated in Figure S1 (see Appendix online at www.jvsgbi.com).
The decision for surgery is a multidisciplinary team decision involving the surgeons, anaesthetists and critical care team, taking into account the chance of surviving surgery, the chance of long-term recovery, and the perceived quality of life benefit. The main reason for palliation in 33 (78.6%) cases was unsuitability for surgery. In seven cases, it was due to patient choice. Lastly, two patients, who had already been admitted to hospital, had point of care ultrasound (POCUS) but were too unstable and died on the ward. 22 (53.4%) of the palliated patients were known to have an AAA and had previously declined surgery.
Co-morbidities
The three most common co-morbidities were hypertension (HTN), chronic obstructive pulmonary disease (COPD) and myocardial infarction (MI), as shown in Table 1. Some 59.3%, 71.1% and 42.9% of open, EVAR and palliated patients had HTN registered as a co-morbidity. For the same groups, 19.8%, 22.4% and 28.6% had COPD. The prevalence of remaining comorbidities is shown in Table 1. The only significant risk factors were chronic kidney disease (p<.001) and female gender (p=<.001).
Mortality
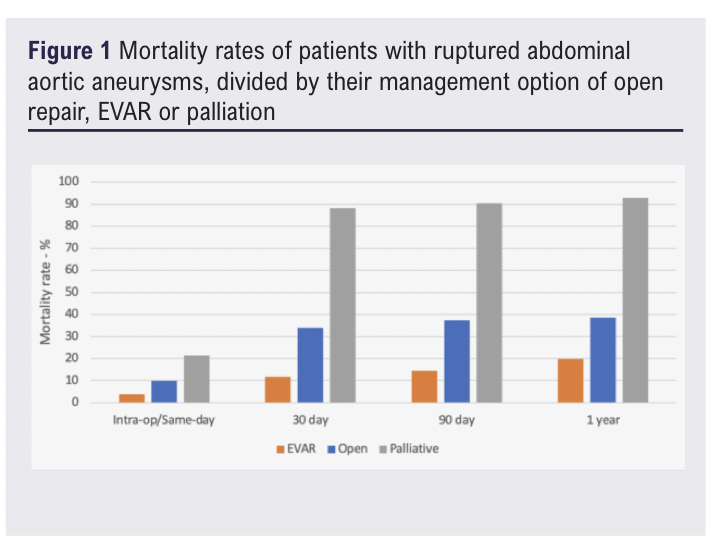
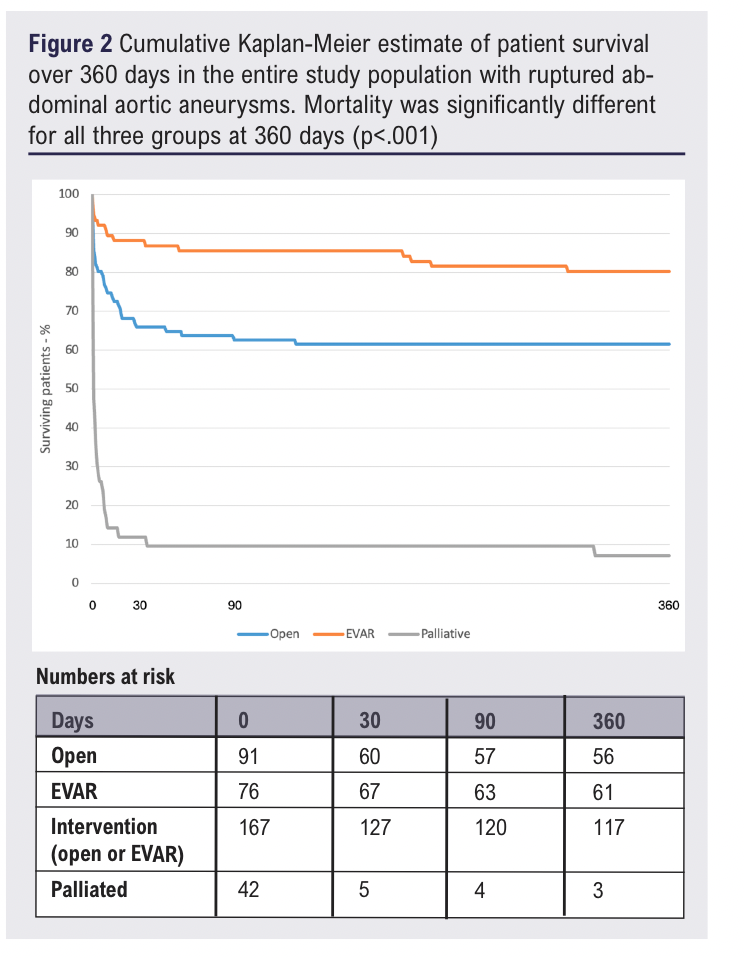
Mortality for all patients with a ruptured AAA, for intra-operative (intra-op) or same-day, 30-day, 90-day and 1-year timescales was 10%, 37%, 40% and 43%, respectively. Open repair carried a mortality risk of 10%, 34%, 37% and 38%, while EVAR had a mortality risk of 3%, 12%, 15% and 20%. Mortality for palliated patients was 21%, 88%, 90% and 93%. This is shown in Figure 1. Of the three palliated patients that survived over a year, one was noted to have a contained rupture, while the reason for survival for the other two patients cannot be ascertained. Mortality of open repair vs EVAR vs palliated patients was significantly different (p<.001) at 30 days, 90 days, and 1 year, as shown in Figure 2.
 Temporal trends
Temporal trends
Caseload
The overall trendline of cases appears to be decreasing, though the number of cases is variable, as shown in Figure S2 (see Appendix online at www.jvsgbi.com) and Table 2. The number of cases operated on appears to follow the trend of the caseload. Open operations were more frequent overall, with 91 carried out compared to the 76 EVAR surgeries. In 5 out of 8 years, open surgery was more frequent.
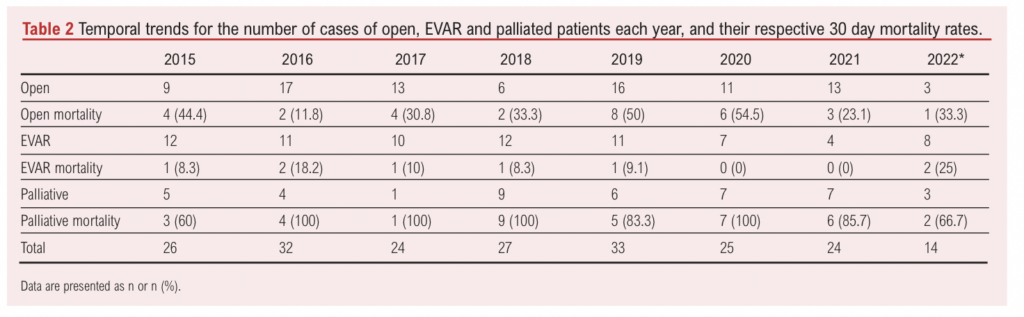
Mortality
Temporal trends in mortality were analysed over the 8-year period. Table 2 and Figure S3 (see Appendix online at www.jvsgbi.com) show the temporal trends for 30-day mortality. The overall mortality of open repair appears to be slightly increasing, though it is highly variable due to the low number of cases each year. For EVAR the overall mortality rate is again variable.
Pre-operative imaging
All patients with a suspected rAAA will first have a POCUS to confirm the diagnosis. All patients who underwent EVAR had a CT scan before the operation. 15 (16.5%) of the patients who underwent open repair were too unstable and only had POCUS before surgery. In one case, aneurysm size identified by POCUS contraindicated EVAR.
EVAR is the first-line option in our unit, and therefore the reason for open repair was analysed. Twenty-four (26.4%) of the patients undergoing open repair were deemed too haemodynamically unstable for EVAR, 10 of whom had a CT scan, with the other 14 only receiving POCUS. A further 49 (53.8%) patients were deemed to have unsuitable aneurysm anatomy for EVAR, mainly determined by its location and the structure of the neck. Six cases were initially planned for EVAR, though were changed to open repair before the operation started as the patient became more unstable. Two cases received open repair due to patient choice. For 10 cases the reason for open repair could not be ascertained.
For EVAR, open and palliated patients, the average aneurysm size was 73.8mm ± 22.6 (SD), 84.7mm ± 20.4 (SD), and 81.0mm ± 19.5 (SD), respectively (p=.017).
Return to theatre
Owing to the complexity of the operations, return to theatre is relatively common. Open operations have a rate of return to theatre in-hospital of 25.3%, of which 5.5%, 14.3% and 5.5% required 1, 2 and 3 returns to theatre, respectively. EVAR had a significantly lower in-hospital return rate of 10.5% (p=.012), with no patients having to return to theatre more than once. Overall, 52 additional surgeries were done, 43 for open repair and nine for EVAR. The reasons for return to theatre are shown in Table 3.

Long-term re-intervention rates which occurred post-discharge were also analysed. Three (3.3%) cases of open repair required re-intervention related to vascular issues. However, 15 (19.7%) cases of EVAR required later intervention (p=<.001). Following open repair, long-term re-interventions included EVAR relining of the graft (n=1), thoracic EVAR (n=1) and revascularisation operations (n=1). No midline hernia repair surgeries were recorded. For EVAR, three patients required two interventions though none required three. The reasons for re-intervention were another EVAR (n=2) or EVAR relining (n=3), revascularisation (n=7) pseudoaneurysm repair (n=3), wound explorations (n=2) and amputation (n=1).
Recovery
The average time spent in the hospital was 15 (21.25 [IQR]) and 8 (9.5 [IQR]) days for open and EVAR surgery, respectively (p<.001). All patients first began in level 2 or 3 care after surgery, before they were either discharged from the hospital or de-escalated to a lower level of care. 17% and 83% of open surgery patients entered level 2 and 3 care, respectively, while for EVAR this was 19% and 81%.
The total time spent on wards is shown in Figures S4 and S5 (see Appendix online at www.jvsgbi.com), according to whether patients initially entered level 2 or 3 care post-operatively, respectively. This excludes patients who died on the ward. If a patient post open repair initially entered level 2 care post-operatively, they would spend on average 6.5 (10.5 [IQR]) days on level 2, and a further 9.5 (7.25 [IQR]) days in hospital in level 1 care. EVAR patients initially spent on average 4 (6 [IQR]) days in level 2 care, often being discharged straight from level 2 care. Following open repair, a patient entering level 3 care would spend on average 5 (7.25 [IQR]) days, and a further 9 (11.5 [IQR]) days in lower level care. EVAR patients entering level 3 care would spend on average 1.5 (3 [IQR]) days, and a further 6 (8.75 [IQR]) days in a lower intensity of care. The total time spent on wards was significantly different between open and EVAR for those entering level 3 care (p<.001) and level 2 care (p=.002). Two cases of open repair and one case of EVAR had to be re-escalated from level 2 to level 3 care.
Blood transfusion
Open repair required a significantly higher number of units of RBCs, FFP, platelets and cryoprecipitate, as shown in Figure S6 (see Appendix online at www.jvsgbi.com) (p<.001).
Discussion
These data describe the outcome of all ruptured abdominal aortic aneurysms in a large vascular unit serving a sizeable population.
Mortality
Mortality rates for ruptured abdominal aortic aneurysms (rAAAs) highlight the first 30 days post-surgery as critical, with open repair showing a 30-day mortality of 34%, rising to 37% after 90 days. EVAR outcomes are better, with a 30-day mortality of 12%, increasing slightly to 15%. Survivors of open repair past 30 days have a good chance of reaching one year. Compared to the IMPROVE study’s 90-day mortality rates of 35.1% for EVAR and 38.3% for open surgery,4 this study aligns with open surgery rates but shows a significantly lower mortality for EVAR, by 20.1%. The Cambridge Vascular Unit’s EVAR-first policy, influenced by IMPROVE and similar studies, means patients with suitable anatomy for EVAR, who generally have better survival outcomes,5-7 are preferentially selected, leaving more challenging cases for open surgery. In effect, the patients undergoing EVAR tend to be a self-selecting group due to their haemodynamic stability.
Palliation rates can affect perceived mortality rates, but this study found 20% of patients were palliated from the entire cohort. When only analysing the patients that presented originally to Addenbrooke’s, the palliation rate was 34.3%, lower than the national average of 39.3%,8 indicating a successful intervention strategy at the Cambridge Vascular Unit.
Demographics
The average age of individuals receiving palliative care was notably higher than those undergoing surgery, which aligns with expectations since older people often have more co-morbidities and less physiological reserve. Abdominal aortic aneurysms (AAAs) occur predominantly in men, yet a higher percentage of palliated individuals were women. These women tend to present with AAAs later, with less favourable anatomy and a greater risk of rupture.9
Temporal trends
The overall caseload is decreasing, a trend matched by overall AAA repair rates, likely due to fewer smokers, better medical therapy and increased screening and non-screening pick-up rates. In 2014, 18.1% of UK adults smoked; by 2021 this dropped to 13.3%.10 Interestingly caseload dropped noticeably in 2022. By November 2022, 14 cases were recorded, lower than the previous average of 25. Further evaluation cycles are needed to confirm this trend.
Ruptured AAAs present with varying stabilities so the reported mortality rate may simply show natural variation. Cambridge Vascular Unit operated on an average 26 cases of rAAAs per year, a large number compared to the average UK vascular unit (1,458 rAAA repairs were reported from 2020-2022 – an average of 8 per centre per year).11 Given the relatively low frequency of these complex surgeries, other centres may need to look towards novel methods to keep skill sets current.12,13
Despite COVID-19, there was not an increased tendency to palliate patients. However, mortality rates did see a drop during the pandemic. More patients may have deteriorated at home, reducing diagnoses. However, the pandemic’s impacts may have been more nuanced and over-arching effects have since reduced the rupture rate, though future research is needed to confirm this.14,15
Pre-operative imaging
POCUS can be done at the bedside to help confirm a rAAA diagnosis, though it is unsuitable in determining whether anatomy is EVAR-suitable, which requires CT. The two most common reasons for EVAR unsuitability were being too unstable and having inappropriate and complex anatomy. These patients are already more likely to have worse outcomes from their pre-morbid state, perhaps explaining why the short-term outcomes for open repair are worse than EVAR.
Return to theatre
Open repair had a much higher early return to theatre than EVAR (p=.012). Patients often required multiple returns to theatre due to complications in open repair, while no patients returned more than once to theatre after EVAR. Laparotomy was the most common reason for returning to theatre in open surgeries. Open surgery was associated with more complex procedures during return to theatre, including amputations and bowel ischaemia operations, likely due to greater patient instability.
Long-term re-intervention rates were significantly higher for EVAR compared to open repair. No midline hernia repairs were recorded following open repair, possibly because these cases occurred in the patient’s local hospital. This is consistent with the literature, that those with EVAR are more likely to require reintervention in the long term.16 While EVAR requires further re-intervention in the long term, open surgeries require more in-hospital re-interventions.
Care requirements
Open-repair patients consistently spend significantly more time on level 3 and level 2 wards compared to EVAR patients. Similarly, open-repair patients used significantly more blood cells and products.
Limitations
This paper reports the palliation rate for a large tertiary hospital, something not often reported in the literature. Still, there are some important limitations which would have affected the calculated palliation rate, particularly regarding the number of palliated patients recorded. Cases may not be logged on the system when patients die at home, before they contact the hospital or in the ambulance. Even for patients that may die from a rAAA, it may be that the cause of death is not recorded, especially if they are frail. Secondly, cases are referred to the Vascular Hub from external hospitals. Some cases which are deemed unsuitable for transfer due to inoperability may not reach the arterial centre, therefore reducing the relative palliation rate, which is not captured by this dataset. In the spoke hospitals, there are consultants in satellite areas who document cases which should capture most decisions. Therefore, due to centralisation, such palliation without review is rare in modern clinical practice and so it would be rare for cases from spoke hospitals to not be included in this report.
While these limitations have been presented, this estimated palliation rate is the best that can be done currently with the resources given. The number operated on is relatively certain from the EPIC hyperspace system. However, the limitations given will likely mean that some palliated patients were missed. This would mean that the calculated palliation rate is probably an underestimation of the true value. Even acknowledging these limitations, the palliation rate is still 35.1% for just the Cambridge population, below the national average. For improvement, death certificates of the entire population would need to be analysed to find some of the missed cases which have been highlighted, though this would require many more resources.
Conclusion
This study reports on outcomes for patients with ruptured abdominal aortic aneurysms at a tertiary vascular centre, importantly including the denominator – the number of palliated patients. Though acknowledging the limitations of the study, this estimate is the best estimate with the data available. Our mortality rates are below those generally reported in the literature.2 Adopting an EVAR-first approach results in favourable mortality rates and short-term outcomes, including shorter hospital stays and reduced post-operative complications. Even so, open repair also shows promising results for patients with complex anatomies not suitable for EVAR. Future research on ruptured AAAs should aim to include palliation rates to enhance understanding of surgical success. This study highlights the need for paired reporting of surgeries and palliation rates to put success rates into perspective. A unit’s palliation rate does not necessarily need to change practice, but can theoretically confound outcome reporting if not reported, and could therefore contribute to setting an intervention target.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;4(2):74-80
Publication date:
February 28, 2025
Author Affiliations:
1. University of Cambridge, School of Clinical Medicine, UK
2. Cambridge University Hospitals, Cambridge, UK
Corresponding author:
Arjun Sharma
Gonville and Caius College,
University of Cambridge,
Trinity St, Cambridge,
CB2 1TA, UK
Email: [email protected]











