Systematic review
Changes in functional health status following open abdominal aortic aneurysm repair and the role of exercise-based rehabilitation: a systematic review
Ravindhran B,1 Lathan R,1 Staniland T,2 Carradice D,1 Chetter I,1 Smith G,1 Saxton J,3 Pymer S1
Plain English Summary
Why we undertook this work: An abdominal aortic aneurysm (AAA) is a balloon-like swelling of the aorta, which has a higher chance of rupturing if it grows beyond 5.5 cm. Surgery within 8 weeks is therefore recommended for all suitable patients with aneurysms greater than 5.5 cm. Delayed recovery and complications are common following open AAA repair. Complications include temporary or long-term damage to the lungs, kidneys and/or bowel. Also, reductions in functional ability are likely due to the required bed rest and the demands of surgery. At present we do not know how much functional ability reduces after AAA repair. Additionally, exercise-based therapy following AAA repair could reverse these reductions in functional ability, although we do not know if there is enough evidence to support this suggestion.
What we did: We systematically reviewed the current evidence to improve our understanding of the reduction in functional ability following AAA repair (component 1). We did the same to increase our understanding about whether exercise can improve functional ability (component 2) following AAA repair. Databases were searched to identify trials that have explored the changes in functional ability and the effect of exercise following AAA surgery.
What we found: We found no published evidence or ongoing studies to improve our understanding of the reduction in functional ability following AAA repair (component 1). One study met the criteria for component 2. This trial compared the impact of a forward or backward walking-based physiotherapy programme with standard physiotherapy following surgery. Patients who underwent walking-based physiotherapy could walk for a longer distance during the 6-minute walk test and also had better energy reserves than patients who underwent standard physiotherapy.
What this means: No evidence is available to help us understand the changes in functional ability following AAA repair. There is limited evidence available to help us understand the impact of exercise-based rehabilitation. Therefore, future research is urgently needed to explore these areas.
Abstract
Background: Physical domains of quality of life measures are negatively impacted following abdominal aortic aneurysm (AAA) repair. This is likely to reflect a reduction in objective measures of functional status, although this is yet to be established. These reductions can be targeted via exercise-based rehabilitation. This review aims to systematically evaluate the current evidence quantifying changes in functional status following open AAA repair and to consider the role of exercise-based rehabilitation for these patients.
Methods: The Medline, EMBASE and Cochrane CENTRAL databases were searched using two distinct search strategies. We included all prospective randomised and non-randomised trials that considered the impact of open AAA repair on functional status and/or the effect of exercise-based rehabilitation following open AAA repair. The primary outcomes were changes in objective measures of functional status following AAA repair and changes in these measures following exercise-based rehabilitation. Risk of bias was independently assessed by two review authors using the criteria outlined in the revised Cochrane tool (ROB 2.0) or the risk of bias in non-randomised studies of interventions (ROBINS-I) tool.
Results: No studies were identified that quantified changes in functional status following open AAA repair. One study considered exercise-based rehabilitation. This three-arm randomised trial compared two walking-based exercise programmes with routine care physiotherapy. Patients who underwent backward walking-based rehabilitation had a significantly lesser decline in functional status than the other groups, based on the 6-minute walk test and standard metabolic equivalents. There were no significant differences in length of stay or pulmonary function.
Discussion: This is the first systematic review to explore the objective decline in functional status and the role of exercise-based rehabilitation following open AAA repair. There is no evidence to quantify functional decline following AAA repair and limited low quality evidence to support exercise-based rehabilitation. The ideal next step for future research would be a feasibility or observational before-and-after cohort study using direct measures of physical function such as the short physical performance battery or the 6-minute walk test.
Introduction
Patients with abdominal aortic aneurysms (AAA) are usually older adults with widespread atherosclerosis and considerable cardiovascular risk factors.1–3 As a result, open surgical repair is associated with significant perioperative morbidity which may require a prolonged inpatient or intensive care stay.4,5 The associated metabolic and cardiopulmonary challenges may have substantial resultant consequences on functional status and quality of life (QoL).6,7 The current evidence suggests that there are initial declines in both mental and physical domains of QoL following AAA repair, with the mental domains recovering to preoperative levels by 4–6 weeks post-surgery. The physical domains, however, may take more than a year to recover.8,9 This suggests that there are likely to be quantitative changes in functional status following AAA repair that are reflected in these reductions in physical QoL domains.
However, no systematic review evidence has considered these quantitative changes.
Exercise-based rehabilitation has the potential to ameliorate some of these reductions in functional status and QoL following open AAA repair. However, the evidence to support this has also not been synthesised. This is despite evidence to suggest that exercise programmes performed preoperatively improve functional capacity and postoperative outcomes,10,11 as well as the recommendations to enrol patients in exercise-based cardiovascular rehabilitation following major cardiac surgery.12
Therefore, the aims of this study are to (1) review the evidence considering quantitative changes in functional status following AAA repair, and (2) review the evidence for postoperative exercise-based rehabilitation following AAA repair.
Methods
This review was split into two components to specifically address each of the aims above. Aims 1 and 2 will be referred to as components 1 and 2, respectively. The full study protocol has been published previously, and outlines the search strategy, inclusion criteria, data management selection and collection process, outcome measures, risk of bias and quality of evidence rating and planned data analysis.13
Briefly, searches were performed on the MEDLINE, EMBASE and Cochrane CENTRAL databases from inception to 23 June 2022. For component 1, search terms included “Aortic Aneurysm” [AND] “Functional Capacity” [OR] “Functional decline” [OR] “Functional capacity” [OR] “Aerobic endurance” [OR] “Functional Fitness” and for component two, terms included “Aortic Aneurysm” [AND] “Exercise therapy” [OR] “Physical Therapy” [OR] “rehabilitation”. All randomised and non-randomised trials were eligible for inclusion. For component 1, trials that considered the impact of AAA surgery on quantitative measures of functional capacity and physical function were eligible whilst, for component 2, trials that considered the effect of exercise-based rehabilitation following AAA repair were eligible. Study screening, data extraction and risk of bias and quality assessment was performed by two independent reviewers, with a third reviewer consulted to resolve conflicts.
The primary outcome was changes in objective measures of functional status either after AAA repair (component 1) or after exercise-based rehabilitation (component 2), including but not limited to metabolic equivalent of task (MET), cardiopulmonary exercise test parameters such as maximum oxygen consumption (VO2 max), ventilatory efficiency (VE/VCO2 slope), anaerobic threshold (AT), or objective measures of physical function such as the six-minute walk test (6MWT), short physical performance battery (SPPB) or timed up and go (TUG). For component 2, secondary outcomes included all-cause mortality, cardiovascular mortality, event-free survival, rate of rehospitalisation, changes in QoL and adverse events related to the intervention.
For each component we intended to produce a narrative synthesis with a summary of findings table. Meta-analysis was planned, but this was precluded by a lack of available data.
Results
Component 1
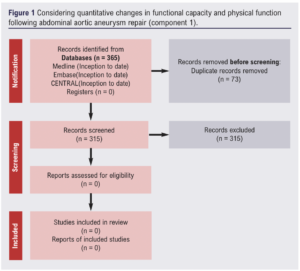
Out of 365 potential studies screened, none met the inclusion criteria (Figure 1). There was therefore no available evidence to evaluate the changes in objective measures of functional status following AAA repair.
Component 2
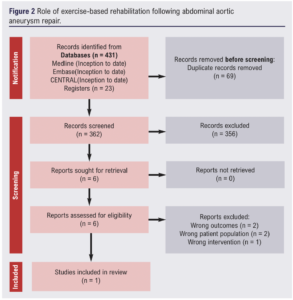
Out of 431 potential studies screened, one met the inclusion criteria (Figure 2). The included study was a three-arm randomised trial that compared two walking-based exercise programmes with routine care physiotherapy in a cohort of 65 patients (Table 1).14 The risk of bias summary for this trial is shown in Figure 3.
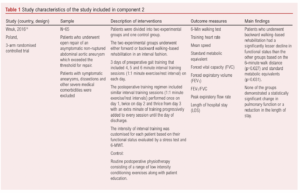
Routine postoperative physiotherapy consisted of a range of low intensity conditioning exercises along with patient education to improve awareness about postoperative rehabilitation. The walking-based interventions included forward or backward walking performed in an interval fashion. The training intensity was customised for each patient based on their baseline functional status. The frequency of training started at once per day, increasing to three times per day, whilst exercise duration was also gradually increased. Exercise was performed from the first day post-surgery to the day of discharge. The results of this study demonstrated that patients who underwent backward walking-based rehabilitation had a lesser decline in functional status, which was statistically significant. These findings were based on changes in the six-minute walk distance and METs, calculated as: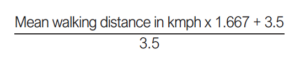
None of the three groups had a significant improvement in pulmonary function nor a significant reduction in length of stay. There were also no differences between these groups for these outcomes.
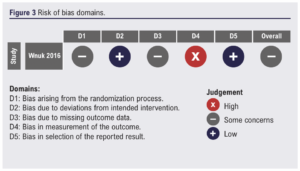
A risk of bias assessment of this study revealed some concerns for bias, with the overall predicted direction favouring the experimental group. This rating was mainly because study participants were recruited from a larger purposefully selected cohort and there was a lack of blinding (Figure 3). We were unable to assess the certainty of evidence with just one study eligible for the review.
We identified no completed or ongoing studies that quantitatively assessed the decline in functional status following open AAA repair. We searched for studies irrespective of publication year, publication type and publication status. We also searched relevant clinical trial registries to identify ongoing trials or any that had not yet been published. This makes it likely that this finding is a true reflection of the current evidence base.
We identified one completed randomised clinical trial that evaluated the effects of exercise-based rehabilitation following open AAA repair, which showed promising results.15 However, there were some concerns of bias because of purposeful patient sampling and the single blind nature of the study. Moreover, the authors also acknowledge that the study was underpowered.
We identified another study considering the feasibility of a home-based exercise programme following major surgery, including open AAA repair. However, the results are not available so this study cannot yet contribute to the evidence base.15 Clearly, the evidence base considering the impact of AAA repair on functional status and the role of exercise-based rehabilitation is almost non-existent.
Functional outcomes after major vascular surgery have become an increasingly important area of interest in recent years, especially with the limited amount of published data.16 Significant declines in subjective physical health composite scores have been demonstrated after both open and endovascular repair, with open repair being associated with a statistically significant decline in three out of four physical health domains.17 Other attempts have been made to assess the general wellbeing in patients after AAA repair, but these have been limited in scope and have not contained specific end points.18,19 As such, there is a paucity of data quantifying whether there is an objective decline in functional status following AAA repair. It would, however, be reasonable to expect a decline in functional status, given the possible complications and associated perioperative metabolic and cardiopulmonary challenges. Indeed, this has been demonstrated in patients undergoing coronary artery bypass grafting,20 but is yet to be evaluated in those undergoing AAA repair. Exercise-based rehabilitation has the potential to ameliorate some of the reductions in functional status and QoL following AAA repair. However, we have also demonstrated a paucity of data to support this notion.
Therefore, as anticipated in the protocol for this review, we have demonstrated that there is little or limited evidence exploring these current areas of interest. Despite the recommendation that all patients undergo cardiovascular rehabilitation following major cardiac surgery,21-24 which is supported by strong evidence,25 the evidence for such interventions following AAA repair is limited to just one study. This is also surprising considering that preoperative exercise programmes improve fitness and reduce complications in patients undergoing AAA repair,11 and such gains are likely to be furthered via the use of postoperative exercise programmes.
Given that there is limited evidence to support the efficacy of exercise-based rehabilitation in those undergoing AAA repair, known barriers such as a lack of funding, expertise and patient motivation will be all the more pertinent.26
Based on the limited evidence identified by this review, important evidence gaps remain. First, the extent to which functional status is impacted by open AAA repair needs to be established. Second, the effect of exercise-based rehabilitation on functional status and QoL also needs to be established.
This review is not without limitations. The clear lack of evidence precludes our ability to make any conclusions or recommendations, other than those for future research. However, we followed the guidance of the Cochrane handbook and performed a comprehensive literature search across several databases that span both published and unpublished sources. We therefore believe that this review highlights a true lack of evidence, rather than evidence that has been missed due to poor methodology.
Overall, this review has identified that there is no evidence quantitatively objectifying the impact of open AAA repair on functional status. It has also identified that there is extremely limited evidence to support exercise-based rehabilitation following AAA repair. Future research is urgently needed to establish this evidence base. Identifying any objective decline in physical function is imperative to ascertain the need for targeted postoperative rehabilitation, especially in a cohort likely to derive significant benefit from exercise-based rehabilitation. The ideal next step for future research would be a feasibility or observational before-and-after cohort study using direct measures of physical function such as the SPPB and 6MWT to track the objective decline in physical function over time following AAA repair.

Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022; 3(1): 46-51
Publication date:
November 20, 2023
Author Affiliations:
1. Academic Vascular Surgical Unit, Hull York Medical School, Hull, UK
2. Hull University Teaching Hospitals NHS Trust, Hull, UK
3. Department of Sport, Health and Exercise Science, University of Hull, Hull, UK
Corresponding author:
Bharadhwaj Ravindhran
Academic Vascular Surgical Unit, 2nd Floor, Allam Diabetes Centre, Hull University Teaching Hospitals NHS Trust, Hull HU3 2JZ, UK
Email: [email protected]











