REVIEW
Carotid webs: a review of diagnosis and management strategies in current literature
Ahmad M,1,2 Tan M,1,2 Abuarqoub M,3 Patel K1, Siracusa F,4 Shalhoub J,1,2 Davies AH1,2
Plain English Summary
Why we undertook the work: Carotid webs are small protrusions on the inside of blood vessels in the neck where clots can form and lead to a stroke. They are a rare cause for strokes in young people and can be difficult to diagnose. We undertook this review to look at the current research on how this is being treated globally.
What we did: We evaluated existing evidence in the literature on the diagnosis, management and outcome of carotid webs.
What we found: We found a mix of low- and medium-quality evidence, which suggests there is no clear guideline on the best way to manage carotid webs at present. Options include treating with medication which thins the blood, keyhole surgery to put stents in the blood vessel or open surgery.
What this means: There is no clear evidence about which option is better and when this should be done, and further studies are needed. It would be useful to establish a worldwide registry so that data can be standardised and evidence improved.
Abstract
Introduction: Carotid webs (CaW) are non-atherosclerotic fibrous bands which present as shelf-like linear intraluminal filling defects at the carotid bulb or internal carotid artery. They are a known cause of cryptogenic strokes. Current management includes medical, interventional (stenting) and surgical approaches.
Aims: The aim of this review was to systematically evaluate the existing evidence in the literature on the diagnosis, management and outcomes of carotid webs. Methods: This review was performed in accordance with the Preferred Reporting for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A combination of the medical subject headings (MeSH) terms “carotid web”, “carotid shelf”, “CaW”, “web vessels”, “Intraluminal web” and “cryptogenic stroke”, “ischaemic stroke”, “embolic stroke of undetermined source” was utilised in the primary search. Basic descriptive statistical analysis was completed using IBM’s Statistical Package for the Social Sciences (SPSS) statistics software, version 29.
Results: 123 articles met the criteria and underwent data extraction. This included two registry reviews, 13 cohort studies, 20 case series and 73 case reports. The articles spanned from 1967 to 2024. A pooled total of 771 patients were included (registry and cohort studies n=559; case series/case reports n=212). A higher prevalence of CaW is reported in young female patients and in patients of Afro-Caribbean origin. Symptom recurrence is reduced following intervention in the form of stenting or open surgery in a subset of patients. There is little evidence on the management of asymptomatic CaW.
Conclusions: Current literature on CaW lacks homogeneity and is mostly anecdotal in nature. Previous studies have focused on diagnosis, with emerging cohort studies in the last decade evaluating management options. Further large-scale studies are needed. Establishing a worldwide registry will allow standardisation of the data collected and evaluated. Improving the quality of evidence available will help to guide management.
Introduction
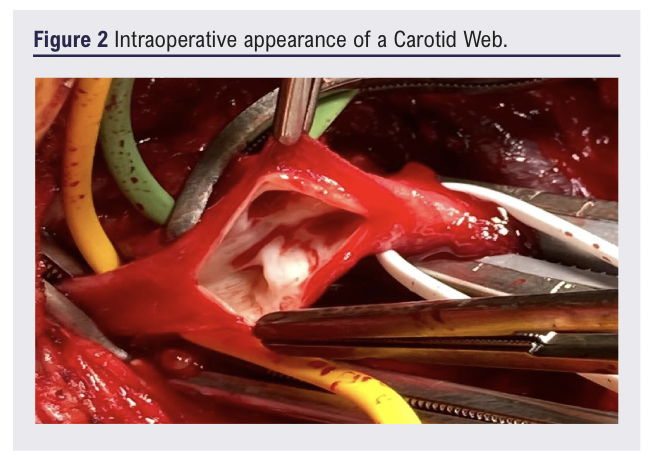
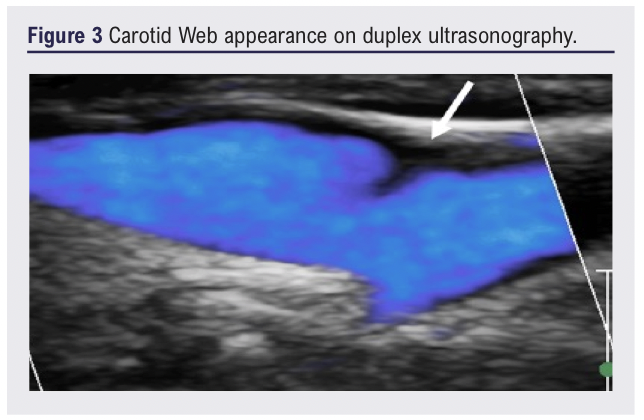
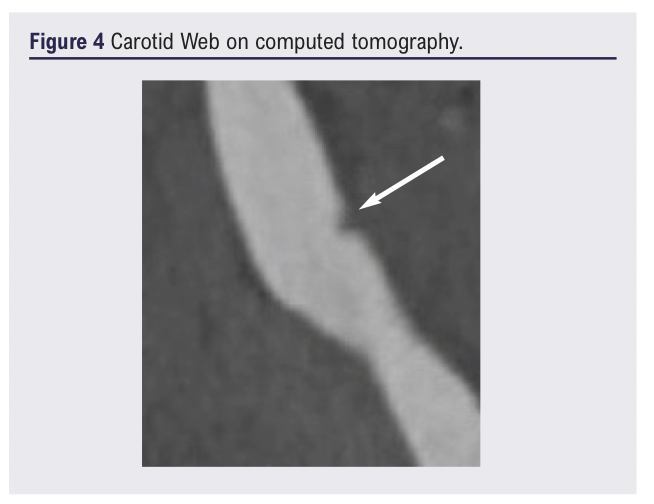
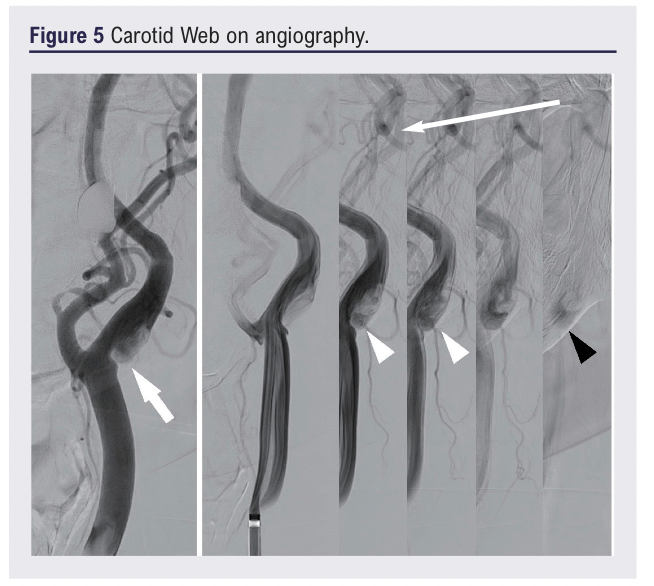
Carotid Webs (CaW) are non-atherosclerotic fibrous bands which present as shelf-like linear intraluminal filling defects, often on the posterior wall of the carotid bulb or the proximal internal carotid artery, causing turbulent flow (Figures 1-5).1-4
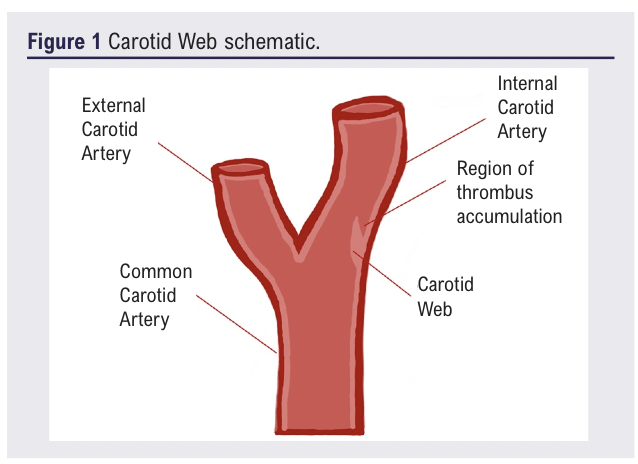
The condition was first described by Ehrenfeld in 1967 and is often referred to as atypical fibromuscular dysplasia due to the fibrosis and hyperplastic changes seen in the intimal layer on histology.3,5,6 CaW are difficult to diagnose on imaging and are increasingly being recognised as a source of cryptogenic stroke. The CaW shelf serves as an area for accumulation of thrombus with a risk of subsequent embolisation, resulting in large vessel occlusion and subsequent ischaemic strokes.7-9 A high index of suspicion should be considered in cases where no other source for the transient ischaemic attack (TIA) or stroke has been identified. CaW are still underdiagnosed due to the imaging challenges and a general lack of awareness of this pathology. Current literature suggests that CaW have a higher prevalence in young individuals (age <60 years), female patients and individuals of African descent.1,10-15 Current management options may include conservative medical management, carotid artery stenting (CAS) or surgical intervention in the form of carotid endarterectomy (CEA) and web resection with or without patchplasty or segmental resection.8
Aim
The aim of this review was to evaluate existing evidence in the literature on the diagnosis, management and outcomes of carotid webs.
Methods
This review was performed in accordance with the Preferred Reporting for Systematic Reviews and Meta-Analyses (PRISMA) statement.16 The literature was searched using Embase and Medline (via Ovid interface), Web of Science, Scopus and CINAHL databases. A combination of the medical subject headings (MeSH) terms “carotid web”, “carotid shelf”, “CaW”, “web vessels”, “Intraluminal web” and “cryptogenic stroke”, “ischaemic stroke”, “embolic stroke of undetermined source” and “stroke” was utilised in the primary search strategy.
Randomised controlled trials, cohort studies, cross-sectional studies, observational studies, case series and case reports on the subject of CaW were included. Studies were limited to those written in the English language. No time limit was placed for the search and articles up to 2024 were included. The exclusion criteria consisted of studies where only the prevalence or incidence was reported, abstracts, letters and conference papers. The abstract and title screening and full text review was completed using the Covidence software by two reviewers (MAh, KP, MT).
Data extraction was completed by four reviewers (MAh, MT, MAb, FS). The extracted information included the author, year of publication, type of study, number of patients, age, gender, ethnicity, presenting complaint, co-morbidities, initial investigations, investigation findings, territory of stroke/TIA, National Institute of Health Stroke Scale (NIHSS) score, ipsilateral/contralateral disease, acute management, long-term management, histology and outcome. Basic descriptive statistical analysis was completed using IBM’s Statistical Package for the Social Sciences (SPSS) statistics software, version 29.
Results
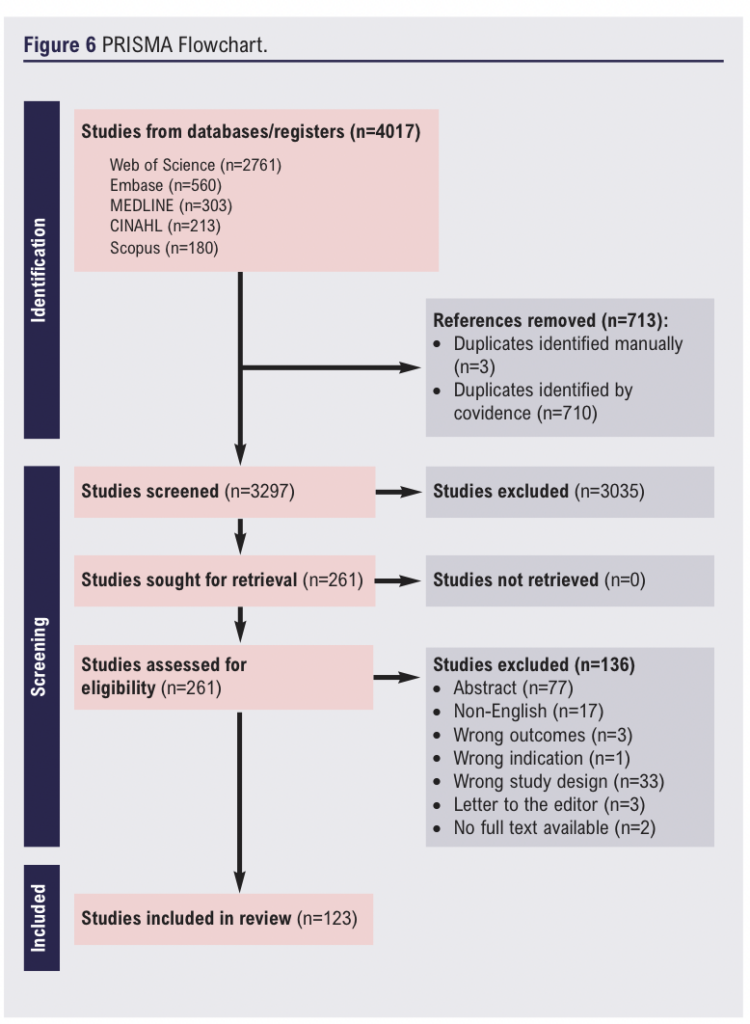
Some 4,017 articles were initially identified and they are summarised in Figure 6. After de-duplication, 3,297 articles underwent title and abstract screening and of these 3,035 were excluded. 261 articles were assessed for eligibility. 123 articles met the criteria and underwent data extraction. They included two registry reviews, 13 cohort studies, 20 case series and 73 case reports. The articles spanned the period from 1967 to 2024.
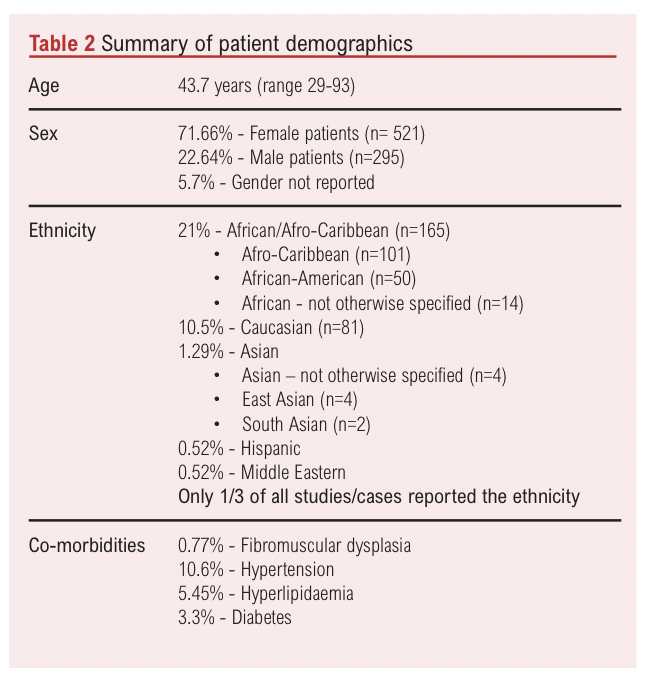
A pooled total of 771 patients were included (registry and cohort studies n=559; case series/case reports n=212).3,6,17-105 The findings are summarised in Tables 1-4. Further details of each case series and case report are available to view in Appendix 1 (online at www.jvsgbi.com). There was a higher prevalence of CaW reported in female patients (n=521) compared to male patients (n=295). Forty-four case reports did not describe the gender. The mean age of presentation was 43.7 years (range 29-93 years) across the case series and reports. The mean age range across the pooled registry/cohort studies was between 44-59 years. Fifty-five patients had concurrent bilateral carotid webs.3,25,38, 42,47,49,67,106-109 Only a third of the articles reported the ethnicity. A higher prevalence was reported in individuals of African descent, who represented 21% of the patient cohort (Afro-Caribbean n=101, African-American n=50, African n=14), followed by 10.5% of Caucasians (n=81). Other reported ethnicities included Asian (1.29%), Middle Eastern (0.52%) and Hispanic (0.52%). Where reported, almost 9% of the 212 patients (n=19) from the case series/case reports had a series of recurring symptoms at the time of presentation and diagnosis, although the time frame for these was not clear. All other reported cases were emergent or semi-emergent cases presenting with symptoms in the preceding hours or days. From the symptomatic case reports, 79% presented with TIA and 58.9% had stroke symptoms. There were 20% which did not specify the presentation or had atypical symptoms. The NIHSS score at presentation was provided in 54 case reports. The mean score was 7.7 at presentation (range 0-25). Six patients had a known pre-existing diagnosis of fibromuscular dysplasia.2,17,18,22,26,47,53,110 The most commonly co-morbidities, where reported, were hypertension in 10.6% of the cohort, followed by hyperlipidaemia in 5.45% and diabetes in 3.3%.
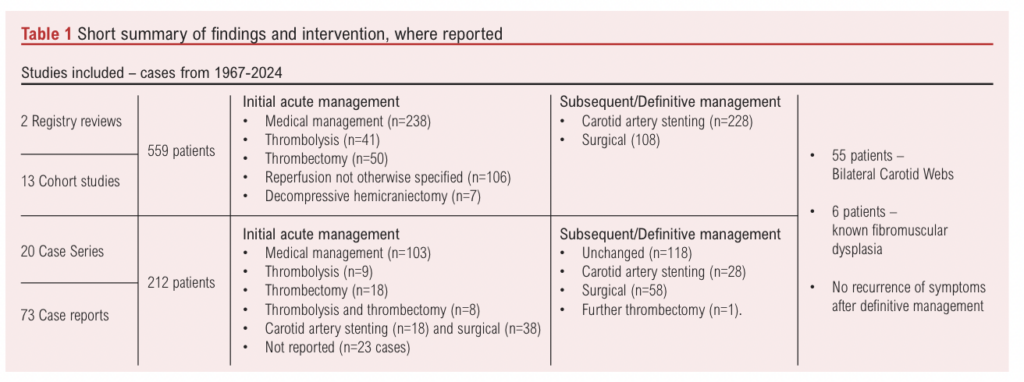
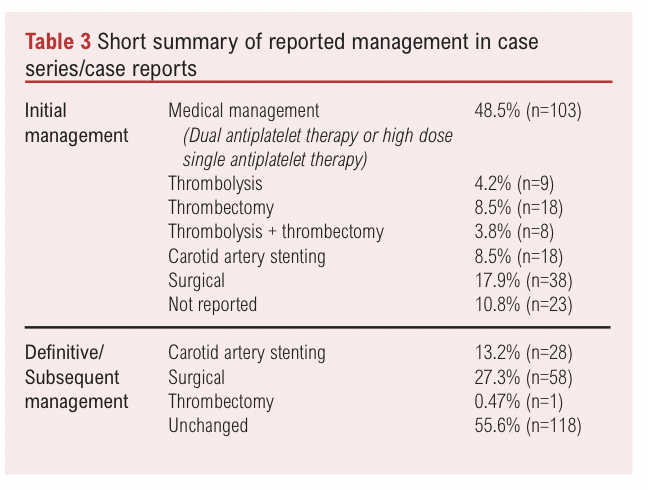
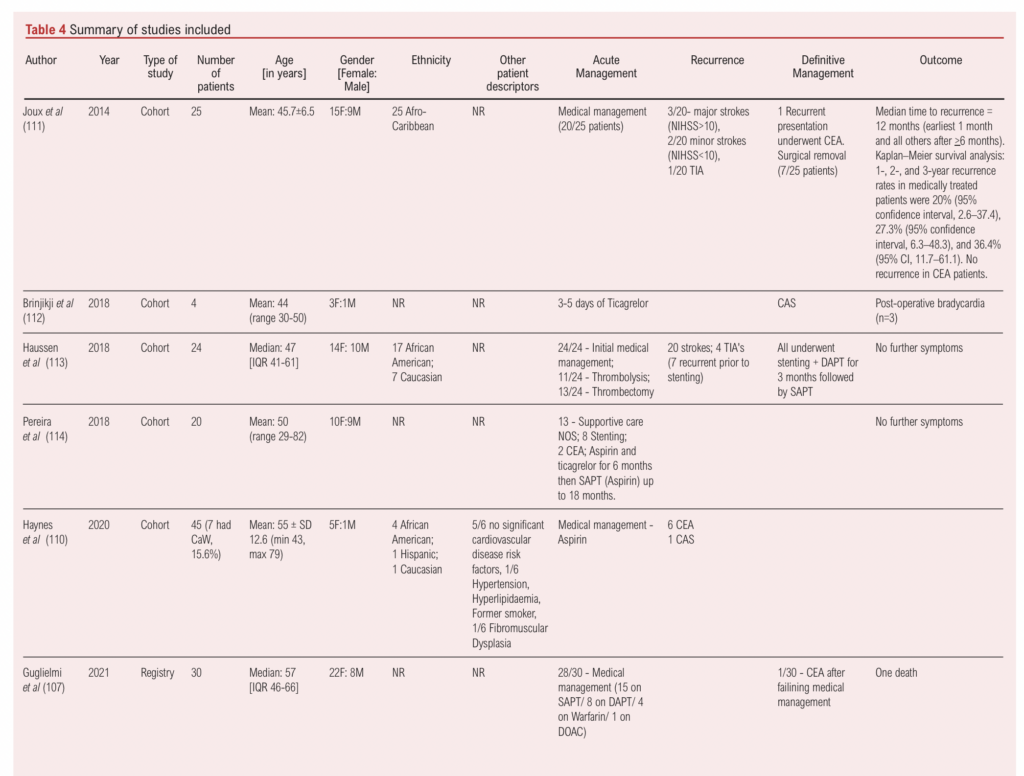
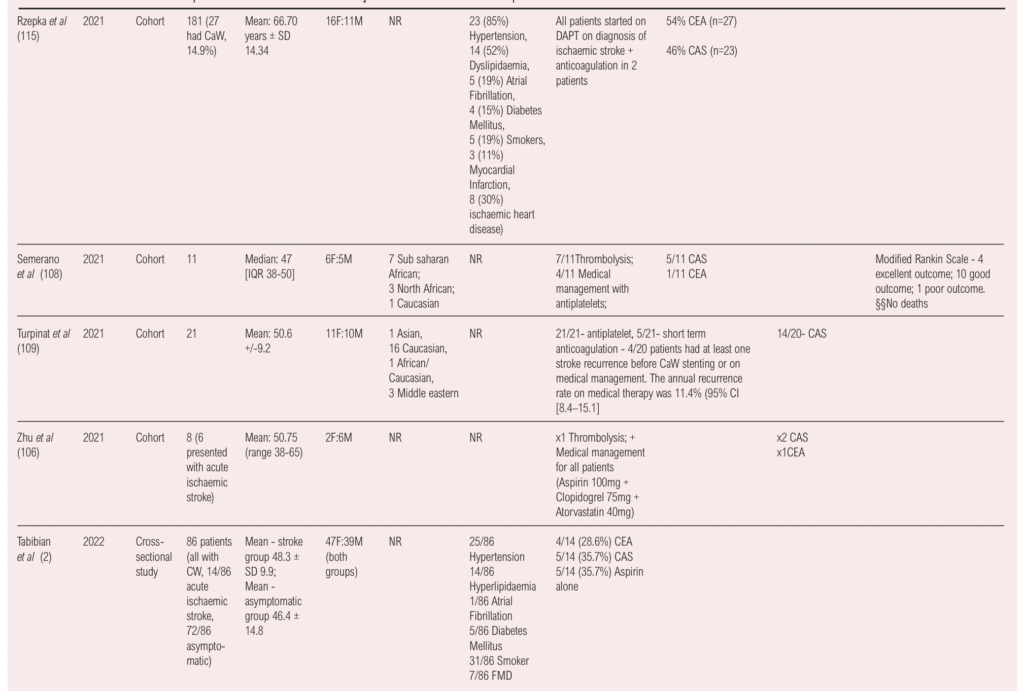
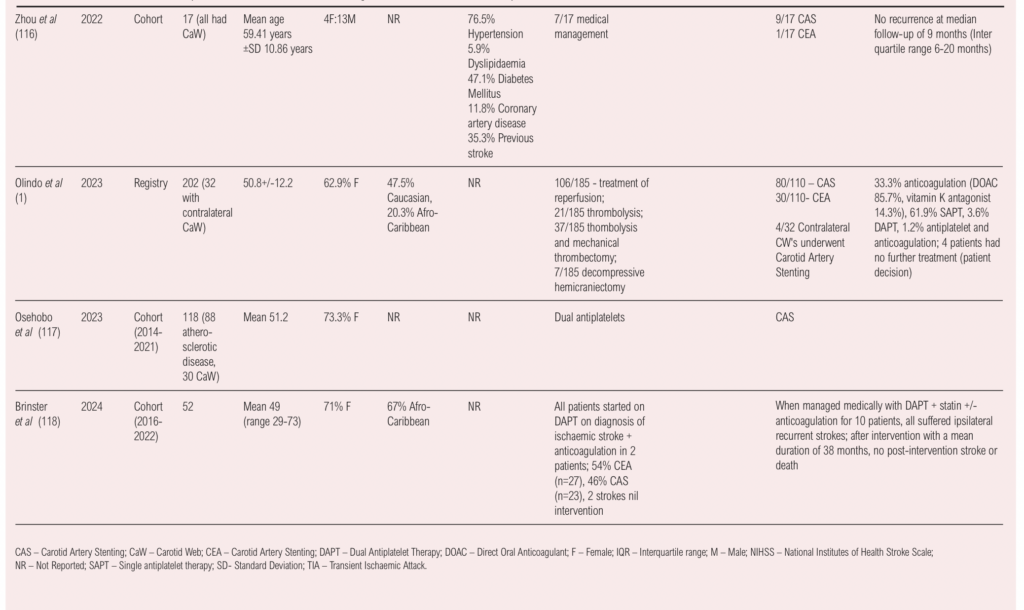
All studies and case reports initially managed CaW with medical management or thrombolysis/thrombectomy.2,106-119 However, further intervention with either stenting or surgery was required in a subset which comprised almost half the patient group who had symptom recurrence or as a means to definitive management of the CW.2,106,108,109,111,112,115,116,119 Of the 212 cases reported, the initial acute management included medical management with dual antiplatelet therapy or a high-dose single antiplatelet agent in 48.5% of the reported cases (n=103). 4.2% underwent thrombolysis (n=9), 8.5% underwent thrombectomy (n=18), 3.8% had thrombolysis and thrombectomy (n=8), 8.5% had carotid artery stenting (n=18) and 17.9% had surgical intervention (n=38). Initial management was not reported in 23 of the 212 cases. Subsequent, definitive management remained unchanged in more than 55.6% of the patients. However, further interval intervention included carotid artery stenting 13.2% (n=28), surgical 27.3% (n=58) and further thrombectomy 0.47% (n=1). None of the patients reported further symptoms following further definitive management.
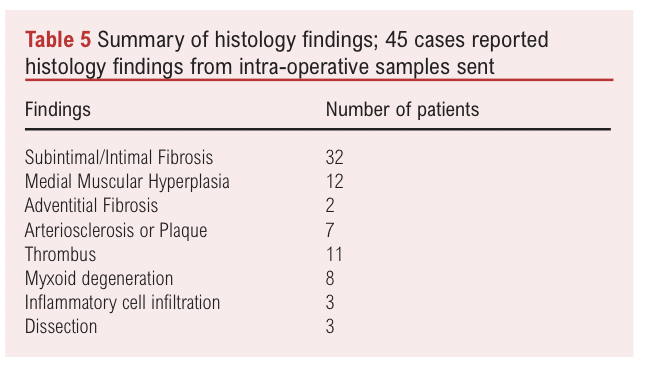
Forty-five cases reported the intra-operative histology from the tissue samples sent. These are summarised in Table 5. Common findings included subintimal/intimal fibrosis (n=32) and medial muscular hyperplasia (n=12) and to a lesser degree, adventitial fibrosis (n=2). Associated thrombus was reported in 11 cases and arterioscleosis or plaques were mentioned in seven cases. Other histological findings included myxoid degeneration (n=8), inflammatory cell infiltration (n=3) and dissection (n=3). Myxoid degeneration results in the accumulation of mucin in tendons, ligaments and fibrocartilage and its presence in CaW warrants further research to gain an understanding of the underlying pathology of CaW formation.
A single peri-partum case with bilateral CaW was also reported in a 39-year-old female with a history of ocular symptoms five years prior to presenting with left arm weakness. This was managed successfully with dual antiplatelet therapy, switched to low molecular weight heparin in the late third trimester and six weeks following delivery.67 Further statistical analysis was not possible owing to missing data as well as the overall heterogeneity of the data available.
Discussion
CaW are increasingly being recognised as a source of stroke for which no other causes may be identified leading to large vessel occlusion, particularly in younger patients.42,119 Current imaging modalities include duplex ultrasonography, computed tomography angiography and high-resolution magnetic resonance angiography: however, CaW can be difficult to detect.103,106,116 Barriers to diagnosis include lack of awareness and diagnosis with respect to imaging interpretation. Lesion identification can take up to four and a half months after initial stroke symptoms in as many as a quarter of patients.1 CT angiography appears to be the most commonly used imaging modality in diagnosing and reporting CaW.1,106,107 Duplex ultrasonography can be helpful as it provides information on the morphology of the CaW and can highlight haemodynamic changes, especially thrombus formation, but requires experience and expertise.106 The literature comprises predominantly case reports and case series, with cohort and cross-sectional studies emerging in the last decade.
The true prevalence of CaW remains unknown. Registries such as MR CLEAN in the Netherlands and the CAROWEB in France have helped to shed light on this.1,15 The CAROWEB registry, comprised of 224 cases, found that CaW were not identified at the time of mechanical thrombectomy in 30 out of the 85 patients.1 The MR CLEAN registry found a 2.5% prevalence of CaW on the symptomatic side and a 0.5% prevalence on the asymptomatic side in a cohort of 443 cases.107 Similar to findings from the pooled evidence in this review, CaW were identified primarily on CTA in female patients in a younger age group. In our pooled cohort of cases series/case reports, symptoms recurred in just under half of all patients, requiring further definitive treatment. The MR CLEAN registry reported a recurrence rate of about 17% over a two-year period. The overall true recurrence rate is therefore not entirely clear. The results from these registries have helped to shape the current iteration of the European Society of Vascular Surgeons current guideline on CaW. The overall underdiagnosis of CaW is a possible factor in the recurrence of symptoms which would otherwise not yield any underlying causes for symptoms during initial investigations.
Current management options available include antithrombotic and antiplatelet medication, including aspirin, clopidogrel or a combination of both, and statin use. Immediate management in acute cases where there is evidence of large vessel occlusion with focal neurological changes includes thrombolysis and/or thrombectomy followed by either medical management or intervention. Carotid artery stenting is a minimally invasive option in patients who may otherwise be high risk or who opt for this option. Dual layer stents show positive results without significant complications.103 Open surgical intervention can include endarterectomy and patchplasty, or web excision and anastomosis, as described in some reports.
In general, there appears to be a higher rate of symptom recurrence in patients managed medically.11,31,109,111,118,120 The overall time to symptom recurrence varies between 1-97 months, with another study citing a median 12 months to symptom recurrence.31,111 An annual symptom recurrence rate of up to 11.4% has been reported in patients on medical therapy alone.109,111 Other studies reported that their cohort of patients with CaW presenting with transient ischaemic attacks progressed to cerebral infarction within three months of medical management in almost two-thirds of the cases.121
No further symptoms were reported after definitive intervention in the form of carotid artery stenting or carotid endarterectomy.106,111-113,115,116,117,120 The risks and side effects associated with intervention also need to be considered and balanced with the frequency of symptom recurrence and future risk of symptom recurrence and risk of stroke. This also needs to be balanced with potential advances in endovascular methodology. The timing of definitive intervention also varies vastly and seems to be dependent on a number of factors, including symptom recurrence and surgeon preferences.
There seems to be a general lack of consensus in managing concurrent contralateral CaW without symptoms. The CAROWEB registry reported invasive intervention (primarily carotid stenting) in four of the 32 patients with contralateral CaW, which appears to show a slightly higher intervention rate for contralateral CaW in the US.4,120 Consideration must also be given to the management of asymptomatic carotid webs which may be detected incidentally. Little is known as to when CaW may occur, whether there is an embryological component and why symptoms present in young patients before the age of 60 but not earlier if CaW have been present for a long period. This also prompts the question as to whether these should be expectantly managed medically and whether early intervention could offset any potential risk of stroke in future. The optimal timing of any definitive intervention in asymptomatic patients also warrants further exploration.
The European Society of Vascular Surgeons current guideline on CaW recommends that for “symptomatic patients with a carotid web in whom no other cause for stroke can be identified after detailed neurovascular work up, carotid endarterectomy or carotid artery stenting may be considered to prevent recurrent stroke”.8 This is based on Level C evidence, given the lack of consistent and sufficient data, and has been highlighted as an area warranting further research.8,122 At present, these patients are managed on a case by case basis, with involvement of relevant specialities including radiologists, stroke physicians and vascular surgeons. There are also differing opinions on whether these cases should be managed with stenting or surgery as definitive management.
The current UK National Vascular Registry (NVR) reports data on patients undergoing carotid stenting and carotid endarterectomy and/or patchplasty. However, it does not report data on CaW and this in part may be due to the underdiagnosis or overall prevalence. Perhaps establishing a worldwide registry would allow uniformity in global reporting and help to establish the true incidence as well as allowing follow-up of the management and outcomes in these cases?
Conclusion
Current literature on CaW lacks homogeneity and is mostly anecdotal in nature. Previous studies have focused on diagnosis, with emerging cohort studies in the last decade evaluating management options. Symptom recurrence is reduced following intervention in a subset of patients. However, the literature on the management of asymptomatic CaW is very limited.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;4(2):99-110
Publication date:
February 28, 2025
Author Affiliations:
1. Section of Vascular Surgery, Department of Surgery and Cancer, Imperial College London, London, UK
2. Imperial Vascular Unit, Imperial College Healthcare NHS Trust, London, UK
3. Imperial School of Medicine, Imperial College London, London, UK
4. London Northwest University Healthcare NHS Trust, London, UK
Corresponding author:
Manal Ahmad
Specialty Registrar and Clinical Research Fellow, Section of Vascular Surgery, Department of Surgery and Cancer, Imperial College London, 4th Floor, North Wing, Charing Cross Hospital, Fulham Palace Road, London W6 8RF, UK
Email: [email protected]











