ABSTRACTS
Top 4 Trainee Competition Abstracts from VASGBI ASM, Belfast
FIRST PRIZE
Emergency management of post-carotid endarterectomy neck haematoma: a teaching and simulation training package
R Little, E Spodniewska, G Hughes, M Safar, T Irving
Liverpool University Hospitals Foundation Trust (Royal Liverpool Hospital)
Background
Post-operative neck haematoma is a clinical emergency that can rapidly progress to airway obstruction and cardiorespiratory arrest if not recognised and managed in a timely manner. In response to a number of high profile cases, joint national guidelines have recently been produced by the Difficult Airway Society, the British Association of Endocrine and Thyroid Surgeons, and the British Association of Otorhinolaryngology, Head and Neck Surgery.1
Although these focus primarily on the management of neck haematoma post-thyroid surgery; the principles can be applied to other forms of neck surgery, including patients who have undergone carotid endarterectomy.1
Aim/Method
Based on the recommendations set out in these guidelines, ‘neck haematoma boxes’ were introduced to our department to facilitate the rapid emergency decompression of a neck haematoma using the SCOOP (Skin exposure, Cut sutures, Open skin, Open Muscles, Pack wound) approach.1 The contents were rationalised and standardised following discussion with our surgical colleagues to include laminated guidelines, scissors/scalpel, sterile gloves, and gauze.
Alongside the introduction of the boxes, a training package was created to develop the knowledge and skills of the non-surgical members of the perioperative team, with the aim of improving their competence and confidence in the early recognition and management of post-operative neck haematoma. This consisted of a short presentation, followed by familiarisation with the new boxes, and finally the opportunity to decompress a mannikin’s ‘neck haematoma’ in a low-fidelity simulation. In the initial pilot phase, the training package was delivered to a range of members of the multidisciplinary perioperative team (n=65); including recovery nurses, operating department practitioners (ODPs), and anaesthetists. Pre- and post-knowledge questionnaires (with a maximum score of 23) and confidence surveys (with a ranking of 1-10) were performed to gain objective and subjective feedback respectively.
Results
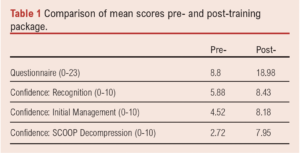
The mean questionnaire score pre-training was 8.8 (SD 3.48) compared to a mean of 18.98 (SD 2.33) post-teaching (see Table 1). When comparing pre- versus post-training surveys, similar improvements were seen in candidates’ confidence for the recognition (mean 5.88 vs 8.43), initial management (mean 4.52 vs 8.18), and performance of SCOOP decompression (mean 2.72 vs 7.95) of a post-operative neck haematoma. Analysis using paired t-test demonstrated statistically significant improvement in each of these score measures (p<0.0001).
Conclusion
In conclusion, as a result of the introduction of this training package, our staff have both improved knowledge and confidence in the management of this life-threatening emergency.
Reference
1. Iliff, H.A., El-Boghdadly, K., Ahmad, I., et al. Management of haematoma after thyroid surgery: systematic review and multidisciplinary consensus guidelines from the Difficult Airway Society, the British Association of Endocrine and Thyroid Surgeons and the British Association of Otorhinolaryngology, Head and Neck Surgery. Anaesthesia 2021;77:82-95.
SECOND PRIZE
Hospital stress factors affects peri-operative care for non-elective lower limb revascularization
K Kohler, DJ Stubbs
University of Cambridge
Background
Patients requiring re-vascularisation for ischaemic lower limbs present a challenge to the peri-operative service as they require urgent intervention, often have complex medical needs and present outside of the elective pathways. The current capacity challenges in the NHS have resulted in a stressed peri-operative care system that faces significant challenges to provide efficient and expedient care. Hospital stress has been shown to result in worse patient outcomes.1
Post-operative care can be characterized by both the time to discharge and the complications a patient encounters. The severity of encountered complications can be summarized in a EPOMS score.2
Aims
The aim of this study was to investigate whether routinely collected hospital stress measures such as bed state and emergency department waiting times are related to a reduced level of care for these high acuity patients.
Methods
We used OPCS codes to select electronic health records from of patients who received non-elective lower limb revascularization at our tertiary care hospital between January 1st 2015 and August 1st 2021. We aggregated parameters such as basic demographics, length of stay, post-operative complication score and added routinely collected hospital stress parameters to build a model relating the outcomes of post-operative complications and length of stay to hospital stress.
Results
Our cohort contained 1072 unique patient encounters with sufficient data completeness in their electronic record. Within this patient cohort, the average length of stay was 6.25 days, 136 had an ICU stay and 29 patients died in hospital. The ASA distribution was: ASA 1 2%, ASA 2 24%, ASA 3 65% and ASA 4 7.2% and the median maximal EPOMS score was 2 (interquartile range 1- 3).
We built a cox-model for the length of stay analysis (censored for patients who died in hospital or were discharged back to their home hospital), which showed that when we considered patient factors alone – age, sex, ASA and complexity of the surgery we found the concordance to be only 0.5, but when we added in the hospital stress measures (hospital occupancy, ICU occupancy, number of theatre sessions cancelled, number of discharges, number of ED breaches and the hospital-wide acuity of inpatients represented by aggregate average NEWS2 score) we found the concordance improved to 0.6.
We also investigated whether we could model patients waiting time for their operation, in particular longer wait than the recommended 5 days, and found that the model again improved significantly with the inclusion of hospital stress measures compared to patient factors alone.
We then built a linear regression relating patient and hospital factors to post operative morbidity (EPOMS) and based solely on patient factors we had a R2 = 0.05 and a p-value of 0.03. When adding daily averaged stress measures we improved the model performance to R2 0.22 with a p-value<0.0001 and so found that including stress parameters we can explain 22% of the observed variation in post-operative morbidity.
Conclusions
Our study was able to quantify that patients admitted for lower limb revascularization had a longer length of stay if the hospital was more busy, which could potentially create further backlog and impact on the ability to perform elective surgery. Additionally, in a busy hospital patients waited longer for surgery and their post-op care needs were higher. While we did not yet investigate where the higher EPOMS score originated and which specific factors contributed most the results will warrant further investigation.
References
1. Eriksson CO, Stoner RC, Eden KB, Newgard CD, Guise JM. The Association Between Hospital Capacity Strain and Inpatient Outcomes in Highly Developed Countries: A Systematic Review. J Gen Intern Med 2017 Jun; 32(6):686-696.
2. Stubbs DJ, Bowen JL, Furness RC, Gilder FJ, Romero-Ortuno R, Biram R, Menon DK, Ercole A. Development and Validation of an Electronic Postoperative Morbidity Score. Anesth Analg 2019 Oct;129(4):935-942.
Blood transfusion & lower limb amputations – A role for cell salvage
A Dodd, S Lillywhite, O Richards, G Ambler, E Cairns, K Zander
Southmead Hospital, North Bristol NHS Trust
Background
North Bristol Trust is the major arterial centre for Bristol and the surrounding regions and carries out 50-100 lower limb amputations per year. Local audit from 2019 identified a high requirement for allogeneic blood transfusions in this patient group (33% transfused; mean of 3.6 units per patient over days 0-7 post-operatively).
Aim
To reduce the requirement for allogeneic blood transfusion through the routine use of cell salvage and or tourniquet application during lower limb amputations.
Method
A process of continuous iterative quality improvement was employed. Baseline data was collected retrospectively on all lower limb amputations carried out in the Trust in 2020 and between January and April 2022. Electronic notes were examined to collect data on the type of amputation, indication for surgery, surgeon grade, cell salvage use (not used vs collection only vs processing and return) and tourniquet use. Haematology and transfusion records were interrogated to determine pre and postoperative haemoglobin levels and the number of blood products transfused to each patient, days 0-7 post-operatively. Following analysis of this data, a multi-disciplinary education programme was initiated to embed the default use of cell salvage for lower limb amputations, with a focus on the use of swab wash. The education programme utilised posters, oral presentations to surgical and anaesthetic multi-disciplinary teams and regular email correspondence to all theatre staff. Practice was re-audited between May and August 2022.
Results
Pre-operative mean haemoglobin levels were 114g/L (range 71-169g/L, 2020), 110g/L (range 79-137g/L, January-April 2022) and 114g/L (range 72-189g/L, May-August 2022). Post-operative mean haemoglobin levels were 95g/L (range 62-152g/L, 2020), 93g/L (74-112g/L, January-April 2022) and 96g/L (range 72-119g/L, May-August 2022).
Prior to the education programme, less than 5% of patients had cell salvage set up for collection and processing (collection only: 4% in 2020 and 4.5% in 2022; processing: 0% in 2020 and 4.5% in 2022) and 25% (2020) and 18% (2022) of patients had a tourniquet applied intra-operatively. Post the education programme, 74% of patients had cell salvage set up with 4% receiving processed cell salvage blood and 52% had a tourniquet applied intra-operatively.
Prior to the education programme, the percentage of patients receiving a blood transfusion was 22% (2020) and 36% (2022) with a mean of 1.6 units (2020) and 1.3 units (2022) transfused per patient episode. Post the education programme, 35% of patients received an allogeneic blood transfusion with a mean of 1.3 units administered.
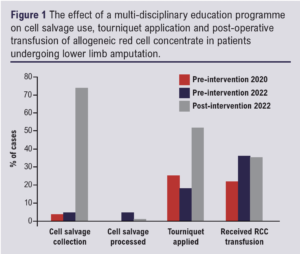
Discussion
Following the introduction of a multi-disciplinary education programme the use of cell salvage for collection of swab wash and tourniquet application during lower limb amputation surgery increased, however the administration of allogeneic blood transfusion in the post-operative period remains unchanged. This may reflect the lack of processing of cell salvage blood and the pre-operative anaemic state of this group of patients. Further education is now being delivered to encourage the processing and return of cell salvaged blood. Routine pre-operative assessment of ferritin levels and intravenous iron infusion is also being considered.
A novel e-learning course on the peri-operative care of the vascular patient
S Samad, P Rudra, C Christou, R Haddon, S Goon, L Grimes, C Sharpe, R Burnstein
Lister Hospital, Bedford Hospital, Cambridge University Hospital, Norfolk and Norwich Hospital. Health Education East of England Blended Learning Team.
Background
The Covid-19 pandemic has had a devastating impact worldwide with the number of lives the virus has affected. Whilst on a much smaller scale, its impact resulted in a loss of training opportunities for doctors. However, the pandemic and the requirements for social distancing has resulted in a rapid adoption and explosion of online distance learning and blended learning platforms.1 Within anaesthetic training in the England, we identified that whilst there was some learning content online, there was a distinct lack of an organised e-learning course to educate anaesthetist on providing peri-operative care for the vascular patient.
Aims
We sought to create a comprehensive accredited course that would enable an anaesthetist to learn the key elements of vascular anaesthesia via an interactive e-learning platform.
Methods
We utilised the 5 step ADDIE model (Analyse, Design, Development, Implementation and Evaluation) as the template to guide our course design.2 We ensured institutional alignment by mapping the learning objective of the course to those currently set by the Royal College of Anaesthetist curriculum. Our target audience were anaesthetist preparing to sit their final fellowship examinations and trainees who were learning vascular anaesthesia as part of their training. The course was designed to rely on an adult learning theory model and we ensured that the design of the course would appeal to all learner types such as visual, auditory and kinaesthetic learners. To ensure high quality content, specialist vascular anaesthetist from the East of England deanery were recruited to write and create the content for the course. Once the content had been created by the specialist, we then refashioned the information to make it more interactive and segmented the content into smaller sections to reduce learner cognitive load. We then created the course using the Rise Articulate platform.
Results
Once the course was completed on the platform. The complete course was sent back to the original content creators for review. Once the initial corrections and adjustment were made, we then sent the course to a small pilot group of trainee anaesthetist for review from a learner perspective and edited the course accordingly based on initial feedback. Finally, to ensure high level accreditation and validation, the course was reviewed and edited by the Vascular Society of Great Britain and Ireland and will also be reviewed by the e-learning for healthcare team at the Royal College of Anaesthetist prior to being made available on their e-learning for healthcare platform.
Conclusion
Distant learning and blended learning is becoming ever present in education and with the increasing recognition of the importance of a stable work life balance, it is critical that doctors are able to learn and educate themselves independently at a time that suits their learning needs.3 We believe that we have created a highly interactive and comprehensive vascular e-learning course with high quality content that will not only engage the learner but provide them with essential knowledge that they can then apply to their daily clinical practice.
References
1. Marinoni G, Land H van’t. The Impact of COVID-19 on Global Higher Education. Int High Educ [Internet]. 2020 Apr 30;0(102 SE-Articles). Available from: https://ejournals.bc.edu/index.php/ihe/article/view/14593.
2. Huynh R. The Role of E-Learning in Medical Education. Acad Med [Internet]. 2017 Apr;92(4):430. Available from: http://journals.lww.com/00001888-201704000-00013.
3. Khalil MK, Elkhider IA. Applying learning theories and instructional design models for effective instruction. Adv Physiol Educ [Internet]. 2016 Jun;40(2): 147–56. Available from: https://www.physiology.org/doi/10.1152/advan.00138.2015
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;2(1):57-60
Publication date:
November 22, 2022











