ORIGINAL RESEARCH
A case study project to explore physiotherapists’ experiences of using removable rigid dressings with patients post transtibial amputation in the UK
Gillow F1, Reed D1,2
Plain English Summary
Why we undertook the work: A transtibial amputation involves removal of a leg between the knee and ankle joint. Guidelines advise that after amputation a removable solid or semi-solid shell that extends to at least the knee is placed around the wound while healing takes place; this is called a removable rigid dressing. At present removable rigid dressings are not widely used in the UK and little is known about the experiences of using them. This study was therefore designed to look at the experiences of physiotherapists who have used removable rigid dressings.
What we did: We interviewed physiotherapists who had experience of using removable rigid dressings with patients as part of their rehabilitation. Ten physiotherapists who worked in acute hospitals and rehabilitation centres within the UK were included. Data from the interviews were analysed by looking for codes and then themes. Trustworthiness of the study was increased as researchers worked as a team to analyse the data and participants were then asked to check that the results reflected their views.
What we found: We found three themes from the interviews: (1) application of removable rigid dressings; (2) removable rigid dressing design; and (3) education and training related to use of removable rigid dressings and the advantages and disadvantages that can occur with these.
What this means: To make sure removable rigid dressings are used in the most effective way, the design and education and training provided needs to be thought about to achieve as many of the possible positive effects while reducing any potential negative effects. More research is required to work out the best design for removable rigid dressings and what education and training is needed.
Abstract
Introduction: Removable rigid dressings (RRDs) provide a solid or semi-solid shell around the residual limb post transtibial amputation. Clinical guidelines advocate the use of RRDs; however, in practice they are not widely used and little is known about the experiences of using them. This study explored the experiences of physiotherapists who have used RRDs with patients post transtibial amputation.
Methods: Qualitative research methods involving a constructivist epistemological approach with inductive reasoning and a case-study methodology were employed. Semi-structured interviews were completed with 10 physiotherapists from acute hospitals and rehabilitation centres within the UK. Thematic analysis was verified through respondent validation and researcher corroboration.
Results: The three themes identified were (1) application of RRDs; (2) RRD design; and (3) education and training related to the use of RRDs, and the associated advantages and disadvantages concerning these.
Conclusions: To ensure RRDs are used as part of patient rehabilitation most effectively, the design and education and training provided needs to be considered to achieve as many of the possible positive effects whilst minimising potential negative effects. Further research is needed on the design of RRDs and the education and training required.
Introduction
Traditionally, post transtibial amputation (TTA) a soft dressing consisting of elasticated bandage and padding would be applied in theatre and kept on for up to five days. In 1969, Berlemont et al challenged the use of soft dressings with a rigid plaster replacement.1 Soft dressings have since been associated with pressure sores and persistent oedema.2 However, lack of access to inspect wounds with a rigid plaster dressing resulted in fears of wound breakdown.3
In response to the desire to regularly inspect the residual limb, Wu et al designed a removable rigid dressing (RRD) made from plaster cast and socks.4 It was noted that RRDs provided progressive compression of the residuum, contributing to a reduction in average healing time from 109.5 days in the control group to 46.2 days in the study group.4 Reduction in healing time is of particular importance for TTAs, as prosthetic rehabilitation becomes more expensive and less successful the longer it is delayed postoperatively.2 Since this early work, RRDs have evolved to either be ‘off-the-shelf’ vacuum-formed dressings or custom made from casting materials. All provide a solid or semi-solid shell around the residuum and are removable for wound inspection, exercises and hygiene. RRDs can finish above or below the patella depending on the type used and clinical reasoning.
Clinical guidelines worldwide recommend RRDs post TTA to manage oedema, promote healing, protect the residuum and reduce incidence of fixed flexion deformities at the knee.5-7 However, it is acknowledged within the clinical guidelines that limitations of the current literature include small sample sizes with poorly defined outcome measures.5-7 Adherence to the guidelines is poor, with 72.27% of physiotherapists surveyed in the UK not using RRDs post TTA, although the survey return rate was not published raising questions regarding non-response bias.8
The literature investigating RRD effectiveness is inconsistent. Deutsch et al found no significant difference (p=0.61) in length of stay with an average 15.5 days spent in hospital post amputation when using an RRD and 17.4 days in the control group.9 However, Taylor et al reported a significant (p=0.001) reduction in acute inpatient length of stay from an average of 15.9 days to 8.7 days with the use of an RRD.10
A narrative review by Reichmann et al concluded that RRDs should be the first treatment choice post TTA to optimise outcomes with regard to reduction in injury post fall, knee flexion contractures, oedema, healing time, time to prosthetic fitting and pain.11 Although the narrative review involved a comprehensive literature search and appraisal process, as expected with a narrative review rather than a systematic review, it was a literature summary with no control of bias.11
Meta-analyses have been used to compare soft dressings to RRDs with results dependent on the criteria for the included literature. In 2019 Kwah et al focused on randomised controlled trials or quasi-randomised controlled trials, concluding that the benefits and harms of RRDs were still unknown due to very low-certainty evidence.12 More recently in 2023, Koonalinthip et al added in non-randomised studies to their meta-analysis and concluded that RRDs are significantly favourable to soft dressings when examining time to wound healing and prosthetic fitting, stump volume, postoperative pain and incidence of revision or joint contracture. However, Koonalinthip et al acknowledge that caution is needed in interpreting their results due to a high risk of bias within the studies included.13
In summary, due to lack of clarity in the literature for the multidisciplinary team and patients to make a fully informed decision on dressing type, more information is needed on the experiences of using RRDs. This study aimed to explore the experiences of physiotherapists who have used or are using RRDs with patients post TTA.
Methods
This study has been reported adhering to the Consolidated Criteria for Reporting Qualitative Research (COREQ).14
The study sought to explore and understand experiences by adopting qualitative research methods. More specifically, the philosophical underpinning involved a relativist ontological stance whereby it was accepted that multiple realities were created by participants’ subjective understandings.15 A constructivist epistemological approach was used to accept that reality is socially constructed.16 The relativist ontological stance and constructivist epistemological approach involved the use of inductive reasoning, allowing the researcher to create theory by understanding patterns.15 Case study methodology with semi-structured interviews was chosen to reflect the philosophical underpinning and to generate rich exploratory data with new thinking and ideas.17 A case study is usually considered a retrospective investigation into an event that has occurred and, in this project, the event was the use of RRDs on patients.18
Agreement was granted by the British Association of Chartered Physiotherapists in limb Absence Rehabilitation (BACPAR) Executive Committee to advertise the study to their members. BACPAR membership was chosen as it provides a UK network for physiotherapists specialising in limb absence rehabilitation. Given that 72.27% of physiotherapists working in amputee rehabilitation report not using RRDs in practice, it was expected that there would be few potential participants from which to recruit.8 A purposeful approach, whereby participants were selected for convenience with additional snowballing was therefore used to maximise participants.19 Participants were screened for suitability using the following inclusion criteria:
• Physiotherapist registered with the Health and Care Professions Council
• Able to read, understand and speak fluent English
• Able to participate in a virtual interview
• Experience of using an RRD with patients in hospital post TTA within the past 5 years
• To not be receiving any financial incentives from or work for a company marketing RRDs
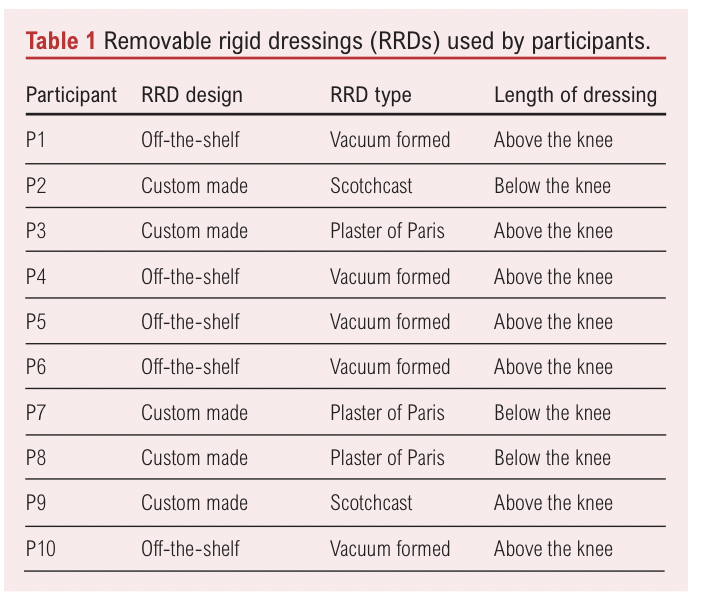
Ten volunteers met the inclusion criteria and took part in the study; five primarily had experience using custom made RRDs and the other five using ‘off-the-shelf’ RRDs, as shown in Table 1. Participants identified seven different acute or rehabilitation centres within the UK where they had mainly used RRDs. All participants who started went on to complete the study. Qualitative research is required by the COREQ checklist to consider data saturation, although the meaning of data saturation is poorly defined with variation in meaning.19,20 In this study saturation was considered to have been reached as data were only adding to a code rather than leading to the emergence of new codes.21
The lead researcher, who was a physiotherapist completing an MSc and who had recently undertaken qualitative research training as part of her studies, collected the data. The lead researcher was working in the field of amputee rehabilitation at the time of the research and knew two of the participants through her involvement with BACPAR. However, the lead researcher had no prior experience of RRD use. The insider status allowed the lead researcher to understand medical terminology used by participants and build a rapport without risk of her own experiences influencing discussions.
One 30 minute interview was conducted for each participant. All interviews were virtual using Webex in the lead researcher’s home or workplace and were captured using both audio and visual recording. Field notes were made as appropriate after each interview rather than during the interview to reduce distraction. The interview process and guide was piloted with one participant. No changes were required, therefore permission was gained from the participant to include their data in the study. Interviews were professionally transcribed and participants conducted respondent validation of the transcript; changes requested were made.
Ethics approval was granted by the University of Kent on the 21 August 2021. Participants were provided with a Participant Information Leaflet to ensure they were fully informed on their right to withdraw, confidentiality and anonymity. Participants signed a consent form before interviews commenced.
Data analysis
Thematic analysis was used to systematically create meaning from data, comprising four stages.21 Data analysis took place concurrently with data collection to allow for follow-up of emerging ideas, moving backwards and forwards between the stages.21
To enhance credibility, researcher corroboration was used as a form of inter-rater reliability throughout the coding, categorisation and theming. In addition, participants were given the opportunity to ‘member-check’ the final analysis and confirm that their contributions had not been misinterpreted or misrepresented.
Results
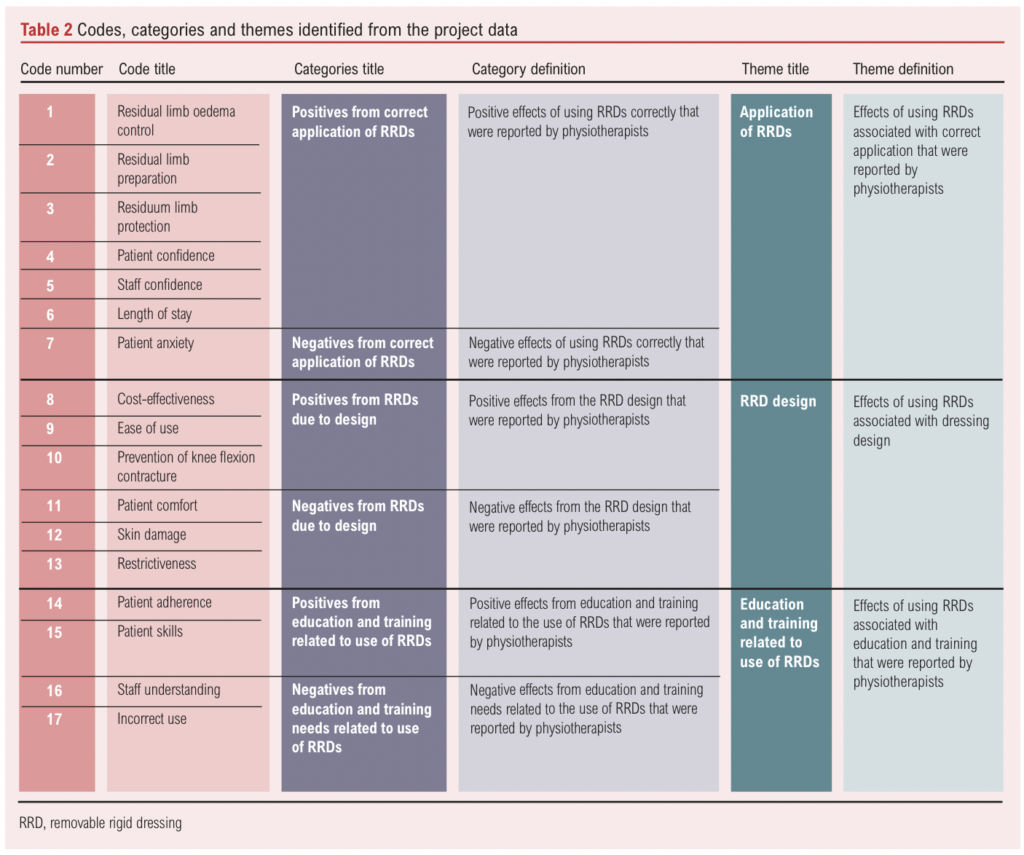
The codes, categories and themes identified from the data analysis are shown in Table 2. Coding produced 17 codes from the data and categorising led to six categories. Finally, theming resulted in three themes: (1) application of RRDs; (2) RRD design; and (3) education and training related to the use of RRDs.
Application of RRDs
Application of RRDs included the effects of using RRDs correctly that were reported by participants. Effects were mainly positive, with just one potential negative.
Participants discussed the importance of RRDs for residual limb protection and explained ‘protection’ was one of the main reasons for RRD use. The solid construction was noted to provide protection in the event of a fall or trauma that can occur during daily activities: “It’s [RRD] also an extra layer of protection when they’re in bed, so if they’re rolling around and accidently knock their leg … It’s an extra layer to, to help with that.” (P4) Participants also mentioned positive effects of RRDs on residual limb oedema, although effectiveness was affected by timing, with application in theatre giving favourable results. “It [RRD] does contain the swelling to a certain degree, although perhaps not as much as it would if put on in theatre.” (P3)
As well as oedema reduction, improvements in residual limb shape ready for prosthetics were reported. “I would say, probably the stumps are a bit better shaped and a bit less oedematous because of the use of RRDs.”(P1) RRDs were also described as helping to prepare for prosthetics by increasing tolerance to pressure: “[Positives of RRDs] Getting used to actually being enclosed in something for a significant part of the day. So that definitely will help patients when they’re actually getting used to the wearing tolerance of the socket.” (P8)
Patient confidence towards rehabilitation and activity were reported to improve with RRD use. It was not only patients who were noted to be more confident; staff confidence improved as well: “I think they [RRDs] give them [patients], more confidence and clinicians kind of peace of mind as well that they’ve done everything in their power to protect that vulnerable, healing leg.” (P7) Participants suggested length of stay was reduced due to improvement in patient confidence from RRD use. However, others acknowledged the impact of numerous factors upon length of stay: “Length of stay-wise, potentially there is [a benefit], because again we don’t have as many wound issues and the rehab’s being speeded up. But it’s hard to put length of stay down to just one thing, isn’t it?” (P2)
The only negative code within the theme was ‘patient anxiety’, which occurred due to being asked to use RRDs: “To put a great big dressing on gives, could give, if they’re healed and further down the line, it could give them a bit of a negative message about moving and fear.” (P7) Patient anxiety was also noted to occur when RRD use was discontinued, potentially reducing patient progress: “I’ve had a few patients who have got quite attached to having it, their leg covered and … yes, so they were kind of declining taking it [RRD] off and moving to the next steps.” (P5) It was debatable whether ‘patient anxiety’ would be better placed in the ‘Education and training related to the use of RRDs’ theme. However, despite appropriate education and training, patient anxiety related to RRD use could still be an issue.
RRD design
The theme included effects of using RRDs associated with design. Codes related to RRD design did not always have exclusively positive or negative effects.
Generally, participants viewed RRDs as simple to use for the multidisciplinary team and patients: “Patients can take it on and off really easily.” (P9) However, other participants reported requiring two staff members to reapply RRDs when the patient was less able to help or noticed that method of securing RRDs affected ease of application: “Sometimes patients find them difficult because the Velcro is sticky, so if that gets a bit crinkled, that can be a little bit tricky for them.” (P6)
The design of RRD and cost impacted participants’ perceptions of effectiveness. One participant felt RRDs were not cost-effective as they are single-patient use: “They are not cost-effective, perhaps, if you could clean them it would be better, it seems such a waste to put them in the bin if they have not stayed on long.” (P10). In contrast, others compared the cost of the RRDs to the potential cost of residual limb complications and concluded cost effectiveness: “I would say they probably are [cost effective]. I think the consequences of not using them are probably quite significant … prosthetically if someone has a fixed flexion contracture then that’s a nightmare to manage.” (P5)
Participants reported prevention of knee flexion contractures as a benefit of RRDs extending above the knee joint; for those that do not routinely go above the knee participants explained they could be extended when required: “Occasionally we can do them [RRDs] above the knee, if someone’s got fixed flexion, we almost like serial cast them into more extension.” (P2)
Skin damage was a major risk linked to RRD design. Participants reported patients could actively flex within some types of RRDs, resulting in patella pressure sores. Participants commonly talked about the potential for skin damage to the residual limb and noted it could occur on the remaining limb too: “The bulky corners could dig into the remaining limb, causing pressure problems and potential lesions.” (P10) Additionally, participants suggested some RRDs cause patient discomfort with heat and bulkiness whereas others were unaware of any problems with comfort. As well as causing discomfort, bulkiness was also described as restricting patients, making it harder to complete personal activities of daily living: “For personal care and toileting, it [RRD] gets in the way.” (P4)
Education and training related to the use of RRDs
The theme included the effects of using RRDs associated with education and training that were reported by participants. This considered education and training of staff within the multidisciplinary team and patients.
Through the use of RRDs, patients were noted to learn how to manage the number of socks to obtain a comfortable fit, a skill required when using a prosthesis: “I’d definitely say there have been some patients who have begun to understand sock management. Because actually they have had to add socks.” (P8) Patient education on benefits and reasons for use was noted to improve the likelihood of patients wearing RRDs: “Generally, people got into the habit of it [wearing RRDs] and if you explained … it’s to protect your wound so to get you … further along your rehab, then they were on board with it.” (P7)
As identified in RRD design, RRDs used incorrectly were reported to risk skin breakdown, RRD breakage or a loss of the potential benefits of RRDs: “Sometimes if the patella window’s not cut adequately then they can get pressure areas across the patella.” (P9)
Education and training were mentioned as areas where improvement was essential to prevent negative experiences, and development of competencies was suggested as a method of preventing incorrect use: “We probably need to roll out some more regular training and develop competencies for the ward staff. I think the whole being able to put it on correctly is the biggest element to it.” (P4)
Discussion
The discussion explores the relationship between the three themes derived from data analysis and the previous literature.
Application of RRDs
Preparation for prosthetics as a benefit from using RRDs was identified from the literature and the results of this study.11,13 A major component of preparation for prosthetics is residual limb oedema control. The use of RRDs for oedema control is widely publicised within professional guidelines and there was a risk that participants would cite guidelines rather than their own experiences.5-7 However, it was found that participants related to their own practice and questioned if greater benefits in oedema control could be seen with earlier application of RRDs.
The other component of preparation for prosthetics is residual limb preparation. Increased tolerance to residual limb pressure was described in this study and has been previously discussed by Hughes et al in their reflective account.22 In this study, limb shape was also suggested to be improved with RRD use. It was not explored in the literature reviewed and, since it is affected by surgical approach, technique and skin condition, it is difficult to assess objectively.
Another common theme in the literature was residual limb protection, with outcome measures focusing on damage sustained or need for revision surgery.11,13 In this study, protection from falls featured in the participants’ comments, but importance of protection was also noted for activities of daily living. Studies investigating protective effects of RRDs using complications or falls as outcome measures may miss recording the more subtle effects.
The combination of residual limb protection and increased confidence was speculated by participants to contribute to a reduction in length of stay. Logically, if residual limb complications are reduced through improved protection and both patients and staff are more confident to participate in rehabilitation, length of stay may decrease. Previous studies have demonstrated an inconsistent impact on length of stay with RRD use, and it has been suggested that length of stay may be approaching the minimum number of days as other factors such as adequate pain control or availability of a care package prevent further reductions.9,10
Patient anxiety was the only negative effect identified from correct application of RRDs. Anxiety occurred due to fear from the need for a large dressing and apprehension at the time of removal. This negative effect from covering the residual limb with a RRD had not been previously discussed in the literature reviewed and is an important consideration.
Design of RRDs
Some of the positive and negative effects identified in this study are specific to certain materials and designs of RRDs, and these effects are encompassed in this theme. However, it is beyond the scope of this study to compare effects of different RRD designs.
Prevention of knee flexion contracture was one of the most apparent ways in which design affected the outcomes from RRD use. RRDs extending above the patella were reported by participants and in the literature to be beneficial in helping prevent knee flexion contractures.11,13 With contractures affecting only 13% of transtibial amputees in hospital and small sample sizes in research, it has been difficult to demonstrate statistical significance.23 The benefits of RRDs going above the patella and potentially preventing knee flexion contractures require balancing against potential negatives. Participants reported some patients still flex their knee within the RRD, causing patella pressure damage. Others found that dressings above the patella had potential to cause skin damage to the remaining limb. Additionally, participants suggested other design factors played a part in skin problems, comfort and restrictiveness, with certain materials causing perspiration or bulkiness affecting clothing that could be worn.
The design of RRDs affected their ease of use for both patients and members of the multidisciplinary team. Generally, design made RRDs easy to use but there were elements of design that increased application difficulty. Going forward it would be useful to consider whether ease of use can be improved through design, education and training or potentially a combination of both.
The cost of providing RRDs was determined by design and some custom types required further RRDs to be manufactured when oedema reduced. Generally, participants reported RRDs to be cost-effective when considered against potential costs of complications, such as knee flexion contractures or trauma to the residuum. It has been claimed in the literature that RRDs are more costly than standard dressings, but this study highlighted that those costs need to be balanced against potential cost savings.12
Education and training related to the use of RRDs
Provision of education and training related to the use of RRDs was reported by participants to lead to positive effects if done well, or negative effects such as incorrect use of RRDs when education and training were not effective.
Positive effects included patient acquisition of skills that are important for use of prosthetics, such as sock management which may make it easier for patients to adapt to prosthetic use. It was also noted that provision of education and training to patients helped to encourage adherence, despite problems with discomfort and restrictiveness, as it created a greater understanding.
Negative effects related to education and training mainly revolved around staff understanding and incorrect use. Participants identified that greater benefits and fewer negatives could have been achieved from RRD use if the multidisciplinary team used them more effectively. The development of formal training and competencies for staff using RRDs, as suggested by participants, would be a useful consideration if not already in place. The role of education and training had not been explored in the literature reviewed, possibly because, when conducting research, the environment is often artificial without the impact of real-life factors within a healthcare environment such as high staff turnover, and education and training may therefore have not been an issue.
Methodological considerations
A case study methodology with virtual semi-structured interviews was used to answer the research question. Virtual interviews had the advantage of using the valuable visual cues and body language that traditional ‘gold standard’ face-to-face interviews offer.24 They also allowed access to participants from a much wider geographical area without travel costs or time constraints.25 Completing interviews virtually created technological challenges too. Participants experienced difficulties accessing the virtual meeting as many were not familiar with the platform used. The technological difficulties may have assisted in establishing rapport as the researcher and participant worked together to resolve problems.26 However, technological difficulties also caused delays to interview start times and stress to both participants and researcher. Despite the difficulties encountered with virtual interviews and the technology used, they were still found to be an effective method of data collection to answer the research question.
This project had the time and financial budget available to include more than 10 participants. However, the limiting factor was the number of people who volunteered to be interviewed. Given that 72.27% of physiotherapists surveyed in the UK were not using RRDs with patients, there was not a large pool from which to draw volunteers.8 Purposeful recruitment with additional snowballing led to some participants having their main experience of using RRDs at the same centre. The methodological underpinning of this study recognised that individual participants would have different subjective understandings regardless of the centre where experience took place and that participants may have prior experiences from previous education and practice that influence them. It could be argued that physiotherapists using RRDs are likely to have been proactive in establishing their use and be generally positive about the benefits. However, participants were included if they had experience of using RRDs within the last five years, so they were not necessarily still using them. It may be useful for future studies to examine continuation rates after RRD use has been introduced to a service and underpinning reasons.
This study could be expanded further by seeking the views of physiotherapists from other countries. The researchers also recognise that it would be useful for future work to explore experiences of patients and other members of the multidisciplinary team such as surgeons, occupational therapists, prosthetists and nurses to establish a wider viewpoint.
Conclusion
In the opinion of the participants, from correct application of RRDs five positive effects were identified: oedema control, preparation, protection, patient and staff confidence, and resultant potential for reduced length of stay. However, correct application of RRDs also brings potential for increased patient anxiety. The design of RRDs impacted experiences of physiotherapists. Generally, design was reported to make RRDs easy to use, useful for prevention of knee flexion contractures, and was considered cost-effective when compared with the potential complications of not using RRDs. However, design was also linked to potential skin problems, discomfort and restrictiveness. Further work is required to establish the optimal RRD design.
Education and training in relation to use of RRDs offers opportunity to teach patients skills ready for prosthetics and, when effective, was also noted to increase adherence to RRD use. However, ineffective education and training caused negative effects on staff understanding and application on patients. To improve within this area, participants suggested regular training and introduction of staff competencies.
This study identified a wide range of possible positive and negative effects within the themes generated. Choice of outcome measures and small sample sizes in previous research may have missed the more subtle but equally important effects from use of RRDs. This study may therefore guide outcome measures for future RRD research projects. Further research is required to expand this study, with inclusion of participants from a wider geographical area, involvement of other healthcare professions and patients, and investigation of the optimal design and education and training required for RRD use.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(4):218-225
Publication date:
August 16, 2024
Author Affiliations:
1. School of Health Sciences; Faculty of Education, Health and Human Sciences, University of Greenwich, Avery Hill Campus, Avery Hill Road, New Eltham, UK
2. Faculty of Life Science and Medicine, Centre for Education, Henrietta Raphael Building, King’s College London, UK
Corresponding author:
Fiona Gillow
School of Health Sciences, Faculty of Education, Health and Human Sciences, University of Greenwich, Avery Hill Campus, Avery Hill Road, New Eltham, London SE9 2UG, UK
Email: [email protected]











