ORIGINAL RESEARCH
Exploring the assessment, diagnosis and conservative management of patients with neurogenic thoracic outlet syndrome (NTOS): an online survey of UK medical and allied health professionals
O’Sullivan J,1 Miller C,1 Bateman M,2 Hill J3
Plain English Summary
Why we undertook the work: Neurogenic thoracic outlet syndrome (NTOS) is challenging to recognise and manage. While exercise and physiotherapy is widely recommended as the first-line treatment for NTOS, it is not clear what exercises should be performed, what the role of physiotherapy is, and which people will benefit from it. We therefore aimed to explore the experiences and opinions of UK therapy and medical professionals regarding their practices with people with NTOS.
What we did: An online survey was created and shared through email and social media and participants were encouraged to share with others who may be interested. The survey remained active for 4 weeks and targeted healthcare professionals with experience of treating NTOS, ending May 2023.
What we found: Forty-six of 55 (83.6%) responses were used in the results. The majority worked in the NHS, with 41% (16/39) specialising in nerve teams, and most (58.7%, 27/46) had over 10 years of experience treating NTOS. Key findings included: NTOS assessment (performed by >91%) involved clinicians asking patients about their complaints and what conditions made them better/worse, looking at neck and shoulder movements, checking their reflexes, strength and feeling of their arms, and assessing a patient’s understanding of NTOS. Physiotherapy treatment (provided by >94%) consisted of advice and education to assist patients to manage their condition by providing them with exercises to increase the flexibility of the neck, shoulder and back. Three-quarters (76.1%, 35/46) of respondents reported an absence of treatment guidelines for NTOS, and 98% (45/46) expressed the need for further research into exercise and physiotherapy management for NTOS.
What this means: Clinicians feel NTOS is a complex condition that lacks treatment guidelines which could assist them in providing better care to patients. Physiotherapy remains highly recommended in current treatment pathways. Further research to understand what exercises should be provided to people with NTOS, and which people will benefit from them, would be beneficial.
Abstract
Objective: Neurogenic thoracic outlet syndrome (NTOS) is challenging to diagnose and manage. While physiotherapy is widely recognised as the primary treatment for NTOS, treatment specifics and target populations are poorly described. The objective of this cross-sectional survey was to explore the experiences and opinions of UK therapy and medical professionals regarding the assessment, diagnosis and physiotherapy management of patients with NTOS.
Methods: An online survey was distributed through a multimodal recruitment strategy employing snowball sampling. The survey remained active for 4 weeks and targeted healthcare professionals with experience of treating NTOS, ending May 2023.
Results: 46/55 (83.6%) responses were deemed eligible for analysis. 84.7% (39/46) worked in the NHS, with 41% (16/39) specialising in multidisciplinary team nerve services and most (58.7%, 27/46) having >10 years of experience treating NTOS. Key findings included: NTOS assessment (performed by >91%) involved taking a subjective history, evaluating cervical and shoulder active range-of-motion, upper limb neurological screening and assessing the patient’s understanding of NTOS. Physiotherapy treatment (provided by >94%) consisted of advice and education, range of motion exercises for the shoulder, cervical and thoracic regions, postural advice, activity modification and a home exercise plan. Three-quarters (76.1%, 35/46) of respondents reported an absence of treatment guidelines for NTOS, and 98% (45/46) expressed the need for further research into exercise and physiotherapy management for NTOS.
Conclusion: While clinicians perceive NTOS as a complex condition lacking treatment guidelines, physiotherapy remains a mainstay in the current treatment pathways. Further research is warranted to enhance the understanding of NTOS and develop evidence-based management strategies.
Introduction
Thoracic outlet syndrome (TOS) is a highly controversial medical diagnosis, as highlighted in a Cochrane review by Povlsen et al in 2014.1 Diagnosis is challenging due to the existence of four reported subgroups of TOS – namely, neurogenic, arterial, vascular and disputed – each presenting with diverse and wide-ranging symptoms.1-3
Authors describe three pertinent anatomical spaces of compression in TOS: the scalene triangle, costoclavicular and subcoracoid spaces.2-5
TOS is believed to be caused by congenital, acquired or traumatic factors, which subsequently create a compromised space for neurological/vascular structures to pass through. Neurogenic TOS (NTOS) refers to an assumed dynamic positional compression of the brachial plexus,6 which can present with an array of symptoms including neck/shoulder/arm pain, paraesthesia and weakness often exacerbated by repetitive overhead motions (occupational or recreational), and can lead to significant functional disabilities.2,3,5,7
NTOS stands out as the most elusive in terms of definition and diagnosis, often being referred to as a ‘diagnosis of exclusion’.2,8 Consequently, conducting studies that possess methodological homogeneity becomes exceedingly challenging.
Since the Cochrane review in 2014,1 considerable progress has been made in the field of TOS. An agreed clinical diagnostic criterion (CDC) by Thompson in 2016 provided a standardised framework for identifying and diagnosing TOS.9 Validation of these criteria against Patient Reported Outcome Measures (PROMs) has been completed.10 Furthermore, standardised reporting standards have been published by the Society of Vascular Surgeons (SVS) to encourage increased homogeneity of care through consistent reporting of TOS cases.11 However, it is unclear whether healthcare professionals are aware of these guidelines and are using them to support the management of NTOS.
Physiotherapy management and efficacy
Many papers refer to physiotherapy as a ‘mainstay’ of treatment.5 However, the descriptions of physiotherapy programmes are often insufficient, providing only brief summaries that are difficult to reproduce.12 Various papers state the aim of physiotherapy is to: ‘improve postural alignment’,3,4,13 ‘improve scapular control/stabilisation’7,14,15 along with ‘strengthening and lengthening exercises for the shoulder girdle muscles’.3-5,7,15
A recent publication by Goeteyn et al in 2022 marked the first randomised clinical trial (STOPNTOS) comparing continued physiotherapy with surgery for persistent NTOS, which was refractory to change with physiotherapy.7 Details of the physiotherapy regime for patients in this study were directed to previously published reviews.14,16 Although these reviews comprehensively describe a scapular stabilisation programme starting at rest and building through range, they document evidence of the programme’s effectiveness is anecdotal and not specifically linked to NTOS. They also acknowledged the need for high-quality research to determine the most effective conservative management strategies for individuals with NTOS. In the recent STOPNTOS trial,7 statistically significant differences in outcomes were reported favouring surgical intervention over continued physiotherapy in 50 randomised patients with persistent NTOS. It should be noted that the characteristics of patients who did respond favourably to physiotherapy were not described in this study.
The literature on the efficacy of physiotherapy in NTOS suggests that for many patients it is ineffective as, despite receiving physiotherapy treatment, a considerable proportion of patients (60–70%) still require surgical intervention.6,10,15 Additionally, it should be stated that currently, due to lack of standardisation of the assessment and treatment of NTOS, some patients may not respond to treatment for NTOS because the diagnosis may be incorrect.
There are two prospective studies in which a proportion of NTOS patients did respond favourably to conservative management and did not require surgery.10,15 Both studies used the CDC and SVS reporting guidelines to diagnose and classify their cohorts. 27% (40/150) of NTOS patients improved sufficiently with specific physiotherapy, with mean QuickDASH percentage change of 29.5±5.7%. Within this study,10 conservative treatment consisted of 4–6 weeks of stretching and ‘relaxing’ exercises for scalene and pectoralis muscles, along with shoulder girdle and scapular mobility, postural advice and breathing exercises. Mean follow-up for the physiotherapy group was 21.1 months. The remaining 60% of patients (90/150) did not respond sufficiently and underwent surgery, and achieved a higher percentage change in QuickDASH scores (47.9±3.6%).sup>10</sup Although not statistically significant, the patients who responded to therapy versus those requiring surgery trended towards having less severe symptoms at baseline.10
Unfortunately, in the other study,15 the 39.1% (186/476) of patients who were reported to respond effectively to physiotherapy and did not require surgery did not have their characteristics described or receive any follow-up visits. This limits the conclusions that can be drawn. Although characteristics were not described, the authors did state that physiotherapy was conducted for 6–12 weeks and consisted of ‘posture evaluation’, ‘scapular mobility’ and ‘shoulder girdle therapy’.
The current survey aims to address this gap by investigating practices among UK medical and allied health professionals (AHPs) regarding the assessment, diagnosis and physiotherapy management of people with NTOS.
Methods
Survey design and development
An online anonymous cross-sectional descriptive survey was used. Survey questions were piloted independently by four of the authors’ clinical colleagues. Ethical oversight and governance was granted by Keele University (REC- 0472 30/03/2023). The survey was designed and reported using the Checklist for Reporting Results of Internet E-surveys (CHERRIES).17
Study population
Respondents met the inclusion criteria if they were either a medical professional (surgeon or medical doctor) or registered AHP based in the UK with experience of caring for patients with NTOS.
Invitation and consent
The survey was hosted on the Microsoft 365 online platform via Microsoft Forms (www.office.com). A multimodal recruitment strategy was used to promote the survey via email, Twitter, the interactive Chartered Society of Physiotherapy (iCSP) website (http://www.csp.org.uk/icsp) and via the authors’ professional networks, including the British Association of Hand Therapists (BAHT) and the British Society for Surgery of the Hand (BSSH) membership. Peer-to-peer snowball sampling was encouraged. This method of sampling has been previously employed in other studies using online surveys.18
The survey opened for 4 weeks, closing on 2 May 2023 due to similar studies using this timeframe.19 Respondents were directed to an online information sheet outlining the purpose of the study, and provided assurances of anonymity and that completion was voluntary. Consent was assumed based on submission of the survey and this was explicit in the information sheet. Contact details and processes for outlining any concerns regarding the study were made explicitly clear. Confirmation of eligibility was required prior to commencing the survey. Ineligible responders were unable to proceed. The survey had to be completed in one sitting, with no function to partially save and return to complete at a later date.
Survey questionnaire
The survey’s primary aim was to explore AHP and medical professionals’ experience and opinions of the assessment, diagnosis and physiotherapy management of people with NTOS.
Thirty-five closed-style questions were asked with a combination of response options including dichotomous yes/no answers, multiple choice, 5-point Likert scales and free-text options.
The Likert scales ranged from ‘never’ to ‘always’ to describe the clinician’s frequency of use of certain diagnostic, assessment or physiotherapy treatments. To aid readability, and in conjunction with a similar survey,20 the respondents who selected ‘always’ or ‘sometimes’ have been combined to describe the most selected components. All future references to ‘commonly’ refer to this.
Data analysis
Data were imported into Excel (Microsoft Corps, Redmond, CA, USA) and analysed using descriptive statistics. The authors used a threshold of >70% of similar responses to indicate consensus, due to this threshold level being used in large consensus studies.21
Results
Survey response and characteristics
In the 4 weeks during which the survey was live there were 55 responders, of whom 46 (83.6%) indicated they met the survey’s inclusion criteria. 71.7% (33/46) were therapists, the vast majority being physiotherapists (32/33). Surgeons (92.3%, 12/13) were the most common medical professional to respond. 84.7% (39/46) of respondents worked within the NHS, with 41% working in specialist MDT Nerve Units (Table 1).

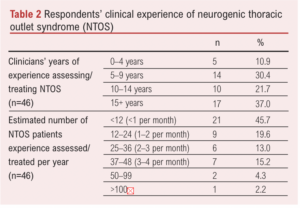
Clinical experience of NTOS
58.7% (27/46) of respondents had more than 10 years of clinical experience treating people with NTOS, with 54.3% (25/46) stating they saw at least 1–2 people with NTOS per month (Table 2).
NTOS diagnosis
91.4% of respondents (42/46) indicated that nerve conduction/electromyography studies were the most common diagnostic investigation used compared with 84.8% (39/46) for chest/ cervical plain x-ray and 82.6% (38/46) for brachial plexus magnetic resonance imaging. Targeted injections into scalene/pectoralis minor as part of a diagnostic work-up were ‘sometimes’ used by 43.5% (20/46) of respondents (Figure 1).
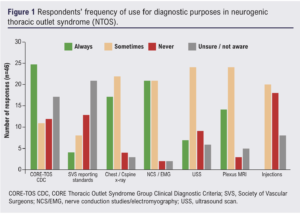
Implementation of published literature in NTOS in UK practice
Only 36.9% (17/46) of respondents stated that they used the CORE-TOS Clinical Diagnostic Criteria developed by Thompson,9 whereas 50% (23/46) either were ‘unaware’ or ‘never’ implemented it. Additionally, 56.6% (26/46) of respondents stated they were not aware or ‘never’ used the TOS reporting standards developed by Illig et al,11 although 26.1% used them commonly (Figure 2).
Clinical assessment of NTOS
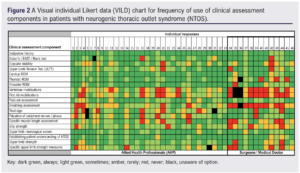
Commonly used assessment components (>70% of respondents)
All clinicians reported that taking a comprehensive subjective history was commonly part of the assessment. High agreement (>91%) of common use was also achieved for ‘cervical range of motion (ROM)’, ‘upper limb neurological screening’, ‘shoulder ROM’, ‘establishing the patient’s understanding of NTOS’, and the use of ‘clinical tests such as Adson’s/EAST/Roos’ (Figure 3).
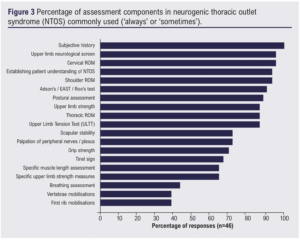
Less commonly used assessment components (<70% of respondents)
Six assessment components were reported by less than 70% of respondents of being performed at least ‘sometimes’. These were: ‘Tinel sign’ (67%, 31/42), ‘specific muscle length assessment’ (65%, 30/46), ‘specific upper limb strength measures’ (65%, 30/46), ‘breathing assessment’ (44%, 20/46) and both ‘vertebrae’ and ‘first rib’ mobilisations (both 39%, 18/46).
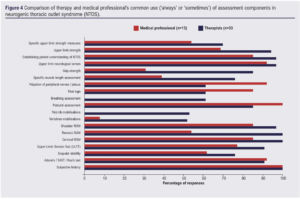
Comparison of AHPs’ and medical clinicians’ responses
Figure 4 provides a visual representation of the responses for clinical assessment based on the profession of the respondents. The largest percentage differences in responses favouring regular AHP use were observed in ‘breathing assessment’ (61%, 20/33 vs 0/13), ‘grip strength’ (54%, 28/33 vs 4/13), ‘first rib mobilisations’ (53%, 18/33 vs 0/13), ‘thoracic ROM’ (46%, 33/33 vs 7/13), ‘vertebrae mobilisations’ (44%, 17/33 vs 1/13) and ‘specific upper limb muscle length assessment’ (37%, 25/33 vs 5/13). Conversely, medical professionals favoured the use of ‘palpation of peripheral nerves/brachial plexus’ (31%, 13/13 vs 20/33) and ‘Tinel sign’ (24%, 11/13 vs 20/33) more frequently than their therapy counterparts.
Physiotherapy and NTOS
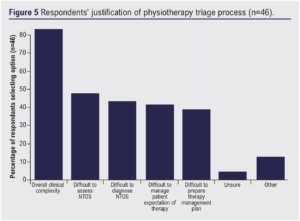
Triage of NTOS referrals to grade of therapist and justification
Over three-quarters of respondents (76.1%, 34/46) indicated that NTOS patients are triaged to either a highly specialised NTOS therapist or an experienced therapist within musculoskeletal specialty. Respondents were also asked their justification for why NTOS patients were referred to a particular grade of therapist (Figure 5). 82.6% (38/46) indicated that ‘overall clinical complexity’ was the main justification. Additionally, difficulty with assessment (47.8%, 22/46), diagnosis (43.5%, 20/46) and management of patient expectations (41.3%, 19/46) were indicated.
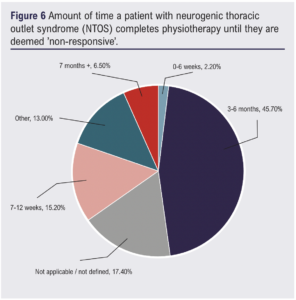
Timeframe, measuring response to physiotherapy and outcomes of physiotherapy informing future management
When asked about the period that patients with NTOS should engage in therapy, between 3 and 6 months was the most prevalent answer (45.7%, 21/46) (Figure 6).
In terms of interpreting the response of patients with NTOS to physiotherapy, there was a mixed response to the use of PROMs or specific objective markers. The vast majority (89.1%, 41/46) indicated that response to therapy was measured ‘subjectively via patient/therapist’.
Changes to specific NTOS objective tests such as EAST, Adson’s and ULTT, and changes in NTOS-specific PROMs (QuickDASH, Cervical Brachial Symptom Questionnaire, TOS Disability Questionnaire, etc) were indicated to be used in a minority of respondents with 36.9% (17/46) and 26.1% (12/46), respectively.
Physiotherapy treatment guidance for NTOS
Over three-quarters of respondents (76.1%, 35/46) indicated that there were no guidelines or protocol for their physiotherapy treatment for patients with NTOS.
Physiotherapy treatment package components
The frequency of use of physiotherapy treatment components for NTOS are presented visually in Figure 7.
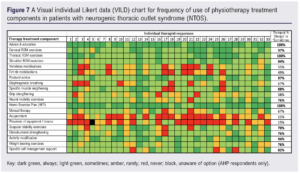
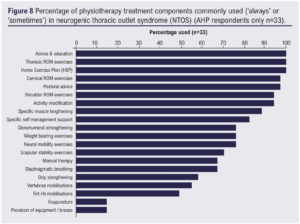
Provision of ‘advice and education’, a ‘home exercise plan’ and ‘thoracic ROM exercises’ were reported by 100% (33/33) of therapists as being commonly used as part of their treatment package. There was also high agreement for the use of ‘cervical ROM exercises’ and ‘postural advice’ (both 97%, 32/33), ‘shoulder ROM exercises’ and ‘activity modification’ (both 94%, 31/33).
Six other treatment components were reported by >70% of respondents as being commonly used (see Figure 8 for further details). Seven components received less than 70% agreement for commonly being part of a physiotherapy package for NTOS, with ‘acupuncture’ and ‘provision of equipment/braces’ having the lowest use at 15% (5/33).
Factors associated with a positive response to physiotherapy and overall physiotherapy rationale in NTOS management
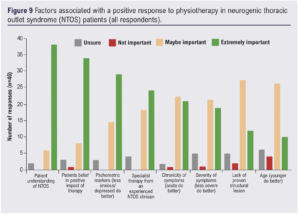
Clinicians’ thoughts on what factors may influence a positive response to physiotherapy in the management of NTOS are presented in Figure 9. A high level of ‘patient understanding’ (82.6%, 38/46) and patients having ‘belief in a positive response to therapy’ (73.9%, 34/46) received the highest gradings of being ‘extremely important’. Additionally, 52.2% (24/46) of respondents felt it was ‘extremely important’ to receive specialist therapy from an experienced NTOS clinician to promote a positive response to therapy.
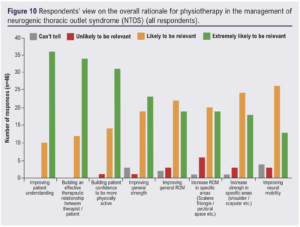
Clinicians were also asked what they thought was the ‘overall rationale’ for the role of physiotherapy in the management of patients with NTOS (Figure 10). ‘Improving patient understanding’ (78.3%, 36/46) and building an ‘effective therapist–patient therapeutic relationship’ (73.9%, 34/46) were deemed ‘extremely likely to be relevant’. ‘Improving neural mobility’ had the lowest proportion of clinicians feeling it was ‘extremely likely to be relevant’ to the overall rationale of physiotherapy in NTOS management (28.3%, 13/46), whereas ‘increasing ROM in specific areas’ such as the scalene triangle/pectoral space received the most responses of being ‘unlikely to be relevant’ (13%, 4/46).
Future research into exercise for NTOS
Finally, when clinicians were asked whether they thought further research into exercise/physiotherapy management of NTOS patients would be beneficial, 98% (45/46) stated ‘Yes’.
Discussion
This paper reports the findings of a cross-sectional survey of UK AHPs and medical professionals concerning the assessment, diagnosis and physiotherapy management of NTOS.
Main findings
Assessment
A comprehensive subjective assessment of NTOS was commonly undertaken by all clinicians who responded. This was most frequently (87%, 40/46) complemented with assessment of ROM (cervical, thoracic and shoulder), posture, upper limb strength and neurological screening; NTOS clinical tests (Adson’s, EAST/Roos, ULTT) and establishing a patient’s understanding of NTOS. Vertebrae/first rib mobilisations were rarely used as an assessment modality (39%, 18/46).
Medical professionals favoured the use of peripheral nerve palpation and the Tinel sign compared with therapists. The Tinel sign can be used to evaluate nerve compression, injury or regeneration, although its validity for use in NTOS is unknown.22
Implementation of published literature in NTOS in UK practice
In recent years, studies have attempted to address the heterogeneity of NTOS reporting by producing standardised reporting guidelines,11 with the aim of being able to reliably compare interventions for NTOS. However, according to this survey’s responses, these guidelines have not translated into UK practice to the extent they may have in the Netherlands where there have been multiple recent prospective studies.7,15,23 If higher quality research examining the management of NTOS in the UK is to be published, this needs to be addressed again. A UK TOS Registry24 has been mooted but has not come to fruition at the time of publication.
Although most respondents of this survey were not using or were not aware of the reporting standards or CDC for NTOS, the clinicians did indicate they were using many of the reporting standards’ recommended assessment components for NTOS, with a high use of clinical tests such as Adson’s, EAST and ULTT.
Physiotherapy treatment times and evaluation
The respondents of this survey echo other published literature that NTOS is a highly complex condition to both assess and treat.1,2 The majority stated that a highly specialised/experienced clinician was needed to treat these patients due to the overall clinical complexity.
The timeframe for NTOS patients receiving physiotherapy before it is deemed non-responsive in the literature is variable. Studies in the USA6,10 opt for shorter bursts of therapy compared with that reported in this survey (3–6 months), likely reflecting our different healthcare models. The majority (89.1%, 41/46) of respondents reported that a patient’s response to physiotherapy is measured through subjective questioning by the clinician, rather than using PROMs or objective clinical signs. The use of validated outcome measures to monitor patients’ progress has been recommended in best practice care.25 Three-quarters of responders also indicated that they have no local guidelines for treating NTOS, which may highlight the clinical uncertainty in NTOS.
Physiotherapy treatment
AHP respondents indicated that they most commonly prescribe interventions to aid and support self-management of NTOS. Advice and education, postural advice, activity modification, specific self-management support and a home exercise plan were all commonly provided more than 70% of the time. Additionally, exercises to improve ROM (shoulder, thoracic and cervical spine), glenohumeral strengthening, neural mobility and specific muscle lengthening (scalene and pectoralis minor) exercises were all commonly used by >70%.
Respondents indicated less common use (<55%) of ‘passive’ interventions such as acupuncture, provision of equipment and manual therapy/vertebrae mobilisations. This may be due to a general trend of moving away from hands-on therapy, with recent National Institute for Clinical Excellence (NICE) guidelines for back pain removing the recommendation of isolated manual therapy and acupuncture for common care.26
Therapists indicated that the level of a patient’s understanding of NTOS, along with their belief in a positive therapy outcome and having fewer psychosocial markers, may be correlated with a more favourable outcome for NTOS. These results align with a longitudinal cohort study of 1030 patients with shoulder pain27 and may be important if further work investigating clinical prediction rules for NTOS are conducted.
Clinicians felt the overall rationale for physiotherapy in the management of NTOS was more likely concerned with educating and coaching patients to assist with general improvements in physical activity, ROM and strength, rather than attempting to elicit specific muscle length, strength or neural mobility changes. Despite this, most clinicians in this survey reported that they provided both neural mobility (76%, 25/33) and specific muscle lengthening (88%, 29/33) exercises as part of their common treatment for NTOS. This highlights and mirrors both the uncertainty of rehabilitation for NTOS and wider musculoskeletal conditions, with studies arguing both for and against the effectiveness of region-specific exercises over general exercises in conditions such as spinal pain and knee osteoarthritis.28,29
Further research
98% (45/46) of clinicians felt that further research concerning exercise in NTOS would be beneficial, which has also been advocated by multiple authors.3,8,13-15 Expanding the knowledge base surrounding exercise and physiotherapy for NTOS could have wide-reaching implications in improving patients’ experiences, pathways and outcomes, in addition to potential efficiency savings for healthcare providers. For this to be achieved, we need to be able to produce homogeneous studies, allowing direct comparison of treatments with standardised assessments.
Although there are still understandable questions relating to the diagnosis of NTOS, in recent years since the introduction of the CORE Thoracic Outlet Syndrome Group (CORE-TOS) and SVS reporting standards there has been an emergence of randomised clinical trials7 and prospective studies,6,10,15 with repeatable comparable diagnostic criteria for the first time. This may suggest that now is the right time to build on this evidence base and lay the foundations for work in other contentious areas within the management of NTOS, such as the development of a consensus approach to physiotherapy management.
Limitations
Although the authors acknowledge that this is a small sample of clinicians, we feel the spread of clinicians from around the UK is a strength, given the small number of specialist MDT nerve services. In addition, the clinical experience of the respondents was substantial. The challenge of recruitment to online surveys has been well documented, as is the ability to calculate response rates.30
Conclusions
Most survey responders completed a comprehensive assessment for NTOS including subjective, objective and NTOS-specific clinical tests. AHPs prescribe treatments aimed at assisting self-management, in addition to exercises for ROM, strength and neural mobility. Passive interventions are less commonly prescribed.
Most clinicians recognise NTOS as a complex condition which requires experienced therapists to treat, although a patient’s response to physiotherapy is not measured consistently. Three-quarters of respondents did not have physiotherapy treatment guidelines to assist them. Clinicians are overwhelmingly in favour of further research pertaining to exercise and NTOS. In addition to research on physiotherapy, further efforts to standardise the assessment and treatment of NTOS within the UK are required.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023; 3(1): 36-45
Publication date:
November 19, 2023
Author Affiliations:
1. Physiotherapy, Upper Limb Therapy Department, Queen Elizabeth Hospital, Birmingham, University Hospitals Birmingham NHS Foundation Trust, UK
2. Consultant Upper Limb Physiotherapist and NIHR/CSP Doctoral Fellow, University Hospitals of Derby and Burton NHS Foundation Trust, UK
3. Professor of Physiotherapy, School of Allied Health Professionals, Keele University, UK
Corresponding author:
Joel O’Sullivan
Physiotherapy, Upper Limb Therapy Department, Queen Elizabeth Hospital, Birmingham, University Hospitals Birmingham NHS Foundation Trust, B15 2GW, UK
Email: Joel.o’sullivan@ uhb.nhs.uk











