Systematic review
Home-based high intensity interval training in patients with intermittent claudication: a systematic review protocol
Prosser J,1 Staniland T,2 Harwood AE,3 Ravindhran B,1 McGregor G,4,5 Huang C,6 Twiddy M,6 Nicholls AR,7 Ingle L,7 Long J,1 Chetter IC,1 Pymer S1
Plain English Summary
Why we undertook this work: Reduced blood flow to the legs can cause pain and cramping when walking and exercising. For people with this condition, the recommended treatment is a supervised exercise programme (SEP). However, most vascular centres do not have access to a SEP and, when they do, most patients are unable to attend as it is conducted face-to-face, requiring a significant time and travel commitment. We therefore developed a shorter, less time-consuming high intensity interval training (HIIT) programme which could be easier to provide and more attractive to patients. It means exercising a little bit harder than during the normal SEP, but over a shorter time period. When we tested this programme we found that, despite it requiring less time to complete, most patients still did not want to attend as they were still having to travel to a hospital/community venue to complete their exercise. Therefore, we need to find different ways of providing exercise programmes that reduce the need to attend a hospital or community centre so that more people can perform them. Having the option of participating at home with live remote supervision may be one way. The existing research suggests that SEPs can already be delivered this way, although it is less clear if HIIT can.
What we will do: We plan to look at all the existing research to see how HIIT can be safely delivered at home for people with reduced blood flow to the legs.
What this means: A review of the evidence will help us plan how we can deliver HIIT at home with live remote supervision. Once we have this information, we can compare HIIT with traditional SEPs with the option of attending in person or remotely.
Abstract
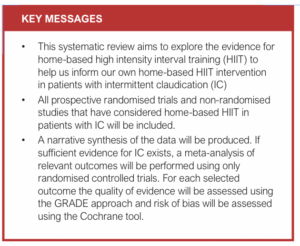
Introduction: The aim of this systematic review is to consider the evidence base for home-based high intensity interval training (HIIT) in patients with intermittent claudication (IC). Prior knowledge of the evidence base suggests that there may be little research considering HIIT in patients with IC. If so, the evidence base across all cardiovascular diseases will be considered.
Methods: Medline, EMBASE, CINAHL and Cochrane CENTRAL databases will be searched for terms including ‘peripheral arterial disease’, ‘intermittent claudication’, ‘home-based exercise’, ‘high intensity interval training’ and ‘home-based high intensity interval training’. All prospective randomised trials and non-randomised studies considering home-based HIIT in patients with IC will be included. Studies will not be excluded based on the use of a comparator arm, meaning single-arm studies as well as multi-arm trials will also be included. If appropriate, based on the extant literature, a meta-analysis of randomised controlled trials will be conducted. The outcomes of interest will include intervention components, intervention feasibility (based on uptake and completion rates), intervention tolerability (based on compliance and adherence to the intervention), maximum walking distance, pain-free walking distance, quality of life and cardiorespiratory fitness.
Conclusion: This review aims to assess the evidence for home-based HIIT in patients with IC, to establish its feasibility and to inform the refinement of an existing supervised HIIT intervention to allow it to also be delivered remotely. Following this, a pilot randomised controlled trial to compare HIIT versus usual care supervised exercise programmes will be developed. For this, the interventions will be delivered either in person or remotely in real-time, depending on centre availability and patient preference.
Introduction and rationale
Peripheral arterial disease (PAD) is caused by atherosclerosis of the arteries supplying the lower limbs, limiting blood flow to the legs.1 PAD is estimated to affect more than 237 million people worldwide and its prevalence is increasing.2 Intermittent claudication (IC) is the classical symptom of PAD, and is characterised by a reproducible ambulatory muscular leg pain secondary to an oxygen supply/demand imbalance that is relieved by rest.1
IC carries an increased morbidity and mortality risk1,3,4 which also reduces functional capacity and quality of life.3,5 The first-line treatment for IC, as recommended by the National Institute for Health and Care Excellence (NICE), is cardiovascular risk reduction and, for symptomatic benefit, a supervised exercise programme (SEP).6 The SEP should consist of two hours of supervised exercise per week for a period of 12 weeks, with patients encouraged to exercise to the point of maximal pain.
Evidence for SEPs is irrefutable, providing superior improvements in walking distances compared with home-based exercise programmes (HEPs) and basic walking advice7 and comparable longer-term improvements compared with more invasive interventions.8 Despite this evidence and the NICE recommendations, SEPs suffer from suboptimal provision, uptake and completion. In the UK, only 48% of centres have access to a SEP, with funding, staffing, facilities and equipment being key barriers.9 When SEPs are available, fewer than 25% of patients attend and, of these, only 50–75% complete the programme.10,11 Patient-related barriers include the time commitment required to attend and complete a SEP.10,12
These barriers led our group to explore a time-efficient alternative in the INITIATE study which investigated the feasibility and acceptability of cycle-based high intensity interval training (HIIT) in two UK centres, a theoretically more attractive and easier to deliver exercise programme for patients with IC.13,14 The INITIATE study also attempted to answer priority 2 of the James Lind Alliance priority setting partnership “How can we improve provision and access to exercise programmes for patients with PAD?”.15 The results showed that actively supervised cycle-based HIIT improves completion rates and appears to be safe and efficacious. Unfortunately, the uptake rates were comparable to SEPs and remained low at 25%. This is because patients were still required to attend face-to-face sessions and, although the time commitment of HIIT was 50% less than for SEPs, the additional logistical burden associated with centre-based programmes including transport/travel and inflexible timings remained.12,16 The limited access and uptake for SEPs/HIIT also means that the feasibility of a randomised controlled trial comparing these exercise therapies in their current form is questionable.
A more adaptable approach to supervised exercise therapy, both in terms of SEPs and HIIT, is required. One such approach, which has been delivered in other patient cohorts, is via real-time remote delivery whereby patients exercise at home with real-time supervision provided via video conferencing (eg, Zoom).17 This adaptation could improve the possibility of a randomised controlled trial as centres without a standard SEP could refer their patients to receive their allocated exercise therapy remotely. Centres with SEP provision can offer patients the choice between in-person or remote delivery. This adaptable provision is also likely to translate to clinical practice should it prove efficacious, potentially increasing access, uptake and adherence. Although HEPs are considered inferior to SEPs for patients with IC, a real-time remotely delivered programme, despite being performed at home, would be considered a SEP. Additionally, HEPs with remote monitoring (albeit not in real time) appear to be equivalent to traditional SEPs in terms of health-related outcomes, providing evidence to suggest that the proposed model has promise.7,18 Although no study has considered home-based, real-time, remotely delivered SEPs for patients with IC, the current evidence base for HEPs does suggest that a SEP, mirroring the traditional programme, can be feasibly delivered in this way.19,20
The current evidence base, however, does not consider the role of home-based HIIT for patients with IC, either remotely delivered or otherwise. Additionally, the cycle-based nature of the current INITIATE HIIT programme means that it cannot be delivered remotely due to the logistical challenge of equipment availability/delivery. It is therefore not known if patients with IC are able to perform HIIT in a home-based setting (with or without supervision), and if they are, how it should be delivered. The aim of this study is therefore to review the evidence for home-based HIIT in patients with IC to establish its feasibility and to inform the refinement of our HIIT intervention to allow it to also be delivered remotely. Prior knowledge of the evidence base suggests that there may be little research considering home-based HIIT in patients with IC.21 If so, the evidence base across all cardiovascular diseases will be considered (cerebrovascular, coronary and peripheral arterial disease).
Methods
This protocol is written in accordance with the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) guidelines.22
Search strategy and inclusion criteria
The Medline, EMBASE, CINAHL and Cochrane CENTRAL databases will be searched from inception for terms including ‘peripheral arterial disease’, ‘arterial occlusive disease’, whilst also including terms such as ‘high intensity interval training’ and ‘home-based exercise’ (see full draft search in Appendix 1 online at www.jvsgbi.com). In addition to the databases, trial registers such as clinicaltrials.gov and the Web of Science conference proceedings will be searched. Should any relevant abstracts be identified, the authors will be contacted to obtain study outcome reports, if available. Only studies using the English language will be considered in this review and no date restrictions will be applied.
Population: All prospective randomised trials and non-randomised studies evaluating a home-based HIIT programme in patients with IC (Fontaine II/Rutherford stages 1–3) will be included. Studies including other PAD subgroups (eg, asymptomatic or chronic limb-threatening ischaemia) will be excluded.
Intervention: All studies which use HIIT, defined as an interval approach conducted at >85% peak heart rate (HRPeak) or another surrogate measure (ie, >80% maximal exercise capacity or peak oxygen uptake (VO2Peak) or a rating of perceived exertion >15) performed in a home-based setting, will be included.21 Studies will not be excluded based on the duration, frequency or protocol (ie, ratio between length of exercise and rest periods) used. HIIT can be prescribed via structured advice given in a similar fashion to traditional HEPs18,23 with or without remote monitoring (via pedometers, accelerometers, physical activity monitors or exercise diaries) or delivered remotely in real time (via a video conferencing/communication platform). Although the former is considered a HEP and the latter a SEP, the aim of this review is to identify if and how HIIT can be performed in a home-based setting to inform our intervention. Therefore, the mode of delivery is less important at this stage.
Comparator: Studies will not be excluded based on the use of a comparator arm. This means single-arm observational cohort studies as well as multi-arm comparative studies will be included. Comparator groups may include centre-based SEPs, HEPs, exercise advice and non-exercise controls.
Outcomes: Because of the aim of this review, studies will not be excluded based on the reporting of certain outcomes. However, outcomes of interest include intervention components, intervention feasibility (based on uptake and completion rates), intervention tolerability (based on compliance and adherence to the intervention), maximum walking distance, pain-free walking distance, quality of life and cardiorespiratory fitness.
Should no studies meet the above inclusion criteria, the population criteria will be widened to include those with other cardiovascular diseases (coronary or cerebrovascular) with the intervention, comparator and outcome criteria remaining the same.
Data management, selection and collection process
Results from the database searches will be uploaded to the Covidence systematic review software (2024, Veritas Health Innovation, www.covidence.org). Two independent reviewers will screen the titles and abstracts identified by the database searches. Studies deemed potentially eligible will be further interrogated with a full-text review. Any disagreements between the two reviewers will be resolved via consensus or by consultation with a third reviewer. The use of Covidence will allow for the automated production of a PRISMA flow diagram.22
Two independent reviewers will then perform the data extraction using a standardised form which will be input and managed using a Microsoft Excel database (Microsoft Office, 2016). Where any discrepancies are identified, the original source will be reviewed and the correct data will be extracted and input into the final form. Data extraction will include study characteristics (including appropriate information to assess the quality of the study), a description of the participants (inclusion/exclusion criteria applied), sample size, study design, a description of the intervention and any comparators, adverse events, length of follow-up and main findings related to outcome measures.
Risk of bias and rating the quality of evidence
For randomised controlled trials the risk of bias will be assessed by two independent reviewers using the Cochrane Risk of Bias 2.0 tool.24 This assesses the risk of bias as ‘high’, ‘low’ or ‘some concerns’ across five domains including: bias arising from the randomisation process; bias due to deviations from intended interventions; bias due to missing outcome data; bias in measurement of the outcome; and bias in the selection of the reported result. In the event of disagreement between the two reviewers, this will be resolved by consensus or via discussion with a third reviewer. The bespoke Excel tool will be used to manage and record the assessments (https://www.riskofbias.info/welcome/rob-2-0-tool/current-version-of-rob-2), which will be summarised with justifications for each outcome across all domains using the risk of bias table. The least favourable assessment across all domains will be used for the overall risk of bias for each trial.25
Risk of bias in non-randomised studies will be assessed using the Risk Of Bias In Non-randomised Studies of Interventions (ROBINS-I) tool whereby specific signalling questions will elicit information relevant to the risk of bias. The risk of bias judgement will be low, moderate, serious or critical based on the responses to these questions.
The quality of the evidence will be assessed by two independent reviewers using the GRADE approach.26 For this assessment, the reviewers will initially consider the design of the trials that contribute to the evidence before upgrading or downgrading based on risk of bias, inconsistency, indirectness, imprecision and publication bias. All evidence will be rated as high, moderate, low and very low.26
Data analysis and synthesis
Given the aim of this study, the inclusion of both randomised trials and non-randomised studies and our prior knowledge of the evidence base, it is likely that only a narrative synthesis of the included studies will be provided, especially if it is necessary to widen the population criteria.
However, should sufficient evidence be available for patients with IC, meta-analyses will be performed of the relevant outcomes using only randomised controlled trials. Meta-analyses will be performed using Review Manager Web (RevMan web, 2022) to produce forest plots and associated 95% confidence intervals. The model used and the appropriateness of meta-analyses will be based on the assessment of heterogeneity considering the I2, T2 and χ2 statistics and associated p values.
Discussion and conclusion
The proposed review aims to consider the evidence for home-based HIIT in patients with IC to establish its feasibility and to inform the refinement of an existing supervised HIIT intervention to allow it to also be delivered remotely. This work will support our already established body of work considering supervised HIIT in this population.13,14,21,27 Once the supervised HIIT intervention is refined to also allow it to be delivered at home, a pilot randomised controlled trial comparing HIIT with usual-care SEPs will be performed. For this trial, both interventions will be delivered either in person or remotely in real time, depending on centre availability and patient preference.
There are possible limitations that may occur within the proposed review. These are mainly related to a potential lack of evidence. It is possible that there will be no studies considering home-based HIIT for patients with IC. However, the impact of this will be minimised by the intention to widen the population criteria.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(3):155-159
Publication date:
April 24, 2024
Author Affiliations:
1. Academic Vascular Surgical Unit, Hull York Medical School, Hull, UK
2. Hull University Teaching Hospitals NHS Trust, Hull, UK
3. Department of Sport, Health and Exercise Science, Institute of Sport, Manchester Metropolitan University, Manchester, UK
4. Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick, Coventry, UK
5. Centre for Sport Exercise and Life Sciences, Institute for Health and Wellbeing, Coventry University, Coventry, UK
6. Hull York Medical School, University of Hull, Hull, UK
7. School of Sport, Exercise, and Rehabilitation Science, University of Hull, Hull, UK
Corresponding author:
Jonathon Prosser
Academic Vascular Surgical Unit, Tower Block, Hull Royal Infirmary, Hull HU3 2JZ, UK
Email: Jonathon.Prosser @nhs.net











