ORIGINAL RESEARCH
Long-term outcomes of major and minor lower limb amputation: eight-year retrospective analysis from a single tertiary referral centre
Bergman H,1 Clay B,2 Lane T3,4
Plain English Summary
Why we undertook the work: Amputations of the leg, feet and toes are being carried out more commonly as time goes on. Historically, patients undergoing amputation have poor outcomes after surgery. These patients often die within a year of the procedure, require multiple additional amputations and have a poor quality of life. We aimed to assess the outcomes of patients who underwent lower limb amputations in a large hospital performing many such procedures every year.
What we did: Using electronic patient records, we assessed the outcomes of patients who had undergone lower limb amputations in the 8 years prior to the study. We assessed their rates of death over time, particularly looking at how many patients had died at 30 days post-procedure and 1 year post-procedure. We also assessed the rates of patients requiring further amputations, their level of function with prosthetics 6 months after the procedure and how these measures changed over the 8-year period investigated.
What we found: For patients receiving major amputations of the leg (above-knee or below-knee amputations), 8% died by 30 days post-procedure and 24% died by 1 year post-procedure. This is a sign of how unwell patients having these amputations are, rather than that the operation itself causes death later. Patients receiving minor amputations (toes and middle of the foot) were more likely to undergo further amputation procedures. In patients who were fitted with prosthetic legs, all patients showed similar levels of function with their prosthetic limb regardless of what specific type of amputation they had.
What this means: Patients having any kind of amputation have significant risks of dying in the following year and needing further amputations. These risks should be thoroughly discussed with all patients who are being offered amputation so that they can make fully informed decisions.
Abstract
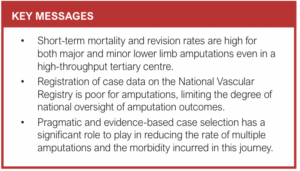
Objective: Lower limb amputation is increasingly common yet outcomes are historically poor, with high rates of short-term mortality, revisions and poor quality of life. This observational study evaluates outcomes from a high-volume tertiary vascular referral centre.
Methods: Retrospective electronic case note review was performed to elicit all major and minor amputations performed between 03/11/2014 and 31/05/2022 for peripheral arterial disease and diabetic foot sepsis. Cases of amputation for trauma or chronic pain were not included.
Results: A total of 1,566 amputations (865 major, 701 minor) were carried out in 1,237 patients during the study period. Mortality was significantly higher for patients undergoing major amputation compared with minor amputation at 30 days (7.9%, n=61/773 vs 1.0%, n=6/575; p<0.0001) and at 1 year post-procedure (23.7%, n=183/773 vs 13.6%, n=78/575, p<0.0001). Revision rates were significantly lower for major amputations than for minor amputations at 30 days (2.4%, n=19/799 vs 13.2%, n=91/691; p<0.0001) and at 1 year post-procedure (10.0%, n=68/677 vs 26.3%, n=163/619, p<0.0001). Of the patients with major amputation fitted with a prosthesis, there was no significant difference in the numbers of patients ambulating (p=0.19) or the mean ambulatory level (p=0.08) between above-knee and below-knee amputation at 6 months post-procedure.
Conclusions: Both major and minor lower limb amputations are associated with a high risk of revision and mortality within 1 year which should be discussed explicitly as part of the informed consent process.
Introduction
Major amputation is a life-changing yet common endpoint in the management of diabetic foot disease (DFD) and chronic limb-threatening ischaemia (CLTI). Less commonly, amputation is performed for traumatic limb injury, deformity, chronic pain or loss of function.1–4 Major amputation is estimated to affect 3–4% of all patients with peripheral arterial disease (PAD)5 and 15–20% of those with CLTI.6 When revascularisation fails, sepsis requires source control, pain is insurmountable or limb function is inadequate, major amputation is the terminal option to preserve life over limb.
Despite increasing numbers of major amputations being performed annually in the UK – more than 3000 major amputations were performed in 20217 – outcomes remain poor. This may be due to the generalised frailty and severely comorbid nature of this cohort.8 There are well-documented high rates of revision to a higher level, major adverse cardiovascular and cerebrovascular events and short-term mortality in the literature, with below-knee amputations (BKA) and above-knee amputations (AKA) having 4.1% and 8.7% 30-day mortality, respectively, in the National Vascular Registry (NVR) 2022 report.7
Cambridge University Hospitals is a tertiary vascular referral centre receiving all referrals for lower limb ischaemia (acute, chronic, diabetic, traumatic) within the wider region in a hub and spoke model, serving a population of approximately 1.8 million. All major limb amputations are performed in the hub, with rehabilitation starting centrally before continuing in the spoke.
Here we assess 8 years of experience encompassing the years from 2014 to 2022 of major and minor amputation from a single high-volume tertiary referral centre to give an overview of the outcomes of contemporary practice and utilisation of the NVR.
Methods
Local approvals
Service evaluation approval was sought through the Cambridge University Hospitals NHS Foundation Trust Research and Development Department (registration number PRN10636).
Standardised practice
Major amputation was performed routinely as per an ‘amputation pathway’. All amputations were performed under the supervision of a consultant vascular surgeon with a standardised approach in terms of planning, marking, limb division, haemostasis and flap reconstruction. All patients received a catheter inserted into the sciatic or tibial nerve with local anaesthetic infused for 5 days postoperatively, except in rare cases where a nerve was not identified. The authors acknowledge the ongoing trials surrounding the use of nerve catheters in amputation and the potential for practice changing in the future. All patients received a 5-day course of prophylactic antibiotics, DVT prophylaxis and their usual antiplatelet within 24 hours postoperatively. All major amputations received a wound drain which remained in situ for 48 hours or until output had ceased. All patients received a dressing comprising a non-adhesive layer directly contacting the wound, followed by gauze, wool and crepe bandage. All wounds were routinely inspected at 5 days postoperatively unless clinically indicated sooner (eg, bleeding or sepsis). Finally, all patients undergoing elective or semi-elective amputation were offered a preoperative consultation with the amputation physiotherapist (for emergency amputations, this was seldom possible) and postoperative intensive physiotherapy to fast-track rehabilitation and discharge planning. Revisions were primarily performed due to non-healing or progressive ischaemia of the stump.
Procedures were only performed out of hours if necessitated due to emergent sepsis or ischaemia that was acutely life-threatening. Any major amputation performed out of hours was performed with at least direct supervision in theatre by a consultant vascular surgeon. In the majority of cases this would mean the supervising consultant being scrubbed and performing or partially performing the procedure as per NVR guidance.
The unit acknowledges the Commissioning for Quality and Innovation framework for the expedited management of patients with CLTI and, where possible within the limitations of theatre, bed and staff availability, this standard was targeted.
Data collection
Retrospective case note review was performed via the EPIC Hyperspace patient management platform to elicit all patients undergoing major or minor lower limb amputation between 03/11/2014 and 31/05/22. Patients were only included if there was a hospital coding or inpatient episode where an amputation procedure was undertaken due to sequelae of PAD or DFD. Cases of amputation due to trauma or chronic pain without primary vascular compromise were not included. Through-knee amputations were not performed at this centre during the study period so were not captured.
Baseline patient demographics including postcode, date of birth, sex and age were recorded. Mortality status was interrogated for all patients to determine date of death, post-procedure days to death and the 30-day and 1-year mortality. Where mortality data were missing, the inter-hospital data spine, connected to all local hospitals and GP practices, was interrogated to complete the dataset.
Multiple instances of amputation in the same limb in the same patient recorded at separate time points were coded as revisions with interval to revision, level of revision and subsequent mortality status recorded for all instances.
Rehabilitation outcomes were extracted from prosthetic clinic notes. These visits were performed routinely at approximately 6 months following discharge. Rehabilitation outcomes were only available for local Cambridge patients (approximately half the cohort) due to the large geographical area over which prosthetic services are offered. All patients fitted with a prosthesis received a prosthesis-related functional status ‘K’ score (0: no prosthesis, 1: cosmetic or transfer only, 2: ambulatory inside the home, 3: ambulatory outside the home, 4: high level of activity).
Case ascertainment was determined by cross-checking the EPIC Hyperspace and NVR reports for the study duration.
Statistical analysis
Statistical and graphical analyses were performed on Microsoft Excel v16 and IBM SPSS v29. Data were analysed with the patient as the unit of analysis. All tests of statistical significance were two-tailed. A p value of 0.05 was used as the threshold for statistical significance for all analyses.
Rates of mortality and revision were calculated at 30 days and 1 year post-procedure and presented as proportions. The mortality risk at 30 days and 1 year post-procedure was compared between amputation types with relative risk. Patients who died before 30 days or 1 year were removed from inclusion in calculations of the revision rate. Patients who underwent multiple revisions were included multiple times in calculations of revision.
Kaplan–Meier survival analysis was carried out for mortality after the index procedure. Patients were censored at their date of death or at the end of the outcome reporting period assessed. Statistical significance of Kaplan–Meier analysis was determined with the Mantel–Cox log rank measure with pooled and paired analyses performed.
Rehabilitation outcomes were presented as proportions of patients achieving a given K score at their 6-month outpatient rehabilitation visit. Patients were included twice in analyses if they were referred for prosthesis for separate AKA and BKA, even if in the same limb. Mean rehabilitation K scores were calculated for AKA and BKA cohorts and compared using an unpaired t-test.
Subgroup analyses of mortality, revision rate and rehabilitation outcomes were performed for each modality of amputation and the cohort of patients with revised amputations.
NVR utilisation was calculated using procedure rather than patient as the unit of analysis.
Caseload, 30-day and 1-year rates of mortality and revision and volume–outcome relationships were calculated for the years 2015–2021 and, where the data fit a linear trendline, the strength of correlation was tested using Pearson’s R.
Results
Study cohort
A retrospective review of the electronic patient record returned a total of 1,566 amputations carried out in 1,237 patients for PAD or DFD over the period. The proportions of each amputation type, average age and gender ratio are shown in Table 1.
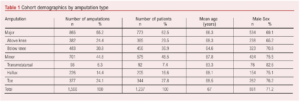
Mortality
Major amputation carried 30-day and 1-year mortality risks of 7.9% (n=61/773) and 23.7% (n=183/773), respectively, and minor amputation carried 30-day and 1-year mortality risks of 1.0% (n=6/575) and 13.6% (n=78/575), respectively. Thirty-day and 1-year mortality for each amputation type is shown in Table 2.
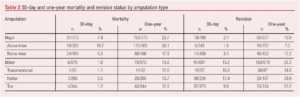
Major amputation was associated with a significantly higher risk of mortality than minor amputation at 30 days (RR=7.6 (95% CI 3.3 to 17.4), p<0.0001) and at 1 year (RR=1.7 (95% CI 1.4 to 2.2), p<0.0001). AKA was associated with a significantly higher risk of mortality than BKA at 30 days (RR=2.0 (95% CI 1.2 to 3.3), p=0.005) and at 1 year (RR=1.7 (95% CI 1.3 to 2.2), p<0.0001).
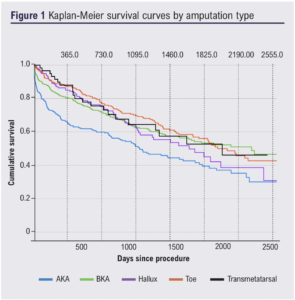
Kaplan–Meier survival curves were plotted for each amputation type (Figure 1). Amputation type was a statistically significant modulator of survival (p<0.001) when assessed by pooled analysis. Major amputation overall was found to result in significantly poorer survival than minor amputation over the study period (p=0.001), with survival poorer for the entire first 5 years post-procedure. AKA was found to have a significantly lower survival than all other amputation types: BKA (p<0.001), transmetatarsal (p=0.015), hallux (p=0.003) and toe (p<0.001). No other amputation was found to confer significant survival benefit relative to another, including within minor amputations (p=0.32).
Revision
Overall, 18.9% (n=234/1,237) of patients underwent a revision of amputation during the study period. Of the patients who were still alive following major amputation there was a 30-day revision rate of 2.4% (n=19/799) and a 1-year revision rate of 10.0% (n=68/677). The risk of revision for minor amputations was significantly higher than for major amputations at 30 days (13.2%, n=91/691, RR=5.5, p<0.0001) and at 1 year (26.3%, n=163/619, RR=2.6, p<0.0001). The 30-day and 1-year rates of revision for each amputation type are shown in Table 2.
For minor amputations, the rate of revision to major amputation at 30 days was 6.1% (n=42/691), with these revisions representing 46.2% of all revisions of minor amputations at 30 days. At 1 year the rate of revision to major amputation was 11.8% (n=73/619), with such revisions amounting to 44.8% of revisions of minor amputations at 1 year.
Rehabilitation
Of the 773 patients who underwent major amputation, 56.9% (n=440) were referred to prosthetic services in Cambridge and fitted with a prosthesis, with the remainder either referred to prosthetic centres outside the retrievable catchment area or not referred at all. Of the 440 patients referred within Cambridge, rehabilitation outcomes were reported for 97.5% (n=429/440) with 11 patients lost to follow-up.
Of the 429 patients with reported rehabilitation outcomes, 27.3% (n=117) had undergone AKA and 72.7% (n=312) had undergone BKA. At 6 months post-procedure there was no significant difference (RR=1.1, p=0.19) in the levels of patients who were ambulatory (K score >1) with their prosthesis between AKA (51.3%, n=60/117) and BKA (58.7%, n=183/312). The mean ambulatory level (K score) of patients fitted with a prosthesis was not significantly different (p=0.08) between AKA (mean=1.55, SD=0.79) and BKA (mean=1.71, SD=0.85).
NVR utilisation
NVR case ascertainment for major amputations within the study period was 56.3% (n=487/865), comprising rates of 54.7% (n=209/382) for AKA and 57.6% (n=278/483) for BKA. For minor amputations, case ascertainment was lower: 3.6% overall (n=25/701), 7.1% (n=7/98) for transmetatarsal, 3.5% (n=8/226) for hallux and 2.7% (n=10/377) for toe amputations.
Temporal trends
In the seven years from 2015 to 2021 with complete capture of all amputations performed, linear trendlines showed that the overall caseload increased over time (Figure 2). The major amputation caseload increased over time with individual increases in both AKA and BKA. The minor amputation caseload decreased slightly over time, primarily due to a decrease in toe amputations, while transmetatarsal amputations increased slightly and hallux amputations remained stable over time.
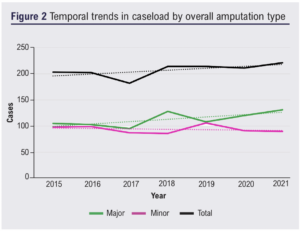
On a per-patient basis, 30-day mortality did not change significantly between 2015 and 2021 for patients undergoing major (R=0.18, p=0.71) or minor (R=–0.16, p=0.73) amputation. One-year mortality also did not change significantly for major (R=–0.61, p=0.15) or minor (R=0.34, p=0.46) amputation.
On a per-procedure basis, the 30-day revision rate did not change significantly between 2015 and 2021 for patients undergoing major (R=–0.26, p=0.57) or minor (R=0.71, p=0.08) amputation. The 1-year revision rate also did not change significantly for major (R=–0.40, p=0.38) or minor (R=0.35, p=0.44) amputation.
Considering volume–outcome relationships with respect to mortality, major amputation showed no significant correlation between caseload and 30-day mortality (R=0.35, p=0.44) or 1-year mortality (R=–0.14, p=0.77). Similarly, minor amputation showed no significant volume–outcome relationship for 30-day mortality (R=–0.40, p=0.38) or 1-year mortality (R=0.47, p=0.29). With respect to revision rates, major amputation again showed no significant correlation at 30 days (R=–0.25, p=0.59) or at 1 year post-procedure (R=–0.65, p=0.11). Minor amputation also showed no significant relationship for 30-day (R=0.35, p=0.44) or 1-year revision rates (R=–0.06, p=0.90).
Discussion
These data describe the outcomes of major and minor amputations performed between 2014 and 2022 in a tertiary vascular referral centre.
The observed rates of 30-day and 1-year mortality are comparable to the wider literature.7,9-11 Survival analysis revealed significantly inferior survival for major compared with minor amputation, with survival lower over the first 5 years. This may reflect the physiological impact of a larger surgery and a greater volume of compromised tissue. Despite this, major and minor amputation survival curves begin to converge at 5 years, indicating the overall poor prognosis of any patient with CLTI and their significant frailty. Compared with other disease processes, even a minor amputation carries a comparable 1-year mortality risk to breast cancer12 and a similar 5-year survival to lung cancer.13
The 1-year mortality rate was high, as expected, with this thought to reflect the systemic burden of atherosclerotic disease not just on the limbs but also on the coronary, renal and cerebral vasculatures.
Hallux and transmetatarsal amputations were found to have the highest rates of revision of any amputation type at 30 days and 1 year, respectively, in accordance with the wider literature.14 When minor amputations were revised, approximately half of them were revised to a major amputation. Clinicians should be aware of the high rate of treatment failure with these strategies and the need for strict post-procedural wound care and cautious ambulation. Selection of a more definitive and durable intervention may be appropriate in some cases.
The inclusion of both major and minor amputations in this study, despite their different but overlapping aetiologies, was useful to allow identification of high-risk minor amputation types – hallux and transmetatarsal. Additionally, the results regarding need for revision, including revision to major amputation, highlight the likely insidious longitudinal progression of repeated minor amputations ultimately towards major amputation. In light of this, in some cases this journey may be beneficently shortened through more fastidious case selection for minor amputations and the selection of a single definitive major amputation rather than pursuing multiple minor amputations.
Positive volume–outcome relationships have previously been reported for carotid endarterectomy and open abdominal aortic aneurysm (AAA) repair15,16 whereby the more procedures a unit completes, the better their outcomes. This ‘learning curve’ relationship has not been observed here – instead, no significant volume–outcome relationship was demonstrated for major or minor amputations with respect to mortality and revision at 30 days and 1 year post-procedure. This may reflect the lower degree of technical complexity of amputations compared with carotid endarterectomy and AAA repair.
The NVR estimates its own major amputation case ascertainment at 87% nationally,7 aided by the automatic generation of an NVR entry for completion during admission for major amputation. Therefore, the observed rate of 56.3% at a tertiary referral centre is particularly notable. Factors which may contribute to this low rate include the performance of many amputations by more junior vascular trainees who may not be registered with or familiar with the NVR; a reduced focus on completion of NVR entries for amputations compared with the three key index vascular procedures (AAA repair, carotid endarterectomy and limb bypass); the frequent performance of amputation out of hours; and simply that there is limited time to complete paperwork during routine clinical practice. Methods to improve fulfilment of the clinician’s responsibility to complete NVR entries could include annual reviews of personal case ascertainment rates during appraisals; teaching sessions to familiarise junior trainees about the importance of the NVR; assurance of access to the NVR by all surgical practitioners; and teaching regarding the practicalities of completing NVR entries for key vascular procedures.
The very low rate of ascertainment for minor amputations is less notable given the lack of automatic NVR entries for minor amputation and the context that minor amputations are often completed alongside a simultaneous revascularisation procedure and patients may undergo multiple interventions (including minor amputation) during a single admission, making them difficult to capture in terms of clinical coding. Given the frequency at which these procedures are performed and their high rate of revision to major amputations at later dates, judicious documentation of minor amputations should be a key development priority for the platform.
Linking of mandatory forms such as the NVR to electronic patient records and streamlining routine data collection are key challenges for the healthcare system to tackle to improve patient safety and the accuracy of reporting. Failure to document reduces our ability to track local, regional and national trends and hampers epidemiological research.
These results and conclusions are likely to be generalisable to other tertiary vascular centres in the UK due to the high caseload of the Cambridge Vascular Unit serving a catchment population over approximately 2 million spanning multiple counties, socioeconomic groups and the full scale of the deprivation index. Furthermore, the outcomes reported here are comparable to those of similarly sized centres in the NVR report.7
The contemporary outcomes data described could impact the informed consent process serving as a recent benchmark. In particular, patients undergoing a minor amputation should be made aware of the magnitude of risk to life, likely need for revision and the risk of revision to major amputation. These risks ought to be thought of less as theoretical risks (which patients are known to be poor at interpreting) and more realistically as the natural history of their underlying disease process.
Limitations of study
This study was retrospective in nature so no causative relationships between intervention and outcome can be asserted. Comorbidities including diabetes status, measures of PAD severity, smoking status and urgency of amputation were not captured during data collection, meaning that outcomes are not risk-adjusted, limiting the degree of translatability to other centres. Similarly, previous and contemporaneous limb salvage procedures such as angioplasty, stenting and bypass were not captured, which may confound the mortality and revision rates after amputation.
Through-knee amputations (TKA) were not performed at this centre during the study period but are increasingly performed at centres throughout the UK. As such, these outcomes may not be generalisable to patients undergoing TKA, with further work needed to compare outcomes, particularly rehabilitation outcomes between TKA, BKA and AKA.
The outcomes reported here are clinician defined, technical and are largely abstract from the patient’s personal disease experience. Of note, the quality of life and communication outcomes specified in the core outcome set by Ambler et al17 were not able to be thoroughly assessed in this study. Limited inferences regarding a quality of life benefit can be made from the reported rehabilitation outcomes. However, it is likely that exploration of the performance of activities of daily living, social reintegration, ongoing care requirements and longer-term ambulation would be valuable in evaluating and planning an amputation service.
Conclusions
Major amputation and, to a lesser extent, minor amputation are last resort procedures performed when a limb cannot be salvaged. As such, they are associated with a high short- and medium-term mortality and carry high revision rates. These contemporary statistics should form part of the informed consent discussion when performed in preference to a conservative or palliative management strategy. Further research into patient-reported outcomes and holistic rehabilitation outcomes will be necessary to provide personalised care, optimise patient pathways and facilitate a real-world patient quality of life benefit.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(2):84-90
Publication date:
February 28, 2024
Author Affiliations:
1. Clinical Research Fellow, Academic Section of Vascular Surgery, Department of Surgery and Cancer, Imperial College London, London, UK
2. Final Year Medical Student, School of Clinical Medicine, University of Cambridge, Cambridge, UK
3. Consultant Vascular Surgeon, Cambridge Vascular Unit, Addenbrooke’s Hospital, Cambridge University Hospital NHS Foundation Trust, Cambridge, UK
4. Honorary Senior Clinical Lecturer, Section of Vascular Surgery, Department of Surgery and Cancer, Imperial College London, UK
Corresponding author:
Henry Bergman
Academic Section of Vascular Surgery, Department of Surgery and Cancer, Imperial College London, Charing Cross Hospital, Fulham Palace Road, London, W6 8RF, UK
Email: henry.bergman@ imperial.ac.uk











