PROTOCOL
Motivating Physical Activity with a Walking Exercise Behaviour Intervention and Pain Management Remotely in Intermittent Claudication (MAvERIC): protocol for a randomised controlled feasibility trial
Carroll SP,1 Gray SR,2 Wood L,3 Bearne L,4 Seenan C1
Plain English Summary
Why we are undertaking this research: Peripheral arterial disease (PAD) occurs when the arteries in the legs narrow and harden. People with PAD have a lower quality of life and are at risk of heart attack and stroke. Research suggests that people with PAD should increase their walking as with advice given for other heart issues. Yet people with PAD receive less exercise and treatment than those with other heart problems despite the benefits to leg pain, walking function and health. For those with PAD, walking can be hard because it hurts. Our studies have found that a small pain-easing device can help people walk further. We also found that helping people know how to manage their PAD and setting exercise goals can increase walking and well-being. Since not all people can travel for these services, we are looking to see if a pain-easing device and online meetings with a physiotherapist can work.
What we aim to do: We will test if an online walking exercise behaviour programme and using a transcutaneous electrical nerve stimulation (TENS) device can help people with PAD be more active. This involves completing a walking programme at home with support from two video and two telephone sessions with a physiotherapist and using a TENS device to reduce any walking pain. We will check how these compare to usual care offered at this health board. Usual care consists of medication, lifestyle and walking advice or plan. Patients from the vascular units will be invited to join the study. If they are suitable they will be put into a group by chance either trying the new methods or usual care alone. A device will track how much walking each person does. They will also share their views through surveys and feedback. This will help to better the study and programme before being tested on a larger scale.
Abstract
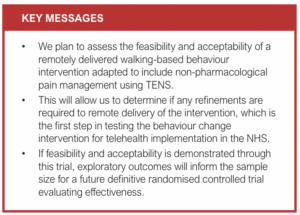
Background: Physical activity (PA) through walking exercise improves functional capacity and quality of life and provides secondary prevention benefits in individuals with peripheral arterial disease (PAD) and intermittent claudication (IC). However, there are many barriers to uptake and maintenance of PA in this population including pain and limited motivation. The aim of this study is to test the feasibility and acceptability of delivering a clinical trial to evaluate the effect of using a walking exercise behaviour change intervention, modified to include the use of a transcutaneous electrical nerve stimulation (TENS) device for non-invasive pain management, to increase walking-based PA in individuals with PAD and IC in comparison with usual care.
Methods: This is a randomised controlled analysis-blinded feasibility study with two parallel groups. We will recruit 48 adults with PAD and IC from NHS Lanarkshire vascular service. Inclusion criteria are: PAD (ankle brachial pressure index <0.90) and stable IC for >3 months, being able and willing to participate, and to provide informed consent. Participants will be randomly assigned 1:1 to intervention plus usual care or usual care alone. Usual care includes best medical therapy, information on PAD, walking advice or home exercise programme, and managing risk factors. The intervention consists of a home-based, walking exercise behaviour change intervention (MOSAIC), adapted for remote delivery, and includes non-pharmacological pain management through a TENS device. Feasibility and exploratory outcomes will be assessed at baseline, after 6 and 12 weeks of intervention, and at 6 and 12 months follow-up. The primary outcomes are trial process and intervention feasibility, as well as intervention acceptability measured using rates of participant recruitment and retention, intervention adherence, and the Theoretical framework of Acceptability questionnaire. Exploratory outcomes include daily PA and patient-reported outcomes including quality of life, pain self-efficacy and catastrophising, and walking impairment pain intensity and quality.
Conclusion: This trial will evaluate the feasibility and acceptability of a remotely delivered walking exercise behaviour change intervention adapted to include the use of a TENS device to improve PA in individuals with PAD and IC.
Trial Registration Number: ClinicalTrials.gov Identifier: NCT06114732
Introduction
Peripheral arterial disease (PAD) affects approximately one in five people aged >60 years.1,2 In addition, 40–75% of these people experience intermittent claudication (IC), a chronic manifestation of PAD which commonly presents as limb pain and reduced exercise tolerance.3,4 People with PAD and IC experience disability and impaired quality of life due to reduced physical capacity compared with age- and sex-matched controls.5,6 Overall, this causes a significant burden to individuals with the disease, as well as wider economic costs and service costs to the National Health Service (NHS) in terms of loss of healthy life-years and treatment.7-10
Improving physical activity (PA) is particularly important in individuals with IC as lower PA levels have been recognised as a strong predictor of increased morbidity and mortality in this population.11,12 National Institute for Health and Care Excellence (NICE) guidance recommends Supervised Exercise Therapy (SET) as a primary treatment for IC with established efficacy in increasing PA, walking distance and improving quality of life, contributing to secondary prevention of major adverse cardiovascular events (MACE).4,13 However, guideline standard SET is available in only one in four vascular services in the UK.14 Moreover, where SET is available, uptake and adherence are limited due to reduced mobility from limb pain or low walking capacity, and this may be further restricted with variation in local service provision within a hub-and-spoke healthcare model.15 This reflects a severe inequality in healthcare to the 17–30% of people in the UK who reside in rural communities and those with increased level of disability.16,17 Therefore, in light of the prevalence of PAD, the constraints of healthcare resources and variation in provision of services nationally, there is an urgent need for the development of easily accessible and scalable alternatives to conventional SET.
Due to the extrinsic and intrinsic barriers to participation in PA in people with IC, it is vital that, as well as navigating the limitations of SET, the interventions also improve health literacy, illness perception and self-efficacy.18,19 There is some evidence that the self-management of IC using behaviour change principles may be effective in addressing issues with self-efficacy, health literacy and uptake of walking exercise.20 Recently, following participation in the walking-based behaviour intervention Motivating Structured Walking Activity in People with Intermittent Claudication (MOSAIC),21 people with PAD (n=190) were able to walk further at 3-month follow-up and reported improvements in other functional and quality of life outcomes.22 The intervention included two in-person and two telephone sessions delivered by physiotherapists over 3 months. MOSAIC has the potential to be delivered remotely to ensure that people with PAD can continue to take part in the intervention even if they live within rural communities with limited transport links or if SET is not provided locally. With the increasing access to the internet, even in low-income groups, the practicality of remote delivery of interventions on a large scale may be possible.23
While it is promising that novel accessible and scalable alternatives may exist to SET, for people with IC to gain the benefits of secondary prevention through PA, exercising beyond the point when pain occurs is recommended.24 This represents another barrier to engagement in PA.25,26 Despite this, a recent systematic review27 found that pain management as a route to facilitate exercise and PA has rarely been explored. Recent work has suggested that the use of transcutaneous electrical nerve stimulation (TENS) applied to the lower limb during walking on a treadmill can improve absolute claudication distance above placebo.28 Moreover, the home use of TENS may contribute to improvement in PA in individuals with IC.28,29
By managing limb pain and facilitating walking exercise behaviour change, MOSAIC adapted to include TENS may have the potential to help increase walking-based PA and walking capacity in people with IC.22,28 However, the combination of a remotely delivered walking exercise behaviour change intervention that includes TENS has not previously been evaluated. Prior to assessing the clinical and cost effectiveness of the intervention in a suitably powered randomised controlled trial (RCT), outcome data from which the sample size of a clinical trial could be estimated, the acceptability and feasibility of both trial processes and procedures as well as remote delivery of MOSAIC with a TENS device must be assessed and refined if appropriate.30 Therefore, the aim of this randomised controlled feasibility trial is to determine the feasibility and acceptability of conducting a trial investigating the effectiveness of a remote walking exercise behaviour change intervention (MOSAIC) adapted to include TENS in people with PAD compared with usual care.
Methods
Research objectives
1. Assess the feasibility of conducting an RCT of a remotely delivered walking exercise behaviour intervention modified to include TENS in people with IC.
2. Measure participant recruitment, retention and attrition.
3. Measure outcome completion, attendance at appointments, total accelerometer wear time and usage of TENS device.
4. Measure protocol adherence and safety.
5. Conduct semi-structured interviews with intervention completers to assess acceptability and lived experience of the trial processes and intervention.
6. Explore changes in physical activity and quality of life outcomes from which the sample size of a definitive trial could be estimated.
7. Explore participants’ experiences and perceptions of the interventions and trial procedures.
Study design
This is an assessor blinded randomised feasibility trial. Forty-eight adults with PAD and IC will be randomised to one of two arms: remote MOSAIC adapted to include TENS plus usual care or usual care alone (Figure 1). The setting in which the trial processes and intervention consultations will take place is within the home or other convenient private area suitable for telehealth consultation. This protocol follows the guidelines recommended by the Standard Protocol Items for Interventional Trials and recommended CONSORT extension to randomised feasibility trials (see Appendix 1 and 2 online at www.jvsgbi.com).

Inclusion and exclusion criteria
Patients within the NHS Lanarkshire Vascular Outpatient Service with either a clinical diagnosis of PAD by a vascular specialist, an ankle brachial pressure index (ABPI) <0.9 at rest or evidence of PAD on Doppler ultrasound or angiography will be invited to participate in the trial. Inclusion and exclusion criteria are listed in Figure 1. Symptomatic stable IC (stage II Fontaine Classification) will be determined by a report of symptoms on the San Diego Claudication Questionnaire (SDCQ)31 and clinical diagnosis by a vascular specialist including ABPI of <0.9. Participants with critical limb ischaemia (rest pain, ulceration, gangrene) and those in whom lower limb revascularisation is planned within the intervention period will be excluded. Patients who are unable to give informed consent, are participating in another medically prescribed exercise intervention, are unable to walk due to co-existing medical morbidities or those with no internet or computer device for video consultations will be excluded.
Study procedures
Sampling and recruitment
Patients with PAD and IC within NHS Lanarkshire will be invited to take part in this study from February 2024 at the vascular outpatient service by the allied health professional or nurse undertaking the consultation. This is the primary method of recruitment; however, if the recruitment rate is <5% of the required sample after 2 months, a screening questionnaire will be used by a member of the vascular service when examining the clinic lists of the last 2 years to identify eligible participants attending the vascular outpatient claudication clinic. They will send by post an expression of interest letter along with a participant information sheet which contains a telephone contact number if the patient wishes to opt into the study.
A total sample size of 48 was calculated based on the proportions of uptake, attendance and compliance from the intervention arm.22,28 An overall sample size of 43 participants was calculated which was increased to 48 participants to allow for potential attrition.32
Randomisation
Participants will be block randomised in a 1:1 ratio to either MOSAIC + TENS or usual care. The randomisation will not be conducted by researchers involved in recruitment or outcome assessment. Allocations will be prepared using a random number generator and kept in sealed opaque envelopes prepared by a researcher who is independent of the study team. The envelopes will remain unopened until allocation by the Principal Investigator (PI) at the first contact following baseline data collection.
Control group
Participants will receive usual care and walking/exercise advice from the vascular and claudication service at NHS Lanarkshire. This will be a pragmatic control arm as individual treatment may vary between participants. Usual care follows standard clinical guidance and often involves offering information on PAD and changes in lifestyle (eg, quitting smoking, managing diet and weight), walking advice or home exercise programme, managing risk factors which includes adjusting lipids, using statin and antiplatelet treatments or medication to enhance leg symptoms (vasodilators such as naftidrofuryl oxalate).4 In NHS Lanarkshire people with PAD are usually diagnosed and treated in primary care within a network of Community Claudication Clinics, with onward referral to vascular outpatient clinics for further investigation and treatment as necessary.
Intervention group
The adapted walking exercise behaviour intervention (based on MOSAIC)21,22 comprises two 60 min consultations completed by video call (weeks 1 and 2) and two 20 min follow-up telephone calls (weeks 6 and 12). The content of each session is standardised and incorporates evidence-based behaviour change techniques to facilitate understanding and commitment to walking exercise. Sessions will be tailored based on participants’ knowledge, goals, symptoms and current walking using a motivational interviewing approach.33 The session is delivered by the PI who is educated in motivational interviewing techniques.
One week in advance of the first video consultation an interactive manual containing worksheets and a walking diary will be posted out as part of the modified walking exercise behavioural intervention. During the first video consultation the participants, in addition to using the MOSAIC materials in the consultation, will be offered a TENS device as an option to manage their leg pain during walking exercise and a pedometer to self-monitor their step count, using the motivational interviewing approach ‘elicit-provide-elicit’.33 If they opt to use the TENS device or pedometer it will be posted to their home address with an instruction booklet for the device. There will be an opportunity to query or troubleshoot TENS device usage at the next video consultation one week after the first video consultation. The intervention group will receive high-frequency TENS (120 Hz, 200 µs and a participant-determined intensity of ‘strong but comfortable’), as this was found in a proof-of-concept study to increase the distance walked in people with IC before reaching their pain tolerance and prolonged time to reach onset of pain (compared with low-frequency TENS).28
As part of the second video consultation, walking plans will be agreed collaboratively between the participant and the physiotherapist and include progressive individualised targets for walking frequency, intensity and duration to achieve at least the recommended walking guidance for IC (30–50 min of walking three times/week at an intensity that elicits pain within 3–5 min).24 Options to use the TENS device will be discussed and agreed alongside walking goals and plans in the second video consultation if the participant agrees to this. Walking plans, progress and goals will be reviewed at weeks 6 and 12 during 20-min telephone booster sessions.
Outcome measures
Feasibility and acceptability outcomes
The study recruitment rate will be recorded by logging reasons for non-eligibility and non-recruitment of eligible participants using the study screening log. Uptake and adherence to intervention sessions by participants will be measured by attendance at appointments, withdrawal from study, TENS usage (via in-built memory of the device and a self-reported TENS diary) and administering the Theoretical Framework of Acceptability questionnaire at the trial endpoint.34 In addition, a purposive sample of participants will be invited to attend a semi-structured interview regarding their lived experience of the trial and interventions. Adverse events will be monitored, recorded in a study log and followed up if required. Data will be collected by the PI at all time points.
Exploratory outcomes
The habitual PA of participants will be recorded by a trial axial accelerometer, the activPALTM, worn for 7 days and the following outcomes extrapolated from the accelerometery data: total daily steps, total duration of walking, total daily time spent sitting, and event-based claudication index (ECBI; the ratio of walking events to upright events participants undertake in a day).35 Three days or 72 hours of continuous wear of activPALTM data at each time point will be the minimum for including a participant’s activPALTM data in the exploratory analysis. Pain-related quality, intensity, self-efficacy and catastrophising will be assessed using patient-reported outcome measures (PROMs): the Short Form-McGill Pain Questionnaire (SF-MCQ)-2,36 a Visual Analogue Scale (VAS) of Intensity of Pain, Pain Self-Efficacy (PSEQ)37 and Pain Catastrophizing Scale (PCS).38 Likewise, quality of life will be assessed using PROMs: the Intermittent Claudication Questionnaire (ICQ)39 and the EQ-5D-3L. Data collection time points for each outcome are shown in Table 1. All outcome assessment devices and measures are returned by post so, to maintain blinded data analysis, materials will be assigned a unique code and any identifying information removed prior to data entry and analysis by a researcher outwith the study team.

Evaluation of intervention delivery fidelity
To assess fidelity to the intervention, all intervention sessions will be audio recorded with permission from the participant. A random sample of 10–20% of recorded sessions will be assessed by a member of the study team from the MOSAIC trial, to assess the extent that mandatory components of each session were delivered as intended. Segments of 20 min, chosen at random from the intervention sessions sampled, will undergo evaluation for the physiotherapist’s effectiveness in motivational interviewing using the Motivational Interviewing Treatment Integrity scale.40 This includes assessing relational proficiency on a Likert scale, where a score of 3.5 out of 5 suggests an acceptable level of interpersonal style and technical proficiency, and a score of 3 out of 5 indicates an adequate technique.
Trial schedule
Baseline assessment
Written informed consent will be recorded and baseline measurements will be conducted including questionnaires and fitting of the activPALTM monitor remotely over video call with the PI. These will be posted out to the participant with an information sheet and further instruction can be sought at the video call with the PI. Paper copies of the PROMs will be posted back using a pre-paid envelope at baseline, week 6 and week 12. These will be collected, anonymised and given a unique identifier by a member of the study team not delivering the intervention or conducting data analysis. Participants will also return the activPALTM after 1 week of wear via a pre-paid envelope. After this point, participants will be randomised to either intervention or usual care as described under study procedures.
Weeks 6 and 12 assessment
The second and third data collection points (6 and 12 weeks) will occur following a 20 min telephone ‘booster’ session and review of progress and goals for the intervention. This will be a repeat of the outcome assessment conducted at baseline; however, the Theoretical Framework of Acceptability questionnaire will only be administered at week 12 (intervention end point). The usual care group will only be contacted at 6 weeks and 12 weeks by the research team to post the questionnaires and video fitting of the activPALTM monitor.
Qualitative interviews and follow-up assessment
At the intervention end point a purposive sample of participants will be invited to an online semi-structured interview session, which will be implemented within 1–3 weeks after the end of the intervention. The setting in which the qualitative interviews will take place is within the home or other convenient private area. The follow-up outcome assessment will be at 6 and 12 months for all groups. This will be a repeat of the outcomes at the baseline assessment.
Data analysis
Analyses will follow the intention-to-treat principle. Secondary per protocol analyses will also be performed. To ensure blinded analysis by the PI, all outcome data received from participants will be sent to the Chief Investigator (CS) who will conceal the group allocation and a unique code in place of identifiable information (eg, participant name). This anonymised data will then be input into an electronic Excel spreadsheet and the Principal Investigator (SC) will conduct data analysis independently to remain blinded. All data will be summarised in accordance with the CONSORT guidelines.41 Descriptive statistics will be used to describe demographics and baseline characteristics of each outcome, as well as to compare the outcomes at each time point between and within groups.
Feasibility and acceptability analysis
To determine the feasibility of conducting an efficacy trial, descriptive statistics will be used to report the number and proportion of participants who meet the inclusion criteria, who consented to participating, and who dropped out during the trial. Feasibility of trial processes in the remote setting will be derived from a participant’s attendance at appointments, follow-up calls, rate of outcome measure completion, total accelerometer wear time and, if applicable, self-reported and internal memory recorded use of the TENS device.
Recordings from the semi-structured interviews will be transcribed verbatim and analysed using interpretive thematic analysis by the lead author.42 The researchers will provide written transcripts to the participants to check the accuracy of the transcription. Provisional themes will be discussed with the wider research team with reference to an audit trail, and processes refined if required to agree on and identify the final labeling of themes. In order to manage the data and undertake analysis, NVivo V20 (QSR International Pty Ltd) will be used.
Exploratory analysis
Between-group comparisons for walking outcome measures and group continuous measures will be summarized using mean and standard deviation, or median and interquartile range if the distribution is skewed. To compare different groups allocated to each intervention, an analysis of variance will be used, or a Kruskal–Wallis test if the data are non-parametric. The Theoretical Framework of Acceptability questionnaire scores will be compared between groups cross-sectionally at the intervention end point using a Mann–Whitney U test. Within-group comparisons longitudinally will be examined using a repeated measures analysis, or non-parametric equivalent if appropriate. Analysis will be blinded by a member outwith the study team anonymising the dataset.
Unblinding will be permitted in the event of a spontaneously reported adverse event or unintended effect of trial intervention that requires liaison with the participant’s medical care team. In this event, this will be logged on the trial adverse event form and the sponsor and local NHS Research and Development office informed. If appropriate, the participant will be removed from the trial.
Data management
Data will remain confidential and stored securely at Glasgow Caledonian University in accordance with the Data Protection Act and General Data Protection Regulation. Electronic data will be pseudo-anonymised and stored on a password-protected database on a secure device at Glasgow Caledonian University. Only named investigators will have access to the data. All paper documentation including signed informed consent forms will be kept in a secure locked filing cabinet at Glasgow Caledonian University. Data will be retained in accordance with the Good Clinical Practice guidelines or local regulations, whichever specifies a longer retention time.
Trial Management Group
The trial will be coordinated from Glasgow Caledonian University by the Trial Management Group. This will consist of the co-investigators, NHS Lanarkshire Claudication Steering Group chair, Service Manager, and a person with PAD as a patient and public involvement (PPI) representative. The role of the group is to monitor the conduct and progress of the trial, ensure that the protocol is adhered to and take appropriate action to safeguard participants and the quality of the trial itself. The group will meet every 3 months via video conference.
Study registration and ethical approval
The West of Scotland Research Ethics Committee provided approval for this study (Reference: 23/WS/0147) on 30 October 2023 and the study was subsequently registered on ClinicalTrials.gov (Identifier: NCT06114732). The research will be carried out following the principles of the Declaration of Helsinki. Those who qualify for inclusion will be asked to provide written informed consent before taking part in the study. Each participant will be reminded of their right to withdraw. Glasgow Caledonian University is the sponsor for this feasibility trial.
Discussion
People with PAD and IC face a loss of healthy life-years, as well as a heightened risk of MACEs, hospitalisation and mortality.1-5 Finding accessible, acceptable and scalable methods to support increasing walking-based PA for people with this condition is crucial, given the disease burden for individuals and their families and the economic demand on the NHS.7-10 The need for this is amplified when considering the significant barriers to walking that prevent uptake and adherence, both intrinsic (self-efficacy, knowledge of PA as beneficial and limb pain) and extrinsic (geography, accessibility to an exercise professional or service).25,26
Altogether, these findings emphasise the need for self-management interventions that are accessible and address both pain management and walking-related behaviour change. MAvERIC is a novel combination of a remotely delivered walking exercise behaviour change intervention (MOSAIC)22 adapted to include TENS28 for pain management. The intervention aims to address the barriers to physical activity in people with PAD and IC. This is the first step in testing the behaviour change and pain management intervention for telehealth implementation in the NHS. If feasibility and acceptability of trial processes and intervention are demonstrated in this study, an appropriately powered RCT will aim to test the effectiveness on walking-based PA in people with IC. Despite the novel approach due to the use of internet and of a smart device/computer in receiving the intervention, there may be some socioeconomic bias in the sample. Additionally, the exclusion of ABPI measurement with exercise testing may have reduced sensitivity of the recruitment strategy.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2024;3(3):147-154
Publication date:
May 16, 2024
Author Affiliations:
1. Department of Physiotherapy and Paramedicine, School of Health and Life Sciences, Glasgow Caledonian University, Glasgow, UK
2. School of Cardiovascular and Metabolic Health, College of Medical, Veterinary and Life Sciences, University of Glasgow, Glasgow, UK
3. Department of Biological and Biomedical Sciences, School of Health and Life Sciences, Glasgow Caledonian University, Glasgow, UK
4. Population Health Research Institute, St George’s, University of London, London, UK
Corresponding author:
Sean Paul Carroll
Department of Physiotherapy and Paramedicine, School of Health and Life Sciences, Glasgow Caledonian University, Glasgow, G4 0BA, UK
Email: [email protected].











