ORIGINAL RESEARCH
Research priorities for patients with peripheral arterial disease: a James Lind Alliance Priority Setting Partnership
Pymer S,1 Harwood AE,2 Long J,1 Chetter IC,1 Saratzis A,3 Coughlin P,4 on behalf of the Vascular Society of Great Britain and Ireland Peripheral Arterial Disease Special Interest Group James Lind Alliance Priority Setting Partnership
Plain English Summary
Why we undertook the work: Research funding is limited and highly competitive and funders and policy makers need to know where best to direct their funding. A priority setting process can help address this issue by asking patients and healthcare professionals what areas of research are important to them. This paper presents the results of this process for the area of peripheral arterial disease (PAD), also referred to as narrowed arteries to the legs.
What we did: We asked patients and healthcare professionals in two separate surveys to tell us what research they felt was important for vascular conditions. The responses were organised and sent back out to patients and healthcare professionals separately, to be scored in order of importance. Both sets of responses were then combined and discussed at a workshop where a final list of PAD research priorities was created based on perceived importance to patients, carers and healthcare professionals.
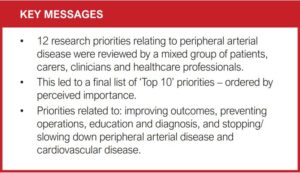
What we found: A total of 481 clinicians and 373 patients or carers proposed research priorities related to vascular conditions in general, which were amalgamated into a list of 12 priorities specifically about PAD. These were discussed at the workshop and ordered in terms of their importance. The top 10 priorities, which are given in full in this paper, related to: improving outcomes, preventing operations, education and diagnosis, and stopping/slowing down PAD and cardiovascular disease.
What this means: PAD research, which is important to both patients and healthcare professionals, can now be undertaken within these topics. Funding bodies and research teams should now focus their efforts into addressing the PAD top 10 priorities.
Abstract
Introduction: Peripheral arterial disease (PAD) is a common health problem associated with reduced mobility, functional capacity and quality of life. Significant research exists in the field of vascular surgery, but its relevance to the research priorities of patients/carers and clinicians/healthcare professionals is unknown. The aim of this process, conducted by the Vascular Society of Great Britain and Ireland with the James Lind Alliance (JLA), was to identify the key research priorities for PAD, from the perspective of patients/carers and clinicians/healthcare professionals.
Methods: A modified JLA Priority Setting Partnership was performed in three stages: (1) a clinician/healthcare professional-led Delphi process; (2) a patient/carer-led JLA process; and (3) amalgamation of patient/carer and clinician/healthcare professional-led results for a final round of JLA-led prioritisation. The clinician/healthcare professional Delphi process surveyed vascular clinicians/healthcare professionals, inviting them to submit important research priorities for vascular surgery. This generated a list of priorities which were redistributed for interim scoring. The priorities fitted into nine specific Special Interest Groups (SIGs), one being PAD. This was followed by a patient/carer Delphi process (in association with the JLA) using a similar two-stage process. Finally, research priorities formed by these two processes were amalgamated to produce a refined list relevant to PAD. The PAD SIG then held a final JLA consensus workshop which was attended by patients/carers and clinicians/healthcare professionals, where a nominal group technique was used to produce a ranked top 10 list of research priorities specific to PAD.
Results: In the clinician/healthcare professional Delphi process, 481 clinicians/healthcare professionals submitted 1,231 research priorities related to vascular conditions. Two hundred and six PAD-specific priorities were amalgamated into 17 priorities which were recirculated for scoring according to perceived importance. For patients/carers, 582 research priorities were submitted by 373 individuals, and 114 PAD specific priorities were amalgamated into 9. These were recirculated for scoring according to perceived importance. After amalgamation of both sets of priorities, 12 remained, which were discussed at the final consensus meeting, resulting in a final ranked list of 10 PAD-specific research priorities. Research priority themes included improving outcomes, maximising non-invasive therapy, education and diagnosis, and stopping/slowing down PAD and cardiovascular disease progression.
Conclusions: We have identified the top 10 PAD-related research priorities from the perspective of patients/carers and clinicians/healthcare professionals. This should provide guidance for researchers, clinicians, healthcare professionals and funders to ensure that proposed PAD research is addressing priorities that are considered important to all parties.
Introduction
Peripheral arterial disease (PAD) is an atherosclerotic process whereby the arteries supplying the lower limbs become narrowed or occluded. PAD is an increasingly common disease, estimated to affect 237 million people, with an increase of 45% between 2000 and 2015.1,2 The PAD spectrum is wide and ranges from asymptomatic, whereby the patient is often unaware they have the disease, to critical limb threatening ischaemia (CLTI), which is associated with a high major amputation rate and mortality risk.3,4 Intermittent claudication (IC), an ischaemic ambulatory muscle pain that is relieved by rest, falls between these being associated with more moderate ischaemia. IC is the most common symptomatic manifestation of PAD and is often stable with regard to leg symptoms, although it is associated with increased cardiovascular morbidity and mortality.5,6 IC negatively impacts on balance, ambulation, functional capacity, activities of daily living and quality of life.7-10 Patients with CLTI suffer more debilitating symptoms including intractable rest pain, trophic skin changes, gangrene, non-healing ulcers or any combination thereof.6
Suggested treatment algorithms vary depending on clinical presentation. All patients require optimisation of cardiovascular risk to reduce the recognised risk of cardiovascular events and death.11,12 First-line treatment to improve the limb symptoms of IC is enrolment in a supervised exercise programme (SEP).12 More invasive treatment for IC should only be instituted if a SEP has failed to improve symptoms. Patients with CLTI require revascularisation if possible to reduce the risk of major limb amputation.12 Primary revascularisation is possible in only 50% of patients with CLTI, with the remainder undergoing primary amputation (25%) or medical management only (25%).6 Many elements of PAD management still lack high level supportive evidence and effective implementation. For example, it is recognised that clinician and patient adherence with cardiovascular risk reduction therapies is suboptimal, yet we do not understand fully how to improve this.13 The provision of, and engagement with, a SEP is still poor in the UK despite evidence to support its benefits.14,15 For patients with CLTI, it is still not known which level of amputation maximises functional recovery when a below-knee amputation is not possible.6,16 These examples demonstrate clearly an unmet need for further high-quality research driven by the priorities of patients, carers and clinicians/healthcare professionals to improve the management of patients with PAD. Such information is also key in informing funding bodies, commissioners and policy makers about the research priorities for vascular surgery. The James Lind Alliance (JLA; https://www.jla.nihr.ac.uk/) uses a well validated Priority Setting Partnership (PSP).17 They facilitate PSPs to ‘bring patient, carer and clinician groups together on an equal footing, identify evidence uncertainties which are important to these groups, work with these groups to jointly prioritise the uncertainties and produce a top 10 list of jointly agreed uncertainties as research questions to be presented to funders’.17 The vascular research collaborative and the vascular condition PSP were founded in 2016 and 2019, respectively, with the aim of developing a national research strategy for the vascular specialty and identifying the research priorities for each sub-specialty. We detail how we undertook a JLA PSP to ascertain and clarify the opinions of clinicians/healthcare professionals and patients/carers to identify the most important clinical research priorities for PAD that require future investigation.
Methods
A detailed methodology of the process has been provided previously.18 We provide a summary below. A visual summary is also presented in Figure 1. We used a modified JLA PSP methodology to identify the research priorities for vascular conditions. The JLA PSP states that a survey should be distributed to patients/carers and clinicians/healthcare professionals who can make suggestions for research uncertainties. These data are then processed to remove out-of-scope submissions, categorise eligible submissions, form indicative priorities and verify the uncertainties (ie, existing research does not already answer this uncertainty).17 The indicative list of priorities is then shortened via an interim prioritisation. This involves redistributing the indicative list of priorities to patients/carers and clinicians/healthcare professionals for scoring according to perceived importance, with the top priorities taken forward to the
final workshop. This final workshop involves whole and small group discussions to produce a ranked list of research priorities, with the aim of delivering a ‘top 10’.
In our case, due to initial resource limitation, the first two stages (survey completion and priority scoring) took place separately for clinicians/healthcare professionals and patients/carers, with oversight from a National Steering Committee.18 The clinician/ healthcare professionals survey was completed first, followed by the patient/carer survey two years later, in association with the JLA. The data from the first round of the clinician/healthcare professionals survey was analysed by a working subgroup of the steering committee and a refined list of summarised priorities was redistributed for interim scoring. This process also led to the creation of nine Special Interest Groups (SIGs) that were organised into different vascular specialty areas, one being PAD. This was followed by a JLA PSP to gather research priorities from a patient/carer perspective via a separate survey. The data from this survey were analysed by the respective SIGs and a summarised list of research priorities was redistributed to patients/carers for interim scoring. Clinician/healthcare professional-led priority setting process The clinician/healthcare professional-led PSP was completed in 2018 and published in 2020.19 Out of 45 potential vascular themes, nine key areas were identified, leading to the creation of nine SIGs in the following areas: Access, Amputation, Aortic, PAD, Carotid, Diabetic foot, Venous, Wounds and a general category for Vascular Service Organisation. This clinician/healthcare professional-led PSP was delivered via a modified Delphi approach. It involved two rounds of online surveys involving members of the Vascular Society of Great Britain and Ireland, Society of Vascular Nurses, Society for Vascular Technology and the Rouleaux Club for vascular surgical trainees. During round 1, participants were invited to submit the research priorities they felt were most pertinent to vascular surgery. These were then collated and categorised into pathological topics and research themes by the steering group. Priorities that addressed the same or a closely similar topic were amalgamated. In round 2, these summary priorities were then recirculated for interim scoring on a scale of 1–10 (1 being the least important, 10 being the most important).19

Patient/carer-led priority setting process
The vascular PSP, in association with the JLA, undertook a consultation with patients and carers to gather their vascular research priorities. The consultation in the form of a survey was open for six months (from September 2019 to March 2020). Patients and carers were approached and completed the survey either online or by paper, with patients being identified through outpatient clinics or from PAD focus groups. In addition, SIG members, UK vascular units, charities and patient groups were contacted to help promote the survey. PAD-specific priorities were identified, and similar or duplicate priorities were amalgamated. Priorities were edited by SIG chairs, with input from patient representatives, and those considered out of scope were excluded. This editing was necessary to ensure the refined list of priorities was easy to understand with no overlap and minimal uncertainty. The rest of the SIG team ratified these edits. This list of PAD priorities was recirculated between November 2020 and February 2021 for scoring using a Likert scale (scores ranging from 1 = Not at all important to 5 = Extremely important). This process took place either online or via paper format.
Final consensus workshop
Prior to the final workshop, priorities derived from both the clinician/healthcare professional and patient/carer surveys were reviewed by the PAD SIG and similar or duplicate priorities were merged. The language used in the priorities was reviewed to ensure it was appropriate and understandable for patients. This generated a final research priority list which was again ratified by the PAD SIG. The final consensus workshop for PAD was conducted virtually on 14 May 2021 using the Zoom platform. All attendees (including clinicians, healthcare professionals, patients and carers) were recruited via direct contact or were approached if they expressed an interest during the initial prioritisation process. Communication prior to, during and following the workshop was led by a JLA coordinator and involved prior circulation of the research priorities (in no particular order) and details of the workshop. Prior to the workshop, each attendee received the list of 12 research priorities and were asked to rank them in order of importance from 1 (most important) to 12 (least important). The workshop was led by three advisers who were skilled in the JLA process and leading such workshops. The workshop used a nominal group technique to create the final ranked top 10 research priorities from the original combined list of 12. Following an initial welcome and introduction to the workshop, the attendees were split into three breakout rooms which consisted of a mix of patients, carers, clinicians and healthcare professionals. The importance of the research priorities was discussed in each group and each member presented their top three and bottom three priorities, outlining underpinning reasons. The group together then ranked the priorities via consensus (from 1 to 12). The priority order was then collected from each group to generate an initial ranked list (based on geometric and arithmetic scoring). This initial ranking was then presented to the overall group. The process was then repeated with the attendees allocated to different breakout groups to discuss the new ranking order. The attendees were then given another opportunity to reorder the priorities again via consensus if it was felt necessary. The results of the final rankings were again collated, creating a final hierarchical list of research priorities based on the same scoring methods. The final top 10 list of research priorities was then presented to all attendees in the closing session. Members of the PAD SIG were present as observers and provided support if required (eg, if a patient needed emotional support), but they were not directly involved in the priority setting and had no influence over the final agreed list of priorities. In line with JLA guidance, they were muted with their camera off.
Results
Results from the clinician/healthcare professional-led research priority identification
A total of 1,231 research priorities were put forward by 481 clinician/healthcare professionals which, when removing duplicates, resulted in a total of 206 PAD-specific priorities. These were refined into a list of 17 summary priorities which were redistributed for scoring. The final list of clinician/healthcare professional priorities and their ranked mean scores is shown in Table 1.
Patient/carer-led research priority identification
A total of 582 research priorities were put forward by 373 patients/carers, with 114 priorities specifically pertaining to PAD. These were refined into a list of nine summary priorities, which were redistributed for scoring in terms of importance. Two hundred and seventy three patients/carers engaged with this phase of the survey and the final list of priorities, and their ranked mean scores is shown in Table 2.
Final prioritisation workshop
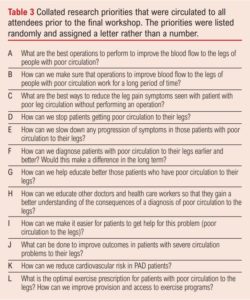
The final workshop was facilitated by four members of the JLA team and was attended by six patients/carers, 10 clinicians/healthcare professionals (consisting of consultant vascular surgeons, specialist vascular nurses, specialist surgical trainees and clinical exercise physiologists) and an additional two observers. The prioritisation process resulted in a ranked list of research priorities, ordered 1–12 by the attendees, from the initial pre-circulated list (ordered A–L to avoid bias; Table 3). This created the final ranked top 10 list of research priorities, being those that were ranked 1–10 (Table 4). During the final discussion it was confirmed by all participants that the top 10 list was a fair, accurate and comprehensive reflection of the discussions and viewpoints that were apparent in the individual breakout rooms and the order was therefore a reflection of the consensus. Results from the participant feedback indicated that 90% agreed or strongly agreed that the process for determining the top 10 priorities was robust and fair.
Two research priorities were ranked as 11th (“How can we make sure that operations to improve blood flow to the legs of people with poor circulation work for a long period of time?”) and 12th (“What are the best operations to perform to improve the blood flow to the legs of people with poor circulation?”). Both these priorities are related to performing operations for the treatment of PAD. The low ranking of these priorities was because it was felt that the top-rated priority “What can be done to improve outcomes in patients with severe circulation problems to their legs?” was more holistic and encompassed these two priorities, given that those with severe circulation problems often require surgical intervention.


Discussion
Using a modified JLA methodology, we have identified the key research priorities for PAD from the perspective of both patients/carers and clinicians/healthcare professionals, which should inform future research (Table 4). This focus on key research priorities will deliver patient relevant studies and will go some way to reducing research waste.20
The number 1 research priority was “What can be done to improve outcomes in patients with severe circulation problems to their legs?”. This is most likely to pertain to those patients with CLTI, which forms most of the clinical workload. The outcomes for patients with CLTI are still suboptimal, with data suggesting that only 50% are candidates for surgical revascularisation, whilst a quarter receive medical management only and the remaining quarter require primary amputation.6 Further, the 5-year mortality rate is >30%, which is worse than some cancers.21 The group agreed that this priority incorporated both the invasive and non-invasive management of those with CLTI, meaning it also encompassed the priorities ranked 11th and 12th. The importance of this research priority is also recognised by the most recent national Get It Right First Time (GIRFT) report and the Vascular Society of Great Britain and Ireland PAD quality improvement framework.22,23
The second most important research priority was “What is the optimal exercise prescription for patients with poor circulation to the legs?”. Exercise therapy is recommended for all patients with IC as the first-line treatment.12 This should ideally be delivered in the form of a SEP, which is more effective than unmonitored home-based programmes and exercise advice alone.24,25 SEPs have been recommended as first-line treatment for patients with IC in the UK since 2012,26 yet access to such programmes is limited and service delivery has not improved in 10 years.15,27 For those who do have a programme, there is still a lack of consensus on the optimal exercise prescription or the value of differing exercise regimes. Finally, the development of technology including wearables and the use of apps alongside the rapid uptake of virtual meeting platforms due to COVID-19 opens potential new methods of delivering such exercise programmes. Despite the existing literature considering exercise for patients with IC, there is a clear need for patients and healthcare professionals to work together to identify further aspects, including the optimal exercise prescription.
The third highest priority was “How can we diagnose patients with poor circulation to their legs earlier and better?”. Patients present at the workshop described a frustration at the length of time it took to receive the formal diagnosis of PAD, with some citing multiple trips to their general practitioner and/or other specialties before receiving the correct diagnosis and management. Frustration due to multifactorial delays in diagnosis has been reported previously.28 First, patients may incorrectly assume that exertional pain is a normal part of the ageing process and may delay seeking medical help.28 When medical help is sought, it may take significant time and effort to receive the correct diagnosis.28 Therefore, research that aims to reduce the time to diagnosis is vital, and this may link to priorities 4 and 5 which relate to patient and clinician education about PAD, and priority 6 which relates to making it easier for patients to get help.
The final four top priorities were related to reducing or slowing down the progression of symptoms without an operation and reducing cardiovascular risk or stopping people from getting PAD. These are all important priorities. With regard to symptoms, IC is associated with reduced balance, functional capacity and quality of life, meaning that an improvement in symptoms would likely result in an improvement in these factors.7-9 Also, people with PAD have an up to 15-fold increased risk of mortality, usually of cardiovascular origin, when compared with those without PAD.11 As such, research that looks at stopping people from getting PAD or reducing their cardiovascular risk is vital to address this.
Strengths and limitations
This study used a well-established process through a recognised organisation – namely, the JLA – to identify the research priorities for PAD from the UK perspective of both patients/carers and clinicians/healthcare professionals. The process was systematic and transparent, included a variety of key stakeholders and ensured active contribution from all parties. This was evidenced in the feedback from participants, which stated that the process was robust and fair and that they were all largely happy with the final prioritised list. However, there are some limitations to consider. First, the nature of data collection (survey) meant that there was a potential for responder bias, meaning the responses provided may not be reflective of the thoughts of all patients with PAD and the clinicians/healthcare professionals involved in their care. We did, however, attempt to minimise this bias. We were able to include patients from a range of geographical locations as well as different socioeconomic and health literacy backgrounds by offering both paper and electronic versions of the survey. We also included a range of clinicians/healthcare professionals, all of whom will interact differently with patients, to ensure varied responses. The PSP was also conducted using a slightly modified approach to that recommended by the JLA by conducting separate initial prioritisation rounds for patients/carers and clinicians/healthcare professionals. It is possible that the top 10 may have differed had the clinician/healthcare professional and patient/carer research priorities been analysed, summarised and ranked by all participants together at the same time. Despite this, the results of the final prioritisation workshop and the subsequent top 10 research priorities were clearly of importance to both groups.
Implications for future research
Identifying the most important PAD research priorities for both patients/carers and clinicians/healthcare professionals is vital for guiding research in this field in both the immediate and long term. These priorities will aid research teams and funders to ensure that the research being designed, funded and undertaken is of upmost importance. While this process has focused on themes, it is incumbent on researchers to determine and develop research projects to address these priorities.
The PAD SIG aims to develop an expert national group of researchers and clinicians/healthcare professionals supported by professional bodies, making it likely that the group will play a key part in providing solutions to these research priorities.
Conclusion
By undertaking a JLA PSP, the PAD SIG has been able to identify the top 10 research priorities from the perspective of patients/ carers and clinicians/healthcare professionals, which should shape the research agenda in this field in the immediate and long term.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2022;1(2):23-29
Publication date:
February 11, 2022
Author Affiliations:
1. Academic Vascular Surgical Unit, Hull York Medical School, Hull, UK.
2. Centre for Sport, Exercise and Life Sciences, Institute of Health and Wellbeing, Coventry University, Coventry, UK.
3. NIHR Leicester Biomedical Research Centre, University of Leicester, Leicester, UK.
4. Leeds Vascular Institute, Leeds, UK











