ORIGINAL RESEARCH
Surgical and rehabilitation outcomes of patients undergoing through knee amputation compared with above knee amputation
Gordon H,1,2 Hebenton J,3 Davie-Smith F,3 Twiddy M,4 Smith GE,1,2 Carradice D1,2
Plain English Summary
Why we undertook the work: Each year in the UK, more than 5,000 people need to have their leg surgically removed (amputated). A leg amputation can have an enormous impact on a person’s physical and emotional well-being. It is important that we research ways to minimise this impact. We know that people who have their leg amputated below the knee find physical and emotional recovery easier than people who have their leg amputated above the knee, but we do not know how amputation through the knee compares with amputation above the knee.
What we did: We used a database that holds information about amputations performed in Scotland between 2007 and 2017 and compared how people having above knee amputation and through knee amputation recovered after their surgery. We looked at how many amputations were performed above the knee and through the knee, how old the people were having an amputation, and what health conditions these people had. We looked to see if there was any difference between the two types of amputation including how long they stayed in hospital after surgery, how well their wound healed, if they were fitted for an artificial leg, and how well they could walk with their artificial leg.
What we found: Of the 4,197 amputation operations we looked at, over 90% were above the knee and less than 4% were through the knee, which means through the knee amputation is rarely performed in Scotland. On average, the people who had through knee amputation were a similar age to those who had above knee amputation, but a larger proportion of people in the through knee amputation group had diabetes or were obese. People who had a through knee amputation were more likely to need a second surgery because of problems with their surgical wound, but this did not mean that they needed to spend more time in hospital compared with people who had above knee amputation. The proportion of people who walked with an artificial leg was similar between the two types of amputation. Patients from centres performing larger numbers of through knee amputation were less likely to need a second operation but were also less likely to have an artificial leg fitted.
What this means: Hospitals in Scotland that perform relatively large numbers of through knee amputation have better results in terms of wound healing than hospitals that perform very small numbers. Through knee amputation is possibly preferred over above knee amputation in these same hospitals for patients who are unlikely to walk with an artificial leg. However, overall, people with through knee amputation were just as likely to walk with an artificial leg as those with above knee amputation, which could indicate that walking is easier with a through knee amputation. Other functional movements such as moving from bed to chair and maintaining balance when sitting in a chair are just as important as walking after amputation and should be investigated further for this patient group. As the numbers of through knee amputation in this study were much smaller than the numbers of above knee amputation, these conclusions should be investigated further with a larger group of patients.
Abstract
Background: Through knee amputation (TKA) may offer benefits over above knee amputation (AKA) in patients unsuitable for below knee amputation. This retrospective analysis compared surgical and rehabilitation outcomes post TKA and AKA.
Methods: All TKA and AKA procedures recorded in the Scottish Physiotherapy Amputee Research Group dataset from January 2007 to December 2017 were included for analysis. All aetiologies, re-amputations and bilateral procedures were included. Demographic information, surgical outcomes (ie, further surgery, survival, and length of stay) and rehabilitation outcomes (ie, limb fitting, early rehabilitation, and mobility scores) were compared using descriptive and inferential statistics, including Kaplan–Meier, log-rank statistics and multivariate logistic regression.
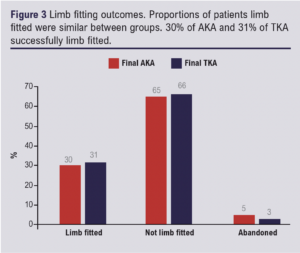
Results: In total, 4,197 procedures were included for analysis (3,471 initial AKA, 146 initial TKA, 580 initial below-knee or other level). Survival (p=0.809) and length of stay (p=0.696) were similar between groups, but TKA had significantly higher rates of further surgery (p<0.001). Multivariable analysis showed that patients who undergo TKA at centres which perform small numbers of TKA are significantly more likely to need further surgery (p=0.048). A significantly larger proportion of these patients had a limb fitted (25%) compared with only 12% of those from centres performing larger numbers of TKA (p=0.041). Overall, 31% (n=23) of those with TKA and 30% (n=725) of those with AKA had a limb fitted (p=0.854). All other rehabilitation outcomes were similar between groups.
Conclusion: High volume centres have better surgical outcomes but appear to select patients not likely to limb fit. Despite this, similar proportions of patients did subsequently limb fit between groups, which may suggest superior rehabilitation potential for TKA compared with AKA, although the numbers performed in Scotland are very small. Prospective randomised studies are urgently needed to inform clinical practice.
Introduction
Every year more than 5,000 patients undergo a major lower limb amputation in the UK.1-3 Major lower limb amputation is a pivotal life-changing event which can result in significant physical and psychological impacts, depending on the person’s functional ability pre-amputation, the cause of their amputation, their co-morbidities and the level of amputation.4,5
Below knee amputation (BKA) offers the greatest chance of using a prosthesis and accounts for over 50% of all major lower limb amputations performed in the UK each year.1,3,6 When a BKA is not viable, above knee amputation (AKA) is routinely performed.1,3,6 The removal of the knee joint, loss of the majority of the muscular insertions of the thigh, means that people with AKA face considerable challenges to achieve mobility with a prosthesis.7,8 However, AKA allows for proportional prosthetic knee centres, and recent advancements in prosthetic technology such as micro-processor knees have improved mobility outcomes post AKA.9,10
Through knee amputation (TKA) is an infrequently used alternative to AKA and represents less than 4% of amputations,1,3,6 despite recommendations for its use in guidelines.11,12 The long, end weight-bearing residuum offers several theoretical advantages over AKA for the prosthetic and non-prosthetic user. The shape of the residuum allows for a more comfortable prosthesis and a superior method for attaching the prosthesis to the residuum than with AKA. However, healing complications following TKA are often considered too high, even though they have previously been reported to be similar to BKA.13,14 Previous studies investigating outcomes of TKA have been limited by small and homogenous samples.15-18 Often, rehabilitation outcomes have been overlooked and only the surgical outcomes investigated.14,19,20 Comparing TKA to AKA was ranked as an important research priority in the James Lind Alliance priority research setting project.21
The aim of this study was to compare both surgical and rehabilitation outcomes for TKA and AKA.
Methods
Materials
This retrospective comparative cohort analysis examined data held in the Scottish Physiotherapy Amputee Research Group (SPARG) database for all patients who underwent TKA and AKA between 1 January 2007 and 31 December 2017. SPARG complete a national audit of anonymised data on every major lower limb amputation performed in Scotland. Collected data include demographic information such as age, sex, co-comorbidities, the centre that performed the amputation, aetiology, need for further surgery and inpatient length of stay. Rehabilitation data comprise limb fitting outcomes: time to cast; time to fit and delivery; time to start compression therapy; type of compression therapy; time to commence early walking aid; type of early walking aid; falls; change in mobility scores; and time to complete prosthetic rehabilitation. Co-morbidities are reported and measured using the functional co-morbidities index (FCI),22 which includes only co-morbidities that impact on function, with each morbidity scoring 1 point and 18 is the highest possible score. Pre- and post-amputation mobility scores are calculated using the Locomotor Capabilities Index-5 (LCI-5).23 The LCI-5 is a self-reporting tool which measures perceived ability to complete activities. All data were entered locally onto the SPARG web-based database and data forms are 97.8% complete in every respect.6
Patients
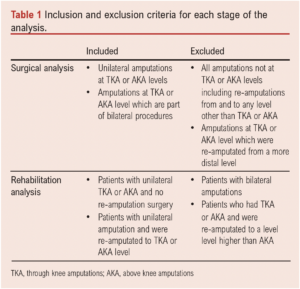
We excluded patients with BKA and through hip amputations; however, patients revised to TKA or AKA from BKA and those who had TKA or AKA and were revised to hip or pelvic levels were included. Amputations of all causes were included as were patients with bilateral amputations, whether both amputations were within the same episode, or if they already had an amputation and this episode recorded their second amputation. All types of TKA, including Gritti–Stokes, were included. Each amputation was considered as a unit of analysis for surgical outcomes. Patients with bilateral amputations were excluded from analysis of rehabilitation outcomes, where the patient was used as the unit of analysis. Exclusion and inclusion criteria for each stage of the analysis are shown in Table 1.
Statistical analysis
Data analysis was performed using SPSS Version 25 (IBM Corp, Armonk, New York, USA). Statistical significance was set at p<0.05 for all analyses. Descriptive statistics and surgical outcomes are presented in comparative groups of ‘initial AKA’ or ‘initial TKA’, meaning all amputations at that initial level including bilateral procedures.
Rehabilitation outcomes were analysed only in unilateral patient episodes due to complexity of rehabilitation in patients with bilateral amputation. The comparative groups are ‘final uni AKA’ or ‘final uni TKA’, meaning all patients who left the hospital with a unilateral amputation at that level.
Continuous variables are expressed as mean±standard deviation (SD). All continuous data were tested for normality. If normal, hypothesis testing was with the Student’s t-test. Median and interquartile range were used for non-normally distributed data and hypothesis testing used the Mann–Whitney U test. Chi-squared tests were used for cohorts with categorical variables. Fisher’s exact test was used for variables with small sample sizes. Survival analyses and hazard analyses for further surgery to the amputated limb were assessed by Kaplan–Meier curves and log-rank statistics. Multivariate logistic regression analysis was used to identify risk factors for further surgery and mortality.
Anonymised data are entered onto the secure SPARG database by a member of the patient’s care team. Only routine clinical data are recorded for the purpose of auditing services, supporting health surveillance and clinical decision-making. No patient identifiable data were required for this study and no additional data were collected. Therefore, no additional ethical approval for this analysis was sought.
Results
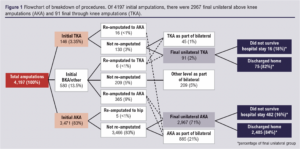
There were 4,197 AKA or TKA surgeries performed as a primary (86%) or re-amputation (9%) procedure in Scotland between 1 January 2007 and 31 December 2017 (Figure 1). A total of 3,471 (83%) initial AKAs and 146 (3.5%) initial TKAs were included. Of those, 25% (n=885) of the initial AKAs and 33% (n=46) of the initial TKAs were part of bilateral procedures. Excluding revisions to a higher level of amputation and those who did not survive their hospital stay, 2,485 people with AKA and 75 people with TKA were discharged from hospital.
Demographics
The majority of the study population were male (62%). The mean±SD population age was 69±13 years. The mean age for the AKA group was 69±13 years and for the TKA group was 67±15 years (p=0.058).
Co-morbidities
The TKA group were significantly more likely to have a diagnosis of diabetes (p=0.034) or were obese (p=0.009) (Table 2). Median FCI scores were 3 out of 18 and were the same between groups.

Aetiology
More than half of all amputations were due to peripheral arterial disease (PAD). Aetiology between groups was similar (Table 2). Other reasons for amputation included tumour, congenital deformity, blood-borne infection, renal disease, drug use and complex regional pain syndrome.
Centre
Over 50% of all TKAs were performed in three out of 21 possible centres; 11 centres performed the remaining procedures and seven centres did not perform any TKA. We classified the top three centres as ‘high volume’ centres and the other 11 as ‘low volume’ centres for comparison of surgical and rehabilitation outcomes.
Surgical outcomes
Further surgery
A higher proportion of patients required further surgery following TKA than following AKA (13% (19/146) vs 4% (151/3471), p<0.001). Of these, 2% of each group (57 AKA, 3 TKA) had further surgery involving only soft tissue (p=0.734). 3% (94) of AKA patients and 11% (16) of TKA patients had revision involving bone, including some which were reclassified as a higher level of amputation (p<0.001). Only 8% of TKA patients from high volume centres required further surgery compared with 19% in low volume centres (p=0.048). Having a second surgery was not associated with mortality for TKA (p=0.308) or AKA (p=0.105).
Length of stay
Despite more TKA patients than AKA patients requiring further surgery, their inpatient length of stay (LOS) was similar (35 (17–72) vs 42 (20–78) days, p=0.696).
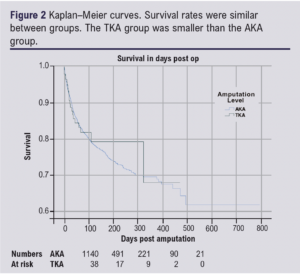
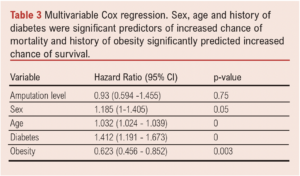
Survival
The proportion of patients dying during their hospital admission was similar (18% AKA vs 16% TKA, p=0.870). Survival was also similar between the two groups (log-rank p=0.809) (Figure 2). In the multivariable Cox regression, sex, age and history of diabetes were significant predictors of increased chance of mortality, and history of obesity significantly predicted increased chance of survival (Table 3).
Rehabilitation outcomes
Limb fitting
Limb fitting outcomes were similar between those with TKA and AKA (Figure 3). Those classed as ‘abandoned’ commenced prosthetic rehabilitation but did not achieve independent mobility with their prosthesis. Those ‘not limb fitted’ were not referred for prosthetic rehabilitation. Only 12% (9/77) of people with TKA from high volume centres were limb fitted compared with 25% (17/69) from low volume centres (p=0.041).
Compression therapy
The median number of days between operation date and commencing compression therapy was similar between the groups (TKA 10 (7–25) vs AKA (13 (7–26), p=0.485). Shrinker socks were the most common method of compression therapy used in all centres; 82% of those with an AKA used shrinker socks as their method of compression therapy compared with only 54% of those with a TKA; 21% used the Post Pneumatic Amputee Mobility Aid (PPAM aid), 18% used a rigid dressing and 7% used an elastic bandage.
Early walking aids
Time to start early walking aids was similar in the TKA and AKA groups (22 and 21 days; p=0.426). The TKA group favoured the PPAM aid (89%) over the Femurett (11%) for early walking aid, whereas 59% of the AKA group used the PPAM aid and 41% the Femurett.
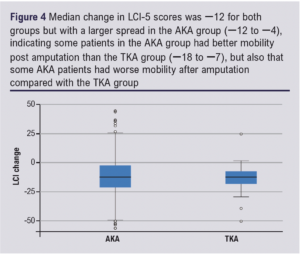
Locomotor Capabilities Index-5
The Locomotor Capabilities Index-5 (LCI-5) was completed retrospectively for the patient’s mobility six months prior to their amputation and prospectively on final discharge from prosthetic rehabilitation. The difference between these two scores gives a score for their change in mobility; a positive score indicates an improvement and a negative score deterioration. The change scores for both groups are shown in Figure 4.
Prosthesis
The median number of days from amputation to being cast for a prosthetic limb was the same for both groups (55 days). Days from casting to receiving the finished prosthetic limb were also similar: 14 (8–21) days for those with AKA and 12 (6–16) days for those with TKA (p=0.084).
For the 23 patients with TKA who limb fitted, it took 99 days (5–207) from inpatient discharge to complete prosthetic rehabilitation. The 725 patients with AKA who limb fitted took 133 (45–230) days (p=0.609).
Discussion
This retrospective study examined demographics and outcomes from all patients who underwent TKA or AKA over an 11-year period in Scotland. Baseline characteristics (age, gender and rates of PAD and diabetes) were comparable to similar studies.16–18 Similarities were observed between groups in the current study for survival, inpatient length of stay, limb fitting rates, mobility scores, and time to complete prosthetic rehabilitation, but reoperation rates in the TKA group were significantly higher.
The rates of reoperation post TKA in the current study are lower than those reported in older studies (34% and 29.9%, respectively).14,20 Furthermore, this study showed that high volume centres obtain much better results, suggesting there is scope for optimisation of patient selection, operative technique and/or perioperative care.
Limb fitting rates were lower in the current study than those reported in similar studies, and were particularly low in high volume centres.17,18 This may suggest that TKA is being chosen for patients not expected to mobilise, but this cannot be determined from these data. Nijmeijer et al and Ten Duis et al reported limb fitting rates of 61% and 59%, respectively, in their TKA groups; however, only 34% and 35% of those actually achieved household mobility with their prosthesis.17,18 The SPARG dataset only includes data up to the point of discharge from rehabilitation, therefore information regarding long-term prosthetic limb use at home is unavailable. It is known that up to 50% of people with AKA who limb fit stop using their prosthesis within the first year.24-26 The reduced energy requirements27 and superior socket comfort from a TKA prosthesis have the potential to improve long-term maintenance of prosthetic mobility. Further research is required to investigate this potential. As well as potentials in prosthetic rehabilitation, it has been claimed that TKA offers advantages for non-prosthetic rehabilitation including sitting balance and ability to transfer.28 The longer lever of a TKA can, in theory, provide a more stable sitting platform, and be used as a lever and/or weight-bearing surface for standing and transferring, but these claims have not been formally tested.
The British Society of Rehabilitation Medicine (BSRM) guidelines recommend TKA for patients with existing contralateral amputation to improve bed mobility, transfer ability and leave the patient with a lap to help with carrying objects when in a wheelchair.11 Despite this, 494 analysed patients underwent AKA for their second amputation compared with only 35 receiving TKA. These data suggest that considerable numbers of patients undergoing bilateral amputation are potentially missing out on significant advantages offered by TKA. The numbers of bilateral cases with one or two TKAs were too small to compare rehabilitation outcomes in this study. Inderbitzi et al compared outcomes of bilateral patients at different levels.29 They found the higher the amputation level the worse the rehabilitation outcome and concluded that, despite the high revision rates they observed in their TKA cohort, they would still advise amputation at the most distal point possible to improve rehabilitation outcomes.
A limitation of this study is its retrospective cohort design. Missing data and unknown confounders are faults with any retrospective study; however, a strength is that the SPARG dataset was used. The dataset exists for research purposes, so efforts are made to ensure there is very little missing data (reported to be less than 3%).
Another consideration is that variations of TKA such as Gritti–Stokes are included in the TKA group, so their outcomes cannot be analysed separately. It is unknown which type of TKA is best, with several being described in the literature.28,30-34 With so many techniques to choose from, surgeons may be more likely to opt for familiar AKA. Amputation surgery should only be performed by suitably experienced surgeons to ensure a good quality residuum.35,36 As such small numbers of TKA are being performed, training may be an issue which limits increased utilisation of TKA. Recently, a classification system has been created to describe different types of TKA which will improve future reporting of the variations of the operation.34
Murakami and Murray suggest that high reoperation rates post TKA are due to poor patient selection and a lack of physiological measures used to decide the level of amputation.28 The absence of defined selection criteria for each level of amputation is another limitation of this retrospective study.
Comparing TKA with AKA has always been challenging due to sample size differences. Even using 11 years of data, only 146 initial TKAs were available for analysis. Of these, only 23 were fitted with a prosthesis, making comparisons of rehabilitation outcomes difficult.
Prospective randomised studies are urgently needed to inform clinical practice with regard to deciding between TKA and AKA.
Conclusion
This study shows that TKA remains an underused option for major lower limb amputation. High volume centres have better surgical outcomes but appear to select patients not likely to limb fit. Despite this, similar proportions of patients did subsequently limb fit between groups, which may suggest superior rehabilitation potential for TKA compared with AKA. Details of current practice and level selection need investigation to determine how best to select patients who would benefit from TKA as opposed to AKA, but with a low risk of need for reoperation. Prospective randomised studies are urgently needed to inform clinical practice.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2023;2(4)208-214
Publication date:
July 5, 2023
Author Affiliations:
1. Academic Vascular Surgical Unit, Hull York Medical School, Hull, UK
2. Hull University Teaching Hospitals NHS Trust, Hull, UK
3. Scottish Physiotherapy Amputee Research Group, WestMARC, Queen Elizabeth University Hospital, Glasgow, UK
4. ICAHR, Hull York Medical School, University of Hull, Hull, UK
Corresponding author:
Hayley Gordon
Academic Vascular Surgical Unit, Hull University Teaching
Hospitals NHS Trust, Hull,
HU3 2JZ, UK
Email: [email protected]











