EDITORIALS
Models of same-day emergency care for vascular limb salvage
Sivaharan A,1 Brooks M,2 Bevis P,2 Day J,2 Davies RSM,3 Sayers RD,3 Sandford B4
Introduction
The efficient and effective management of patients with chronic limb-threatening ischaemia (CLTI) is a challenge for UK vascular services, due to the volume and complexity of patients and centralisation of services.1,2 In an attempt to provide comprehensive limb salvage services in keeping with the global vascular guidelines,3 more than 14,000 revascularisation procedures are performed in the NHS every year.4 Despite our best efforts, outcomes (amputation and mortality) for these patients remain relatively poor, and may be related to delays in revascularisation.5
The recent Vascular Society of Great Britain and Ireland (VSGBI) Peripheral Arterial Disease Quality Improvement Framework (PADQIF) recommends intervention for CLTI within five days for inpatients and 14 days for ambulatory outpatients.6 In an attempt to achieve these targets, certain UK centres have established emergency vascular or “hot” clinics. These one-stop clinics incorporate full clinical assessment of patients with CLTI with consultant review, supported by laboratory and imaging facilities. This facilitates multidisciplinary discussion prior to intervention and may prevent unnecessary hospital admission.
The challenges of establishing and managing these “hot” clinics may minimised by the knowledge and experience of those who have already been through this process.
Hot clinics in other specialities
Broadly speaking, hot clinics facilitate the rapid outpatient assessment and management of those urgent presentations which are not urgent enough to trigger admission. There is often variation in specific staffing, available investigation modalities and management pathways, depending on the speciality or available resources.
Trauma (plastics and orthopaedics)
Both plastic surgery and orthopaedics have a long history of using the hot clinic model to manage minor trauma. This approach helps to improve patient flow, reducing lengthy waiting times in the emergency department. In hand trauma, hot clinics and hot emergency operating lists can reduce waiting times and length of stay and they save the department approximately £1,000/day.7
General surgery
The diversity and severity of presentations of acute vascular patients are perhaps more reminiscent of the acute general surgical than the minor trauma population. Despite this challenge, general surgery has increased the use of ambulatory clinics for the assessment and management of non-critical abdominal pain. Observational studies suggest a large reduction in unnecessary admissions and increased patient satisfaction.8 Indeed, this approach has been so successful that most emergency general surgical services utilise some form of Same Day Emergency Care (SDEC) service.
Care of the elderly
With particular relevance to vascular surgery, the development of an acute frailty service is part of the NHS long term plan (2019), which aims to provide multidisciplinary comprehensive geriatric assessments (CGA) in acute medical services.9 These services, often an acute outreach service rather than a true hot clinic, share our speciality’s objectives of avoiding unnecessary admission, and may reduce mortality and improve quality of life.10-12
Hot clinics in vascular surgery
Several UK vascular units have introduced hot clinics in recent years, in response to the increasing CLTI workload, poor patient pathways and long inpatient waits for urgent care. However, as of 2021, fewer than half of vascular units utilised hot clinics for urgent assessment of patients with CLTI,13 even though they were recommended in the 2019 Global Vascular Guidelines.3 Ambulatory pathways can reduce inpatient stay, particularly in the pre-operative period, with subsequent reduction in deconditioning and opportunity for prevention of functional decline. The benefits to patients are complemented by economic efficiencies and therefore NHS Trusts are generally supportive of these initiatives.
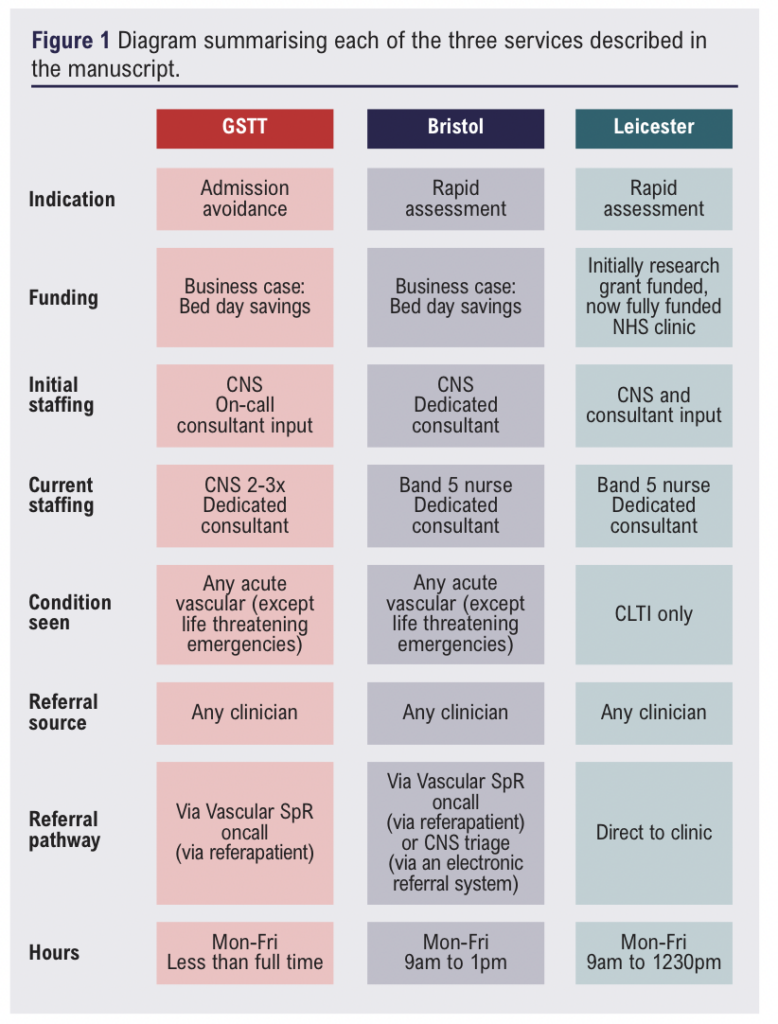
Presented are three UK examples of early adopters, whose ambulatory emergency care model has undergone iterative changes with growing experience. The benefits and challenges in each example are discussed, recognising that many other excellent models exist. Sharing learning points may help to meet the challenges of UK vascular service provision and plan future models of care. Figure 1 provides a summary of the three services.
Bristol
This service was designed as a Clinical Nurse Specialist (CNS)-led, consultant-supported service to reduce unnecessary admissions. The business case was based on admission avoidance and bed day cost savings. The service, which started in 2014, reviews patients with any suspected acute vascular diagnosis, excepting life- or limb-threatening emergencies, within 48 hours of referral. The clinic is staffed by a CNS and supported by the on-call consultant, with duplex ultrasound (DUS) availability. It runs during weekday mornings. Referrals are accepted from any doctor in primary or secondary care and are reviewed on a case-by-case basis to determine their suitability for hot clinic review and the timeframe.
Although the initial model utilised both CNS and consultant expertise, over time this staffing model has been revised. It now includes a band 5 and a band 3 nurse to support a consultant-delivered service, in order to avoid skill-set duplication and to free CNS expertise to support other service areas.
Model-specific successes include support from a dedicated clinical vascular scientist, and additional clinic room availability to ensure maximal service efficiency. Same-day pre-assessment appointments to facilitate rapid access to operating slots following clinic review have also proved invaluable. Additional band 3 nurse training has extended the role to completing ankle and toe brachial pressure index (ABPI and TBPI) assessments.
In this setting, there was a trial of utilising the hot clinic for follow-up appointments when other clinics were overbooked. This was found to be an inappropriate use of resources and was stopped.
Guy’s and St Thomas’ (GSTT)
The emergency vascular clinic (EVC) at GSTT was established to reduce unnecessary admissions for urgent but non-emergency presentations, incorporating CLTI, symptomatic carotid stenosis, iliofemoral deep venous thrombosis (DVT) and embolic presentations. The clinic is CNS-led with support from a consultant vascular surgeon, offering DUS and cross-sectional imaging (computed tomography angiography [CTA] and magnetic resonance venography [MRV]). The service has been demonstrated to be a safe and efficient pathway, avoiding unnecessary admissions.14 The original model, developed as a pilot, utilised a seconded senior vascular ward nurse (Band 6). This required investment in training, with both the advanced assessment skills course and non-medical prescriber courses being undertaken to support the CNS-led role in the service.
Referrals were taken by the registrar on call and triaged as being appropriate for EVC review. The CNS undertook initial assessment, blood tests and organised imaging, and following review by the on-call consultant of the week, an ongoing management plan was made. In ambulatory cases, the CNS assisted with multidisciplinary team (MDT) referral and admission planning. Additionally, a prospective database was maintained to ensure no patient was ‘lost’ in the system.
This service was deemed safe and both clinically effective and cost-effective. A successful three-year business plan application guaranteed that the service continued and expanded. Early challenges included variability in the availability of the consultant of the week to review patients, resulting in occasional long patient delays or discharge without a clearly defined management plan. In response to this, and during COVID when the clinic was both very busy and physically remote from the arterial hub site, a dedicated rotating EVC consultant was introduced. This system has remained, and the CNS numbers have been expanded to facilitate a training rotation for less experienced CNS staff. In addition, administrative support has been provided to assist in the booking of appointments and uploading relevant referral information to the electronic patient record in advance of the patient attendance. A band 3 health care assistant with an enhanced role including phlebotomy has been added to the team.
The current model is largely based on a CNS-led clinic for the assessment of urgent patients and expedited post-operative review to facilitate early discharge, with consultant review for decision making, definitive planning and ‘ownership’ of patients, which has been identified as a key component of care.
Leicester
The Leicester vascular limb salvage (VaLS) clinic model was established to address delays in the management of patients presenting to their community healthcare teams with suspected CLTI. It was initially funded through a philanthropic clinical research donation and, following its successful trial, is now a fully funded NHS clinic. The clinic focuses on suspected CLTI and accepts referrals from all sources, with no specific inclusion or exclusion criteria. Other vascular pathologies are not routinely reviewed in this clinic. Initially the clinic was designed as a nurse-led clinic with consultant oversight to see only new CLTI patients. However, over time, due to service demands, it has evolved into a consultant-delivered service with nursing support, with additional capacity allowing early post-operative review following revascularisation. The clinic runs every weekday morning, can accommodate 10 patients per clinic, and is supported by a dedicated clinical vascular scientist. Uniquely, in addition to ring-fenced outpatient scanning facilities for cross-sectional imaging, this service has dedicated angiography and hybrid theatre slots available to ensure timely intervention in the case of confirmed CLTI. The Leicester VaLS model is associated with improved freedom from major amputation.15
Challenges
The CLTI patient population present unique challenges. The triple threat of frailty, multimorbidity and polypharmacy raises some specific issues in ambulatory services. Many patients will require multiple medications to be dispensed during their time in the hot clinic, including analgesia, diabetic medications, anticoagulation and hydration (especially around CT angiograms), and the nature of CLTI often has implications for mobility and transport.
The PADQIF targets for CLTI necessitate prompt MDT discussion and revascularisation. Daily “mini” MDTs to ensure timely discussion and decision-making have been introduced in some centres. Revascularisation challenges include appropriate list, environment and skill set availability. Ring fencing specific lists for hot clinic patients reduces overall capacity for vascular inpatients. A common question in daily vascular practice is whether inpatients should receive operative priority over ambulatory patients. Although a hot clinic helps with assessment and planning, implementing the management plan still poses significant challenges. The ever-evolving sub-specialisation of services and expansion in the range of technologies and techniques available to treat complex disease also pose a challenge to scheduling patients rapidly, adding an additional dimension of matching the patient to the physical environment (open, hybrid or endovascular suite) and skill mix of the surgical team required to offer optimal care. This is a challenge which also presents opportunities for teams to embrace closer collaboration with colleagues and ongoing professional development in this context. However, this requires the support of senior decision-makers within a Trust.
The hub and spoke model presents specific challenges and frequently results in inequality in patients’ access to vascular services, with spoke CLTI patients experiencing longer peri-operative journeys. This situation may be exacerbated by hosting the emergency vascular services in a hub site. Potential solutions include spoke hot clinics, scan support for diabetic foot clinics, and reserved hot slots in routine vascular clinics with rapid access to imaging.
The future
Virtual clinics
Trauma and orthopaedics have successfully implemented virtual hot clinics.16,17 Virtual vascular surgery hot clinics incorporating video or photographs would minimise patient transport and associated environmental costs and perhaps alleviate some spoke/community podiatry support challenges. This might, however, increase workload as virtual appointments are often easier to obtain and may require more time and digital functionality.
Post-revascularisation care
The post-discharge management of CLTI patients following revascularisation is often complex, and complications are not uncommon. Hot clinics have the potential to support this care, similar to how general surgery same day emergency clinics (SDECs) are often used, but it would require a rapid expansion of staff and funding. This is currently being trialled in Leicester, using a parallel hot clinic to review urgent non-CLTI referrals (aneurysms and carotids) and undertake post-operative reviews. This is very much in an early phase, and it remains to be seen whether it provides enough utility to merit continued funding.
The approach of expedited discharge, with heavy community support, has been trialled in post-stroke care.18 It is unclear whether this type of post-operative outpatient service would be cost-effective by reducing inpatient stays in vascular surgery, especially given the expense of establishing such a service.
Complex geriatric assessment and anaesthetic input
A geriatric / anaesthetic assessment service embedded within the hot clinic itself may be a useful addition to current service models. This would facilitate same-day CGA, expedite and direct investigations and would holistically inform decision-making.
Same-day treatment
Despite the complexity of vascular patients and interventions for CLTI, the increasing use of endovascular surgery has provided the option of day-case angioplasties. This provides a completely ambulatory treatment pathway for carefully selected patients with CLTI. These day case pathways must be carefully developed to select appropriate patients and manage potential complications safely but may avoid admission completely.
Conclusion
Hot clinics have the potential to improve urgent access to acute vascular services. Inherent in the success of such services is a reliable pathway to rapid and efficient assessment, investigations, decision-making and intervention. Such models are likely to have a positive effect on time to revascularisation, major lower limb amputation and mortality.
Article DOI:
Journal Reference:
J.Vasc.Soc.G.B.Irel. 2025;4(2):60-63
Publication date:
February 27, 2025
Author Affiliations:
1. Northern Vascular Centre, Freeman Hospital, Freeman Rd, High Heaton, Newcastle upon Tyne, NE7 7DN, UK
2. Department of Vascular Surgery, North Bristol NHS Trust, Bristol, UK
3. The Department of Vascular Surgery, Leicester Royal Infirmary, Leicester, UK
4. Guy’s and St Thomas’ NHS Foundation Trust, St Thomas’ Hospital, Westminster Bridge Road, London, SE1 7EH, UK
Corresponding author:
Ashwin Sivaharan
Northern Vascular Centre, Freeman Hospital, Freeman Rd, High Heaton, Newcastle upon Tyne, NE7 7DN, UK
Email: [email protected]











